This section includes the diagnostic modalities (imaging and laboratory tests) and algorithms useful to diagnose the following 145 diseases and disorders. It is assumed that the patient has had a detailed history and physical examination before any testing sequence is initiated.
These algorithms are designed to assist clinicians in the evaluation and treatment of patients. They may not apply to all patients with a particular disease or disorder, and they are not intended to replace a clinician’s individual judgment. Please note that specific findings in the patient’s history and physical examination may significantly alter any of the proposed testing sequences.
- 1.
Abdominal abscess
- 2.
Abdominal aortic aneurysm
- 3.
Achalasia
- 4.
Acid-base disorders
- 5.
Acute kidney injury
- 6.
Addison’s disease (adrenal insufficiency)
- 7.
Adrenal mass
- 8.
Alkaline phosphatase elevation
- 9.
ALT/AST elevation
- 10.
Amenorrhea, primary
- 11.
Amenorrhea, secondary
- 12.
Anemia, macrocytic
- 13.
Anemia, microcytic
- 14.
Antinuclear antibody (ANA)–positive
- 15.
Aortic dissection
- 16.
Appendicitis
- 17.
Ascites
- 18.
Avascular necrosis
- 19.
Back pain, acute, lumbosacral (LS) area
- 20.
Bilirubin elevation
- 21.
Bleeding disorder, congenital
- 22.
Brain abscess
- 23.
Breast mass
- 24.
Carcinoid syndrome
- 25.
Cardiomegaly on chest radiograph
- 26.
Cholangitis
- 27.
Cholecystitis
- 28.
Cholelithiasis
- 29.
Complex regional pain syndrome (reflex sympathetic dystrophy [RSD])
- 30.
Constipation
- 31.
Creatinine phosphokinase (CPK) elevation
- 32.
Cushing’s syndrome
- 33.
Deep vein thrombosis (DVT)
- 34.
Delayed puberty
- 35.
Delirium
- 36.
Diarrhea
- 37.
Disseminated intravascular coagulation (DIC)
- 38.
Diverticulitis
- 39.
Dyspepsia
- 40.
Dyspnea
- 41.
Dysuria
- 42.
Ectopic pregnancy
- 43.
Edema, lower extremity
- 44.
Endocarditis, infective
- 45.
Endometriosis
- 46.
Epiglottitis
- 47.
Fatigue
- 48.
Fever of undetermined origin (FUO)
- 49.
Galactorrhea
- 50.
Genital lesions/ulcers
- 51.
Goiter
- 52.
Granulomatosis with polyangiitis
- 53.
Gynecomastia
- 54.
Hearing loss
- 55.
Hematochezia
- 56.
Hematuria
- 57.
Hemochromatosis
- 58.
Hemoptysis
- 59.
Hepatomegaly
- 60.
Hirsutism
- 61.
Hyperaldosteronism
- 62.
Hypercalcemia
- 63.
Hyperkalemia
- 64.
Hypermagnesemia
- 65.
Hypernatremia
- 66.
Hyperphosphatemia
- 67.
Hyperthyroidism
- 68.
Hypocalcemia
- 69.
Hypoglycemia
- 70.
Hypogonadism
- 71.
Hypokalemia
- 72.
Hypomagnesemia
- 73.
Hyponatremia
- 74.
Hypophosphatemia
- 75.
Hypothyroidism
- 76.
Immunodeficiency
- 77.
Infertility
- 78.
Jaundice
- 79.
Joint effusion
- 80.
Liver function test elevations
- 81.
Liver mass
- 82.
Lymphadenopathy, generalized
- 83.
Malabsorption, suspected
- 84.
Meningioma
- 85.
Mesenteric ischemia
- 86.
Mesothelioma
- 87.
Metabolic acidosis
- 88.
Metabolic alkalosis
- 89.
Microcytosis
- 90.
Multiple myeloma
- 91.
Multiple sclerosis
- 92.
Myalgias
- 93.
Muscle weakness
- 94.
Neck mass
- 95.
Neuropathy
- 96.
Neutropenia
- 97.
Osteomyelitis
- 98.
Pancreatic mass
- 99.
Pancreatitis, acute
- 100.
Parapharyngeal abscess
- 101.
Pelvic mass
- 102.
Peripheral arterial disease (PAD)
- 103.
Pheochromocytoma
- 104.
Pituitary adenoma
- 105.
Pleural effusion
- 106.
Polyarteritis nodosa
- 107.
Polycythemia
- 108.
Portal vein thrombosis
- 109.
Precocious puberty
- 110.
Proteinuria
- 111.
Pruritus, generalized
- 112.
Pulmonary embolism
- 113.
Pulmonary hypertension
- 114.
Pulmonary nodule
- 115.
Purpura
- 116.
Renal artery stenosis
- 117.
Renal mass
- 118.
Rotator cuff tear
- 119.
Sarcoidosis
- 120.
Scrotal mass
- 121.
Small-bowel obstruction
- 122.
Spinal epidural abscess
- 123.
Splenomegaly
- 124.
Stroke
- 125.
Subarachnoid hemorrhage
- 126.
Subclavian steal syndrome
- 127.
Subdural hematoma
- 128.
Superior vena cava syndrome
- 129.
Syncope
- 130.
Testicular torsion
- 131.
Thoracic outlet syndrome
- 132.
Thrombocytopenia
- 133.
Thrombocytosis
- 134.
Thyroid nodule
- 135.
Thyroiditis
- 136.
Tinnitus
- 137.
Transient ischemic attack (TIA)
- 138.
Urethral discharge
- 139.
Urolithiasis
- 140.
Urticaria
- 141.
Vaginal discharge
- 142.
Vertigo
- 143.
Viral hepatitis
- 144.
Weight gain
- 145.
Weight loss, involuntary
Acronyms
A-a: alveolar-arterial
AAA: abdominal aortic aneurysm
Ab: antibody
ABG: arterial blood gas
ABI: ankle brachial index
ACE: angiotensin-converting enzyme
ACTH: adrenocorticotropic hormone
ADA: adenosine deaminase
AFB: acid-fast bacteria
ALT: alanine aminotransferase
AMA: antimitochondrial antibody
AMP: adenosine monophosphate
ANA: antinuclear antibody
ASMA: anti–smooth muscle antibody
AST: aspartate aminotransferase
BNP: B-type natriuretic peptide
BUN: blood urea nitrogen
c-ANCA: cytoplasmic antineutrophil cytoplasmic antibodies
CBC: complete blood cell
CDI: Clostridium difficile infection
CHF: congestive heart failure
CMV: cytomegalovirus
CPK: creatinine phosphokinase
C&S: culture and sensitivity
CSF: cerebrospinal fluid
CT: computed tomography
DHEAS: dehydroepiandrosterone sulfate
DIC: disseminated intravascular coagulation
DNA: deoxyribonucleic acid
Ds: double strand
DS: dehydroepiandrosterone
DVT: deep vein thrombosis
EB: Epstein-Barr
ECG: electrocardiogram
ECM: erythema chronicum migrans
ELISA: enzyme-linked immunosorbent assay
EMG: electromyogram
EPS: electrophysiologic
ERCP: endoscopic retrograde cholangiopancreatography
ESR: erythrocyte sedimentation rate
EUS: endoscopy ultrasound
FBS: fasting blood sugar
FENa: fractional excretion of sodium
FNAB: fine-needle aspiration biopsy
FSH: follicle-stimulating hormone
FUO: fever of undetermined origin
GB: gallbladder
GFR: glomerular filtration rate
GGT: γ-glutamyl transferase
GGTP: γ-glutamyl transpeptidase
GnRH: gonadotropin-releasing hormone
HBsAg: hepatitis B surface antigen
hCG: human chorionic gonadotropin
HCV: hepatitis C virus
HIV: human immunodeficiency virus
HSV: herpes simplex virus
IEP: immunoelectrophoresis
Ig: immunoglobulin
IGF: insulin-like growth factor
INR: International Normalized Ratio
IV: intravenous
IVP: intravenous pyelogram
K: potassium
KOH: potassium hydroxide
LDH: lactate dehydrogenase
LGV: lymphogranuloma venereum
LH: luteinizing hormone
LKM: liver kidney microsomal
LS: lumbosacral
LP: lumbar puncture
Na: sodium
MIBG: metaiodobenzylguanidine
MRA: magnetic resonance angiogram
MRCP: magnetic resonance cholangiopancreatography
MRDTI: magnetic resonance direct thrombus imaging
MRI: magnetic resonance imaging
OHP: hydroxyprogesterone
O&P: orthotic and prosthetic
OR: operating room
PA: posteroanterior
PAC: plasma aldosterone concentration
p-ANCA: perinuclear antineutrophil cytoplasmic antibody
PCOS: polycystic ovary syndrome
PCR: polymerase chain reaction
PCreat: plasma creatinine
PE: pulmonary embolism
PET: positron emission tomography
PFA: platelet function analysis
PNa: plasma sodium
PPD: purified protein derivative
PRA: plasma renin activity
PSA: prostate-specific antigen
PT: prothrombin time
PTH: parathyroid hormone
PTT: partial thromboplastin time
RAIU: radioactive iodine uptake
RBC: red blood cell
RDW: red blood cell distribution width
RF: rheumatoid factor
RNP: ribonucleoprotein
r/o: rule out
RSD: reflex sympathetic dystrophy
SBE: subacute bacterial endocarditis
TB: tuberculosis
Tc: technetium
TEE: transesophageal echocardiogram
TIA: transient ischemic attack
TIBC: total iron-binding capacity
TRH: thyrotropin-releasing hormone
TSH: thyroid-stimulating hormone
TT: thrombin time
TTKG: transtubular potassium gradient
UGI: upper gastrointestinal
UCreat: urine creatinine
UNa: urine sodium
UOsmo: urine osmolarity
VDRL: venereal disease research laboratories
V/Q: ventilation-perfusion
WBC: white blood cell
1
Abdominal Abscess ( Fig. 3.1 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

2
Abdominal Aortic Aneurysm ( Fig. 3.3 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

3
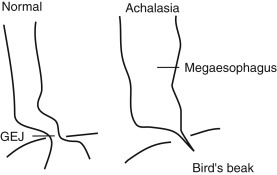
Achalasia ( Fig. 3.5 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

4
Acid-Base Disorders ( Figs. 3.8 and 3.9 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|


5
Acute Kidney Injury ( Fig. 3.10 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

6
Addison Disease (Adrenal Insufficiency) ( Fig. 3.11 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

7
Adrenal Mass ( Fig. 3.12 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

8
Alkaline Phosphatase Elevation ( Fig. 3.14 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

9
ALT/AST Elevation ( Fig. 3.15 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

10
Amenorrhea, Primary ( Fig. 3.16 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

11
Amenorrhea, Secondary ( Fig. 3.17 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

12
Anemia, Macrocytic ( Fig. 3.18 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

13
Anemia, Microcytic ( Fig. 3.19 )
| Diagnostic Imaging | Laboratory Evaluation ( Table 3.1 ) |
|---|---|
Best Test(s)
| Best Test(s)
|

| Abnormality | Ferritin | Serum IRON | TIBC | RDW |
|---|---|---|---|---|
| Iron deficiency | ↓ | ↓ | ↑ | ↑ |
| Inflammatory anemia | N/↑ | ↓ | ↓ | N |
| Sideroblastic anemia | N/↑ | ↑ | N | N |
| Thalassemia | N/↑ | N/↑ | N/↓ | N/↑ |
14
Antinuclear Antibody (ANA)–Positive ( Fig. 3.20 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

- 1.
Systemic lupus erythematosus. Multiple ANAs are frequently seen in systemic lupus erythematosus, often with high levels of anti-dsDNA and antinucleosome antibodies in active disease, together with low complement fractions and high novel biomarker levels, like SIGLEC-1. Distinctiveness of anti-Sm, anti-rRNP, anti-C1q, antinucleosomes, and anti-PCNA.
- 2.
Drug-induced lupus. Restriction of ANAs to antihistone and/or antinucleosome antibodies.
- 3.
MCTD. Restriction of ANA to U1nRNP (by disease definition).
- 4.
Sjögren’s syndrome. Characterized primarily by the presence of antibodies to SS-A/Ro and SS-B/La.
- 5.
Systemic sclerosis. Profile consisting of antibodies to Scl-70/topo I, the centromere/kinetochore antigens, anti-RNA polymerases, and other nucleolar antigens such as fibrillarin and Th/To.
- 6.
Rheumatoid arthritis. Frequent presence of rheumatoid factor and anticitrullinated proteins (AKA, APF, anti-CCP).
- 7.
PM/DM. Presence of Jo-1, Mi-2, and PM-Scl autoantibodies.
- 8.
Undifferentiated connective tissue diseases. Autoantibodies, such as anticentromeres, anti-CCP, and anti-dsDNA, may antedate overt clinical disease by many years.
MCTD, mixed connective tissue disease; PM/DM, polymyositis/dermatomyositis.
15
Aortic Dissection ( Fig. 3.21 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|


16
Appendicitis ( Fig. 3.25 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

17
Ascites ( Fig. 3.27 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

| Condition | Serum-Ascites Albumin Gradient ∗ | Ascites Total Protein Level † |
|---|---|---|
| Cirrhosis | High | Low |
| Malignant ascites | Low | High |
| Cardiac ascites | High | High |
∗ High is greater than 1.1 g/dL; low is less than 1.1 g/dL.
| Biology | Appearance | Total Protein (g/dL) | LDH (IU) | Specific Gravity | Glucose (mg/dL) | WBCs/mm 3 | RBCs/MM 3 | Amylase |
|---|---|---|---|---|---|---|---|---|
| Neoplasm | Bloody Clear Chylous | >2.0 | >200 | Variable | <60 | ↑ | ↑↑ | |
| Cirrhosis | Straw colored | <2.5 | <200 | <1.016 | <60 | ↓ | ↓ | |
| Nephrosis | Straw colored | <2.5 | <200 | <1.016 | >60 | ↓ | ↓ | |
| CHF | Straw colored | <2.5 | <200 | <1.016 | >60 | ↓ | ↓ | |
| Pyogenic | Turbid | >2.5 | >200 | >1.016 | >60 | ↑↑ PMNs | ↓ | |
| Pancreatic | Hemorrhagic Turbid Chylous | >2.5 | >200 | Variable | >60 | Variable | Variable | ↑↑ |
18
Avascular Necrosis ( Fig. 3.29 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

19
Back Pain, Acute, Lumbosacral (LS) Area ( Fig. 3.31 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

20
Bilirubin Elevation ( Fig. 3.32 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

21
Bleeding Disorder, Congenital ( Fig. 3.33 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

22
Brain Abscess ( Fig. 3.34 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

23
Breast Mass ( Fig. 3.36 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

24
Carcinoid Syndrome ( Fig. 3.39 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

25
Cardiomegaly on Chest Radiograph ( Fig. 3.41 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|


26
Cholangitis ( Fig. 3.44 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

27
Cholecystitis ( Fig. 3.46 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

28
Cholelithiasis ( Fig. 3.49 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

29
Complex Regional Pain Syndrome (Reflex Sympathetic Dystrophy [RSD]) ( Fig. 3.51 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

30
Constipation ( Fig. 3.53 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

31
Creatinine Phosphokinase (CPK) Elevation ( Fig. 3.54 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

32
Cushing’s Syndrome ( Fig. 3.56 , Table 3.4 )
| Diagnostic Imaging ∗ | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|
∗ Imaging studies are indicated only after biochemical documentation of hypercortisolism.

| Etiology | Overnight Dexamethasone Suppression Test | Plasma ACTH | Low-Dose Dexamethasone | High-Dose Dexamethasone | Corticotropin-Releasing Hormone Stimulation of Acth | Petrosal-to-Peripheral Acth Ratio |
|---|---|---|---|---|---|---|
| Normal | Suppression | Normal | Suppression | Normal | ||
| Pituitary | No suppression | Normal or high | No suppression | Suppression | Normal or increased | >2 |
| Ectopic | No suppression | High or normal | No suppression | No suppression | No response | <1.5 |
| Adrenal | No suppression | Low | No suppression | No suppression | No response |
∗ Classic responses are indicated. Certain cases of ectopic ACTH production are suppressed by high-dose dexamethasone or are stimulated by corticotropin-releasing hormone. In these cases, petrosal sinus sampling is the most reliable method for distinguishing pituitary and ectopic sources of ACTH.
33
Deep Vein Thrombosis (DVT) ( Fig. 3.57 , Table 3.5 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

| SCORE | |
|---|---|
| Active cancer (treatment ongoing or within previous 6 months or palliative) | 1 |
| Paralysis, paresis, or recent plaster immobilization of the lower extremities | 1 |
| Recently bedridden >3 days or major surgery within 4 weeks | 1 |
| Localized tenderness along the distribution of the deep venous system | 1 |
| Entire leg swollen | 1 |
| Calf swelling >3 cm asymptomatic side (measured 10 cm below tibial tuberosity) | 1 |
| Pitting edema confined to the symptomatic leg | 1 |
| Collateral superficial veins (nonvaricose) | 1 |
| Alternative diagnosis as likely or greater than likelihood of DVT | −2 |
34
Delayed Puberty ( Fig. 3.59 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

35
Delirium ( Fig. 3.60 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

36
Diarrhea ( Fig. 3.61 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

37
Disseminated Intravascular Coagulation (DIC) ( Fig. 3.62 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

38
Diverticulitis ( Fig. 3.63 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

39
Dyspepsia ( Fig. 3.65 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

40
Dyspnea ( Fig. 3.66 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

41
Dysuria ( Fig. 3.67 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

42
Ectopic Pregnancy ( Fig. 3.68 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

43
Edema, Lower Extremity ( Fig. 3.71 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

44
Endocarditis, Infective ( Fig. 3.72 , Table 3.6 )
| Diagnostic Imaging | Laboratory Evaluation |
|---|---|
Best Test(s)
| Best Test(s)
|

| Major criteria |
|---|
| Positive blood cultures for infective endocarditis |
| Typical microorganism for infective endocarditis from two separate blood cultures in the absence of a primary focus: Streptococcus viridans, Streptococcus bovis |
| HACEK group: Haemophilus species, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, and Kingella kingae |
| Community-acquired Staphylococcus aureus or enterococci |
| Persistently positive blood cultures, defined as recovery of a microorganism consistent with infective endocarditis from blood cultures drawn more than 12 hours apart, or all of three, or the majority of four or more separate blood cultures, with the first and last drawn at least 1 hour apart |
| Single positive blood culture for Coxiella burnetii or antiphase IgG antibody titer >1:800 |
| Evidence for endocardial involvement |
| TTE (TEE in prosthetic valve) showing oscillating intracardiac mass on a valve or supporting structures, in the path of regurgitant jet or on implanted material, in the absence of an alternative anatomic explanation, or |
| Abscess, or |
| New partial dehiscence of a prosthetic valve |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree