Abstract
This retrospective case series evaluates an alternative embolization technique for splenic artery aneurysms (SAA) using a combination of coils and NBCA delivered through a Carry Leon NSX microcatheter, addressing the challenge of unpredictable NBCA behavior in high-risk aneurysms. Three female patients—a 55-year-old, a 60-year-old, and an 80-year-old—presented with SAAs that were either incidentally discovered or demonstrated significant growth over time, prompting intervention due to the potential risk of rupture. Each patient underwent successful embolization via a triple coaxial system that allowed precise coil placement and controlled NBCA injection, resulting in complete aneurysm occlusion with minimal complications such as mild splenic infarction or transient inflammatory responses. These cases demonstrate that the use of a PTFE-coated NSX microcatheter can enhance the safety and efficacy of NBCA injections, reduce the number of coils required, and simplify the embolization procedure, suggesting a promising advancement in the management of visceral arterial aneurysms.
Introduction
Splenic artery aneurysms (SAA) are the most common type of visceral artery aneurysms [ ] and carry a high risk of rupture when large or rapidly growing, requiring prompt treatment [ ]. Endovascular embolization has become the first-line treatment, replacing traditional surgical approaches owing to its minimally invasive nature and high success rates.
Coils and vascular plugs are typically used for SAA embolization. However, the use of liquid embolic agents like NBCA (n‑butyl 2-cyanoacrylate) has recently increased [ ]. NBCA offers advantages such as immediate and lasting effects, which result in a strong embolization effect. Despite these benefits, the behavior of NBCA during injection is unpredictable. NBCA is mixed with lipiodol to adjust its viscosity and control its solidification time; however, predicting the in vivo flow characteristics remain challenging [ ]. Risks include distal migration, proximal reflux, and catheter adhesion, which can lead to complications [ ].
To address these challenges, a Carry Leon NSX microcatheter with a polytetrafluoroethylene (PTFE)-coated tip was developed to reduce the risk of NBCA adhesion, thus enabling safer and more controlled injections [ ]. Its effectiveness in splenic artery embolization has been documented [ ]. This case series discusses 3 patients with SAAs treated using a combination of coils and NBCA injection via the Carry Leon NSX microcatheter, focusing on its utility and outcomes.
Case report
This was a retrospective case series of 3 patients with SAAs who were treated at our institution. The study was approved by the ethics committee and informed consent was obtained from all patients, both orally and in writing.
Case 1
A 55-year-old woman was referred to our hospital for the treatment of a splenic artery aneurysm (SAA). Six months prior to her visit, the aneurysm was incidentally discovered during the evaluation of left ureteral stones at a nearby hospital. Subsequent magnetic resonance imaging (MRI) revealed that the aneurysm was > 20 mm in size, prompting a referral for treatment.
Upon admission, the patient showed no abdominal symptoms. Blood tests revealed mildly elevated alkaline phosphatase (ALP) levels: ALP-IFCC, 128 U/L (normal range, 38-113 U/L) and ALP-JSCC, 364 U/L (normal range, 106-322 U/L). No other significant abnormalities were observed.
Preoperative contrast-enhanced computed tomography (CE-CT) revealed a 25 × 16 × 18 mm aneurysm near the splenic hilum, with a 6.7 mm inflow vessel and 2 outflow vessels measuring 4.2 mm and 6.4 mm ( Fig. 1 ). The splenic artery branches from the superior mesenteric artery.

A 5-Fr guiding sheath was introduced through the right femoral artery. A 4.2-Fr cobra-type catheter with a 0.035-inch guidewire was used to catheterize the superior mesenteric artery. A triple coaxial system with 2.85/2.9-Fr (Coiling Support EX, UTM, Aichi, Japan) and 1.9-Fr (Carry Leon NSX, UTM, Aichi, Japan) microcatheters was advanced into the splenic artery. One outflow vessel was embolized with 3 detachable coils ( Fig. 2A ). The other outflow vessel, measuring 6.4 mm in diameter, was chosen for embolization using AVP4 plugs. Initially, an AVP4 plug was deployed, but it migrated into the aneurysm sac ( Fig. 2B ). A second AVP4 plug was then used to successfully embolize the outflow vessel ( Fig. 2B ). After loose coil placement in the aneurysm ( Fig. 2B ), 3.9 mL of a 17% NBCA-lipiodol mixture was slowly injected over 8 minutes and 30 second ( Fig. 2C ). During injection, it was confirmed that the catheter tip did not adhere to NBCA or the vessel wall. Finally, the inflow vessel was embolized using a detachable coil ( Fig. 2D ). Postembolization digital subtraction angiography (DSA) confirmed aneurysm occlusion.

On the day following the embolization, blood tests revealed mild inflammatory changes, with a white blood cell (WBC) count of 14,600/µL (normal range, 3300-8600 /µL), C-reactive protein (CRP) of 1.08 mg/dL (normal range, <0.14 mg/dL), and a mildly elevated lactate dehydrogenase (LDH) level of 262 U/L (normal range, 124-222 U/L). These changes were associated with the embolization procedures. ALP levels remained mildly elevated compared to preoperative values, with ALP-IFCC at 126 U/L and ALP-JSCC at 358 U/L. The patient experienced left-sided abdominal pain, likely due to splenic infarction, which gradually improved. The patient was discharged on day 3, and a follow-up MRI confirmed complete occlusion of the aneurysm with a mild splenic infarction.
Case 2
A 60-year-old woman was referred to our hospital for treatment of SAA. The aneurysm was incidentally identified during follow-up imaging of the hepatic and pancreatic cysts. Over 3 years, the aneurysm showed a 14 mm increase in size, leading to treatment decisions. The patient had a history of left-sided breast cancer surgery and chronic renal failure.
At the time of admission, blood tests revealed mild elevations in ALP levels: ALP-IFCC 120 U/L and ALP-JSCC 341 U/L, as well as gamma-glutamyl transpeptidase (γGTP) at 54 U/L (normal range, 9-32 U/L). Additionally, an increased WBC count of 10,200 and CRP level of 0.89 mg/dL were observed. Grade 3 renal dysfunction was also confirmed, with a creatinine level of 3.22 mg/dL (normal range, 0.46-0.79 mg/dL) and a blood urea nitrogen (BUN) level of 53 mg/dL (normal range, 8-20 mg/dL).
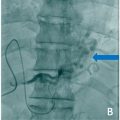
Because of renal dysfunction, preoperative evaluation was conducted using noncontrast magnetic resonance angiography (MRA), including the time-spatial labeling inversion pulse (Time-SLIP) method. The aneurysm measured 26 × 21 × 22 mm and was located near the splenic hilum ( Fig. 3 ). The inflow vessel measured approximately 8.4 mm, and the single outflow vessel measured 9.0 mm. A branch originating from the inflow vessel was identified, but the vessel was preserved. CO 2 angiography was performed during embolization to minimize the contrast.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree