Abstract
Purpose
To explore the efficacy of interventional ultrasound treatment for hoarseness caused by nondisconnected recurrent laryngeal nerve injury after thyroidectomy.
Materials and methods
In this retrospective study, we analysed the clinical data of 21 patients who underwent interventional ultrasound therapy (ultrasound-guided injection of a Diprospan and saline mixture) for postthyroidectomy hoarseness at our hospital between August 1, 2023, and January 31, 2024 (the Diprospan group) and randomly selected 21 patients who did not receive any treatment for postthyroidectomy hoarseness during the same period as the control group. The average vocal cord activity improvement time for the Diprospan group was calculated and compared with that of untreated patients from previous studies. Vocal cord activity improvement rates were assessed at 1, 2, and 3 mo after thyroidectomy, and changes in the voice handicap index (VHI) and the subjective listening perception scale (GRBAS) scores before and after treatment were evaluated. Additionally, the efficacy was compared between patients treated within 2 wk (timely intervention group, TI group) and those treated 2 wk after thyroidectomy (delayed intervention group, DI group) to explore the impact of treatment timing on outcomes.
Results
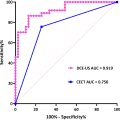
In the Diprospan group, the average vocal cord activity improvement time was 44.6 ± 4.7 d for those treated within 2 wk after thyroidectomy and 17.7 ± 1.5 d for those treated 2 wk after thyroidectomy, both of which were significantly shorter than the 6 mo to 1 y reported in the literature. The improvement rates at 1, 2, and 3 mo after thyroidectomy were significantly greater in the Diprospan group than in the control group (0.0% vs. 28.6%, 23.8% vs. 81.0%, 33.3% vs. 90.5%, p < 0.05). The VHI score (72.6 ± 21.2 vs. 12.6 ± 24.7, p < 0.001) and GRBAS score (12.0 vs. 0.0, p < 0.001) significantly improved after treatment. Compared with the DI group, the TI group also showed faster voice recovery (19.8 ± 5.8 d vs. 14.0 ± 2.6 d, p < 0.05). No treatment-related adverse reactions were observed.
Conclusion
Interventional ultrasound is a safe and effective treatment for hoarseness after thyroidectomy, as it effectively improves vocal cord mobility and accelerates voice recovery.
Introduction
Recurrent laryngeal nerve (RLN) dysfunction followin g thyroidectomy is the most common cause of postoperative hoarseness in patients, with an incidence rate of approximately 30%–80% [ ]. This hoarseness has a great impact on patients’ social life and work. Although careful intraoperative anatomical dissection and intraoperative monitoring of the RLN significantly reduce the likelihood of nerve damage, factors such as surgical traction, oedema, and local tissue adhesion can still lead to nerve swelling and functional impairment (RLN paralysis, RLNP). RLNP can be classified into temporary RLNP and permanent RLNP. The incidence of postoperative temporary RLNP is approximately 9.8%, and patients recover within 6–12 mo. However, if symptoms persist for more than 1 y, RLNP is considered permanent, with an incidence rate of approximately 2.3% [ ]. At present, there is still a lack of effective treatments for temporary RLNP, with conservative observation and voice therapy being the primary approaches. Conservative observation may delay the voice recovery time, and patients with temporary RLNP might miss the treatment window because of the presence of cicatricial tissue and effusion in the surgical area surrounding the RLN, which might lead to permanent RLNP. Although voice therapy can improve pronunciation, as a nonetiological treatment, it mainly improves glottis closing function through muscle adduction compensation, which may increase the risk for subsequent surgery of the head and neck. Voice therapy requires an average of 14 training courses [ ] lasting 1–3 mo, which is a long time commitment and requires high patient compliance.
Aetiological interventions for temporary RLNP are constantly being explored. The findings of a 2006 randomized controlled trial revealed that intravenous injection of 100 mg of hydrocortisone during surgery significantly reduced patient voice recovery time, from 40.5 d to 28.6 d [ ]. However, another randomized controlled trial revealed that preoperative intravenous injection of a 100 mL mixture of dexamethasone at a concentration of 8 mg/2 mL did not significantly improve patients’ subjective vocal ability [ ]. These conflicting results may be attributable to variations in drug dosage and the timing of treatment. We investigated the possibility of using glucocorticoids for the treatment of RLN oedema. The technique of ultrasound-guided local drug injection, which can ensure adequate local drug concentrations and curative effects and can reduce side effects caused by systemic medication, is becoming increasingly mature [ ]. Therefore, we hypothesize that local injection of glucocorticoids around the RLN in the oesophagotracheal groove under ultrasound guidance can reduce RLN oedema and accelerate neurological recovery.
The aim of this study was to preliminarily explore the safety and effectiveness of ultrasound-guided steroid injection treatment by calculating the average time to vocal cord activity improvement in the Diprospan group; compare improvement rates at 1, 2, and 3 mo after thyroidectomy between the Diprospan and control groups; and analyse voice quality changes and treatment timing efficacy. We aimed to determine whether this new treatment method is safe and effective.
Materials and methods
The data of 21 patients with postthyroidectomy hoarseness who received interventional ultrasound treatment and completed a 3-mo follow-up between August 1, 2023, and January 31, 2024 at the First Affiliated Hospital of Sun Yat-sen University was collected as the Diprospan group, and the data of 21 patients who did not receive any treatment and undergo only routine observation and follow-up was randomly selected from the same period at a ratio of 1:1 as the control group. The interventional ultrasound treatment for postthyroidectomy hoarseness, a novel IV-class technique, received approval from the Medical Technology Management Committee of Sun Yat-sen University First Affiliated Hospital in 2022. For this retrospective study, the ethical approval was approved by the Research Ethics Committee of Sun Yat-sen University First Affiliated Hospital in November 2023 ([2023] No. 696), and the informed consent was waived.
Study design and patients
The cases of patients in the Diprospan group and the control group were reviewed ( Fig. 1 ). The inclusion criteria were as follows: (i) underwent thyroidectomy for the first time and experienced postoperative hoarseness (changes in the patient’s voice quality, pitch, volume, or phonatory strength that impact daily communication [ ]); (ii) preoperative laryngoscopy revealed no vocal cord activity abnormality, confirmed by the surgeon intraoperatively as having no RLN transection injury, but postoperative laryngoscopy revealed abnormal vocal cord activity (indicating findings of vocal cord paralysis, including varying degrees of glottic incompetence and limitations in the adduction and abduction of the vocal cords, as observed through electronic laryngoscopy [ ]); and (iii) aged older than 18 y. The exclusion criteria were as follows: (i) previous history of neck radiation or surgery; (ii) presence of hoarseness before surgery or tumours invading the RLN; (iii) diagnosis of immune deficiency or receiving any form of immunosuppressive therapy within 2 wk; (4) allergy to glucocorticoids; (5) refusal to continue participation, demonstrated poor compliance, or did not follow the doctor’s instructions for treatment review; and (6) presence of severe mental illness (schizophrenia, bipolar disorder, uncontrollable anxiety or depression).

Patient preparation
The preoperative talk was complete, and the patient signed the surgical risk consent form prior to the procedure. The patient lay in a horizontal supine position, with a low pillow placed behind the neck to tilt the head and neck back to fully expose the surgical area of the neck.
Ultrasound equipment
An Anesus R9 ultrasonic diagnostic instrument (Mindray, Shenzhen, China) equipped with a linear array high-frequency probe (frequency 10–14 MHz) was used for ultrasound-guided steroid injection treatment.
Operation procedure
Before treatment, a basic ultrasound scan was performed, an appropriate amount of coupling agent was applied to the probe, and the probe was gently placed on the patient’s neck to ensure that the probe was in full contact with the skin. The ultrasound probe plane was parallel to the body surface and perpendicular to the long axis of the neck, scanning from top to bottom from the level of the hyoid bone to the level of the cricoid cartilage arch. Static images of transverse and longitudinal sections of the thyroid surgical area were collected, fluid accumulation or organized adhesion was observed, and subsequent treatment procedures were selected.
Interventional ultrasound treatment
① Disinfection and Draping: While wearing sterile gloves, the area should be disinfected routinely, and then, the high-frequency probe should be covered with a single-use sterile protector. ② Medication Preparation: Using a disposable sterile syringe (5 mL, 0.5 mm, Kinderai, Shanghai, China), 5 mL of Diprospan solution (a mixture of 1 mL of Diprospan (Compound Betamethasone Injection, Merck, Hangzhou, China) and 4 mL of normal saline) was drawn, and then several 5 mL disposable sterile syringes were prepared for the aspiration of accumulated fluid. ③ Injection of the dexamethasone mixture: The procedure is performed on the affected side of the patient. If ultrasound reveals fluid accumulation, it should be aspirated thoroughly ( Fig. 2 ). The ultrasound probe was positioned transversely to the neck, and the tracheoesophageal groove was visualized towards the affected side. The needle was inserted at the cricothyroid membrane level on the affected side, with a needle/probe distance of 0–0.5 cm, avoiding major cervical vessels. Under ultrasound guidance, the needle was advanced along the tracheal outer edge to the tracheoesophageal groove or the recurrent laryngeal nerve pathway. The Diprospan mixture was injected to separate fibrotic scar tissue around the recurrent laryngeal nerve ( Fig. 3 ). The needle was withdrawn, disinfected, and a haemostatic plaster was applied . ④ Postoperative Observation: When the patient lies flat for 30 min after treatment, ultrasound is conducted, and if there are no abnormalities and if the patient is not uncomfortable, treatment can be concluded. However, if neither vocal cord activity nor voice condition improved within 1 wk after the completion of treatment, the treatment was repeated. The treatment was repeated up to 3 times. All ultrasound examinations and interventions were performed by an experienced ultrasound physician (W.Z., 18 y of experience) from the First Affiliated Hospital of Sun Yat-sen University.


Voice assessment
Subjective and objective assessment methods were used to evaluate the patient’s voice condition before and after treatment. The voice handicap index (VHI) score is a patient’s subjective assessment of their own voice quality. The maximum total score is 120. The higher the total score is, the worse the patient assesses their hoarseness. The American Association of Otolaryngology-Head and Neck Surgery (AAOHNS) guidelines state that the VHI is the highest quality scale for the preoperative and postoperative assessment of voice changes [ , ]. The subjective auditory perception assessment scale (GRBAS) score is a subjective assessment of a patient’s vocal acuity made by clinicians through hearing, and the maximum total score is 15 points [ ]. The higher the total score is, the more severe the hoarseness. Electronic laryngoscopy evaluation is a method used to objectively assess vocal cord mobility. Vocal cord fixation was scored as 1 point, improvement in glottis closure function or partial recovery of vocal cord movement was scored as 2 points, and normal vocal cord activity was scored as 3 points [ , ] ( Fig. 4 ). Improvement in vocal cord activity was measured in terms of an increase in the vocal cord mobility score.