Endocrine System
QUESTIONS
1 I-131 destroys the thyroid follicular cells by what particulate emission during its radioactive decay?
A. Alpha
B. Beta
C. Gamma
D. Positron
View Answer
1 Answer B. Iodine-131 (I-131) undergoes beta minus decay and emits a primary gamma photon of 364 keV as well as high-energy beta particles. Beta particles travel substantial distances in air, but only travel a few millimeters in tissue before getting absorbed. High radiation absorbed dose from beta particle emission combined with a long physical and biologic half-life of I-131 in the thyroid results in gradual destruction of the thyroid follicular cells. Gamma and positrons are photons and not particles.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:67-68, 71, 72.
2 What is the half-life of I-131?
A. 13 hours
B. 2.8 days
C. 3.2 days
D. 8.1 days
E. 13.2 days
View Answer
2 Answer D. I-131 has a half-life of 8.1 days.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014: 67-68.
A. I-131
B. In-111
C. I-123
D. Tc-99m
E. Tl-201
View Answer
3 Answer C. Iodine-123 (I-123) decays by electron capture and emits a primary gamma photon of 159 keV. No particulate emission (alpha or beta) combined with relatively short half-life results in low radiation absorbed dose to the thyroid gland. Also, the primary gamma photon of 159 keV is well suited for imaging using the modern gamma cameras.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:68, 71, 72.
4 You have 30 mCi of I-123 remaining in the radiopharmacy. A patient is scheduled to have an I-123 scintigraphy approximately 2 days from now. How much I-123 would remain at the time of the scheduled examination?
A. 25.3 mCi
B. 18.9 mCi
C. 8.3 mCi
D. 2.3 mCi
E. 1.2 mCi
F. 0.646 mCi
View Answer
4 Answer D. Iodine-123 has a half-life of 13 hours. Two days (48 hours) is slightly less than four half-lives of 52 hours. So the remaining activity would be slightly more than the residual activity of 1.8 mCi at 52 hours, making 2.3 mCi as the correct answer. Alternatively, this can be accurately calculated using the following formula:
A = A0 × e(-0.693/half – life)×(t)
A = remaining activity; A0 = activity at time 0; t = time of decay
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:4-5.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:68.
5 Which of the following radiopharmaceuticals is trapped by the thyroid follicular cells but NOT organified?
A. Tc-99m pertechnetate
B. I-123 sodium iodide
C. I-131 MIBG
D. In-111 pentetreotide
E. Tc-99m sestamibi
View Answer
5 Answer A. “Trapping” refers to the intracellular concentration of a substance by the sodium-iodine symporter located on the cell membrane of the thyroid follicular cells. “Organification” refers to oxidation, iodination, and coupling of iodine to the tyrosine residues on thyroglobulin by the thyroid peroxidase enzymes. Tc-99m pertechnetate undergoes trapping without organification. As such, it can gradually wash out of the thyroid gland, requiring imaging at 20 minutes after IV administration. On the other hand, I-123 and I-131 are organified into T3 and T4 and stored in the colloid-filled follicular lumen. Antithyroid medication such as propylthiouracil and methimazole block this organification process.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:66-69.
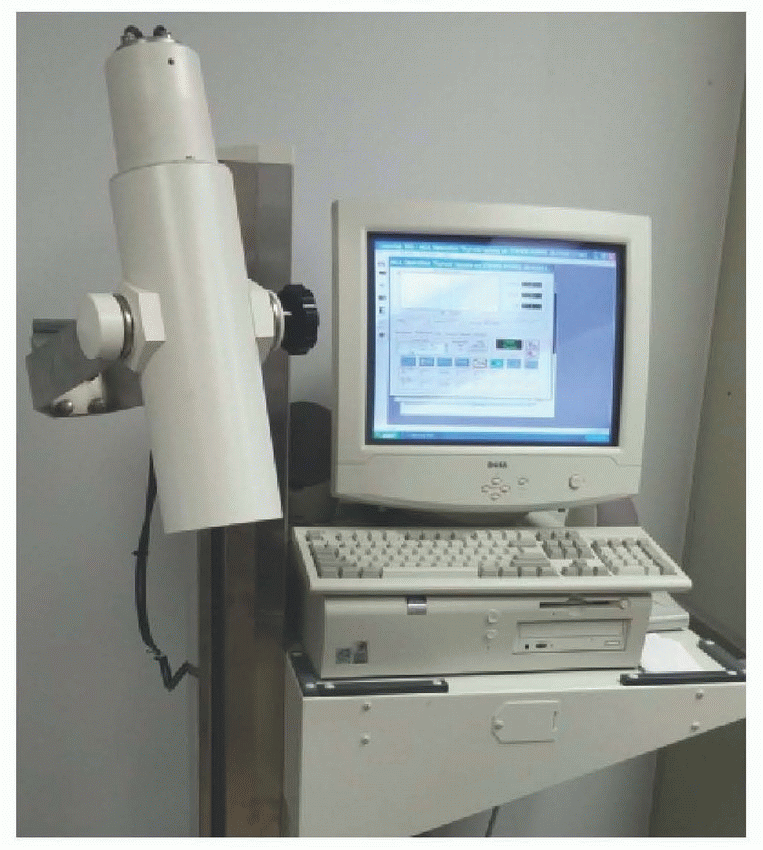
6 The instrument shown below is a scintillation probe, which is commonly used to calculate the radioiodine uptake by the thyroid gland. Which of the following instruments is most closely related to the scintillation probe?
 |
A. Geiger-Mueller counter
B. Ionization chamber
C. Well counter
D. Dose calibrator
View Answer
6 Answer C. Scintillation probes, well counters, and gamma cameras utilize crystal-based scintillation detectors (NaI, CdZnTe, etc.) coupled to a photomultiplier tube for radiation detection. Radiation from the radiopharmaceuticals generates light pulses in the crystal, which are then converted into a voltage signals by the photomultiplier tube (PMT). A scintillation probe used for thyroid uptake utilizes a thick (5-cm) NaI crystal coupled to a PMT. A well counter uses a similar crystal with a well cut into the center of the crystal where a sample may be placed; it is a highly sensitive device used to detect a very small amount of radioactivity (up to 1 mCi) such as those of wipe tests or in vitro studies (GFR, shillings test, etc.).
Geiger-Mueller (GM) counters, ionization chambers, and dose calibrators employ detectors with gas-filled chambers. Radiation from the radiopharmaceuticals interacts with the gas, causing ionization and generating an electric signal. A GM survey meter is used to detect low levels of radiation, while ionization survey chamber can be used to detect and quantify higher levels of radiation. A dose calibrator is a well-type ionization chamber used to accurately measure the radiopharmaceutical doses (activities) given to the patients.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:23-29.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:38-44, , 70-71.
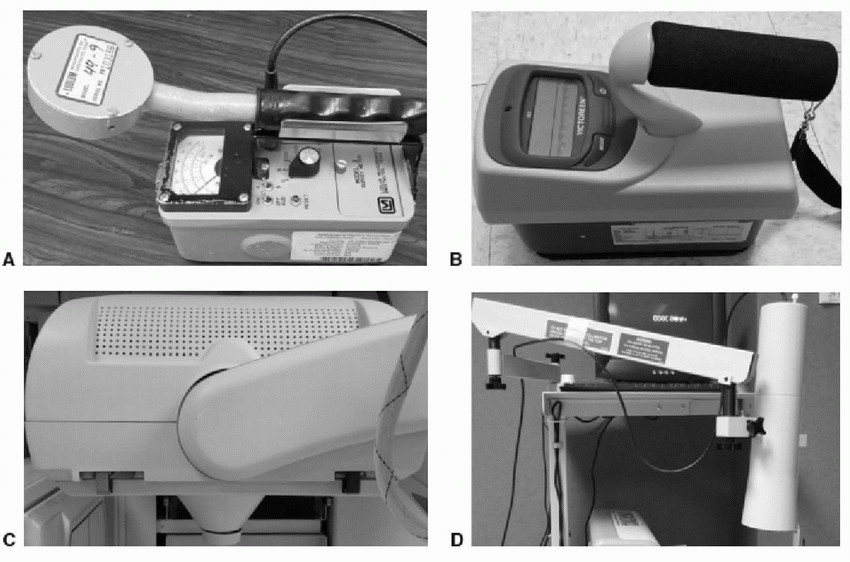
7 A 67-year-old gentleman received 101 mCi of I-131 sodium iodide for the treatment of his differentiated thyroid carcinoma. Which of the following instruments would be typically used to measure the radioactivity emanating from the patient prior to his release?
 |
View Answer
7 Answer B. Ionization chambers (image B) are typically used to measure high exposure rates (range from 0.1 mR to 100 R) such as those from the patients receiving radioiodine therapy for cancer. If the patient receives more than 33mCi of I-131 on an outpatient basis, then precautions are taken to ensure that no other person would receive more than 500 mrem (5 mSv) from exposure to the released patient. Activity is measured at 1 m and 3m using an ionization chamber, and values are typically entered into a spreadsheet to generate a list of precautions to be discussed with the patient and the family members. Geiger-Mueller counters (image A) are very sensitive and are used to detect a very small amount of radioactivity (i.e., contamination). Gamma camera (image C) and scintillation probe (image D) are used for scintigraphy and radioiodine uptake measurement, respectively.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:23-29.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:38-44.
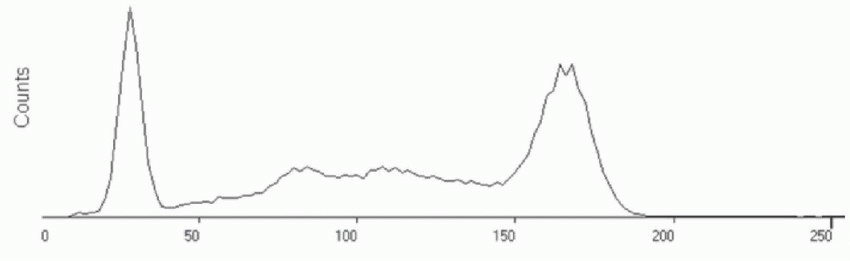
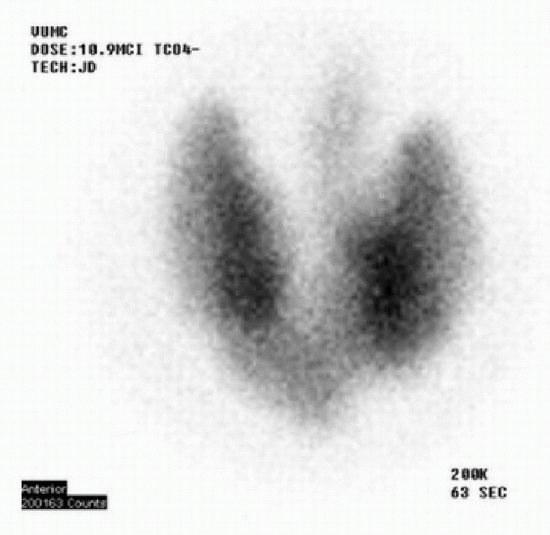
8 The following Tc-99m pertechnetate thyroid scintigraphy image is from a 25-year-old female with hyperthyroidism. What is the most likely 24-hour I-123 radioiodine uptake (RAIU) value for this patient?
 |
A. 5%
B. 15%
C. 30%
D. 60%
View Answer
8 Answer D. The 20-minute anterior image obtained after IV administration of 10.9 mCi of Tc-99m pertechnetate demonstrates enlarged thyroid gland with convex borders. A linear focus of activity extending superiorly from the left isthmus is the pyramidal lobe. The absence of significant background activity and lack of visualization of the physiologic uptake in the salivary glands imply marked increase in the radiopharmaceutical uptake. The findings are those of Graves disease. The Graves disease is caused by increased levels of thyroid-stimulating immunoglobulins (TSI), which cause marked overstimulation of the thyroid follicular cells. The typical 24-hour RAIU in these patients ranges from 50% to 80%. In comparison, the 24-hour RAIU in multinodular goiter and toxic autonomously functioning nodule ranges from 20% to 30% (upper limits of normal to mildly elevated). Normal %RAIU is 4% to 15% at 4 to 6 hours and 10% to 30% at 24 hours.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:74-76.
9 What type of collimator is typically used to acquire I-123 thyroid scintigraphy images?
A. Low energy high resolution (LEHR)
B. Medium energy
C. High energy
D. Pin hole
View Answer
9 Answer D. Pinhole collimator is typically used for imaging the thyroid gland. The resultant magnification provides superior resolution compared to the parallel hole collimator.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:72.
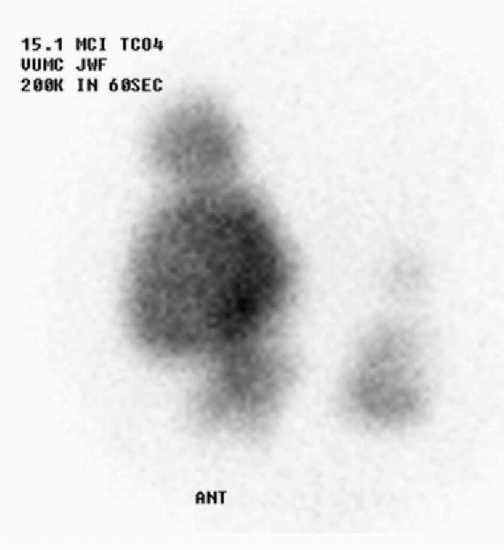
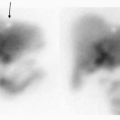
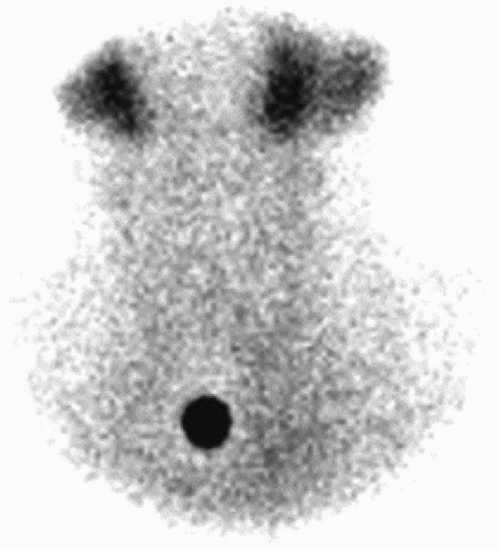
10a The following image is from a 21-year-old female with recent history of viral upper respiratory infection who presents with the complaints of palpitations and tremor. Which of the following is the most likely diagnosis?
 |
A. Plummer disease
B. Subacute thyroiditis
C. Graves disease
D. Acute suppurative thyroiditis
E. Primary hypothyroidism
View Answer
10a Answer B. Absent or poor visualization of thyroid gland and decreased RAIU are seen with primary or secondary hypothyroidism, thyroid gland destruction (acute phase of subacute thyroiditis, type II amiodarone toxicity), exposure to excess iodine (iodinated contrast, or type I amiodarone toxicity), or suppression of thyroid from excess exogenous thyroid hormone (struma ovarii or factitious hyperthyroidism). In this patient with clinical history of recent URI and symptoms of hyperthyroidism, the diagnosis is subacute thyroiditis, specifically subacute granulomatous thyroiditis.
Acute suppurative thyroiditis is an extremely rare but potentially life-threatening bacterial infection; patients present with anterior neck swelling, pain, and fever. However, it typically does not result in significant hyperthyroidism. Plummer disease and Graves disease result in hyperthyroidism but demonstrate increased radioiodine uptake.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:76-78
10b What is the cause of hyperthyroidism in these patients?
A. Increased thyroid-stimulating immunoglobulins
B. Increased thyroid hormone production
C. Increased TSH secretion by the pituitary
D. Release of preformed thyroid hormone
E. Antithyroid peroxidase antibodies
View Answer
10b Answer D. Subacute thyroiditis occurs secondary to the destruction of the thyroid follicular cells, which results in the spillage of preformed thyroid hormone into the bloodstream. Three forms of subacute thyroiditis are recognized: subacute granulomatous thyroiditis (aka painful or de Quervain thyroiditis), subacute lymphocytic thyroiditis (aka painless thyroiditis), and subacute postpartum thyroiditis. Increased thyroid-stimulating immunoglobulins (TSI) are seen with Graves disease. Antithyroid peroxidase antibodies are typically seen with Hashimoto’s thyroiditis.
References: Fatourechi V, Aniszewski JP, Fatourechi GZ, et al. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab 2003;88(5):2100-2105.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:76-78.
11 Which of the following symptoms would be MOST helpful in establishing the correct diagnosis of subacute granulomatous thyroiditis, also known as de Quervain thyroiditis?
A. Painful thyroid on palpation
B. Nonpalpable thyroid
C. Nodular thyroid gland
D. Proptosis
E. Tachycardia
View Answer
11 Answer A. The specific diagnosis in patients with absent or markedly decreased radioiodine uptake and hyperthyroidism depends on their clinical presentation. Specific clinical inquiries regarding recent URI infection and neck pain, recent exposure to iodinated contrast, postpartum status, and amiodarone treatment would help establish a specific diagnosis of subacute granulomatous thyroiditis, Jod-Basedow syndrome, postpartum thyroiditis, and amiodarone toxicity, respectively. Proptosis would indicate Graves disease, while a nodular thyroid gland would imply toxic multinodular goiter.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:76-78.
12 What is the most appropriate I-131 dose to treat the patients with Graves disease?
A. 1 to 4 mCi
B. 5 to 20 mCi
C. 30 to 100 mCi
D. 101 to 200 mCi
View Answer
12 Answer B. Most patients with Graves disease are effectively treated with I-131 with only 10% requiring retreatment. Symptomatic improvement is usually noted by 3 weeks with full therapeutic effect typically in 3 to 6 months. Some patients may experience exacerbation of hyperthyroidism symptoms due to spillage of preformed thyroid hormone. Elderly patients with cardiac history and pediatric patients may benefit from pretreatment with methimazole to “cool down” the thyroid gland and beta blockade to prevent tachycardia.
One of the approaches to treating Graves disease is to use an empirical I-131 dose in the range of 8 to 15 mCi. Another approach takes into account the estimated size of the thyroid gland and 24-hour RAIU using the following formula: I-131 dose = (estimated thyroid gland size × 0.130 to 0.180 mCi/g of thyroid tissue)/24 hour RAIU.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:84.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:84.
A. 5 mCi
B. 10 mCi
C. 30 mCi
D. 100 mCi
View Answer
13 Answer C. Compared to Graves disease, hyperthyroidism from toxic multinodular goiter (MNG) is generally more resistant to radioiodine therapy. This combined with lower RAIU by the thyroid (20% to 30%) in MNG requires about twice the amount of I-131 compared to Graves disease. The typical empirical I-131 dose ranges from 20 to 30 mCi. Similar approach is used in treating a toxic autonomously functioning thyroid nodule.
References: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:84.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:84.
14 Which of the following disease process results in increased radioiodine uptake by the thyroid gland?
A. Viral thyroiditis
B. Iodine deficiency-induced hypothyroidism
C. Jod-Basedow phenomenon
D. Factitious hyperthyroidism
View Answer
14 Answer B. Iodine deficiency-induced hypothyroidism would result in elevated radioiodine uptake due to increased stimulation from elevated TSH levels. This is rarely seen in developed countries in the present day and age. The remaining choices demonstrate decreased or absent radioiodine uptake in the thyroid gland.
Reference: Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Saunders, 2012:101-102.
15 How long after administration of I-131 radioiodine can the patient resume breast-feeding?
A. 8 days
B. 80 days
C. 8 months
D. Next pregnancy
View Answer
15 Answer D. Iodine is concentrated in large amounts by the glandular tissue in the breast and is secreted in the breast milk. As such, all lactating women undergoing I-131 therapy should be asked to stop breast-feeding in order to minimize the radiation dose to the sensitive breast tissue and to prevent the infant’s exposure to I-131. Lactation and the ability of the breast tissue to concentrate large amount of iodine stop 4 to 6 weeks after delivery or cessation of breast-feeding. As such, if possible, therapy should be delayed for approximately 6 weeks, and the patient should be initiated on dopamine agonist therapy to reduce the absorbed dose to the breast tissue. The patient should not resume breast-feeding for that child but may resume with the birth of another child.
References: Baeumler GR, Joo KG. Radioactive iodine uptake by breasts. J Nucl Med 1986;27(1):149-151.
Oh JR, Ahn BC. False-positive uptake on radioiodine whole-body scintigraphy: physiologic and pathologic variants unrelated to thyroid cancer. Am J Nucl Med Mol Imaging 2012;2(3):362-385.
Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:70.
16 How long after administration of I-123 radioiodine can the patient resume breast-feeding?
A. 24 hours
B. 48 hours
C. 8 days
D. Next pregnancy
View Answer
16 Answer B. Radioiodine is concentrated and secreted by the glandular tissue of the breast. Unlike I-131, Tc-99m pertechnetate and I-123 have short half-lives and do not emit beta radiation. As such, breast-feeding may resume 48 hours after administration of I-123 and 24 hours after administration of Tc-99m pertechnetate.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:70.
17 What is the most accurate serum tumor marker to detect the recurrence of a well-differentiated papillary or follicular thyroid carcinoma?
A. Triiodothyronine
B. Thyroglobulin
C. Thyrogen
D. Thyroid peroxidase antibody
E. Calcitonin
F. Thyroid-stimulating immunoglobulin
View Answer
17 Answer B. Serum thyroglobulin (Tg) is the most accurate tumor marker to detect recurrence of a well-differentiated thyroid carcinoma. It is not useful for poorly differentiated, anaplastic, or medullary forms of thyroid carcinoma. Please note that the presence of Tg antibody may compromise the accuracy of the Tg essay.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:85, 89.
18 Whole-body radioiodine scintigraphy is the most effective method for tumor detection and staging of what malignancy?
A. Medullary thyroid carcinoma
B. Papillary thyroid carcinoma
C. Hurthle cell thyroid carcinoma
D. Anaplastic thyroid carcinoma
View Answer
18 Answer B. Papillary thyroid carcinoma is the most common thyroid malignancy and represents about 80% to 90% of well-differentiated thyroid cancers. Well-differentiated thyroid cancers are usually iodine avid but not FDG avid. Whole-body scan with radioiodine is the most effective method for tumor detection, staging, and treatment planning in patients with differentiated thyroid carcinoma (DTC).
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:84-85.
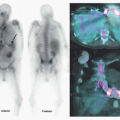
19 The following whole-body posttherapy I-131 scintigraphy was acquired in a patient with history of high-risk, well-differentiated papillary thyroid carcinoma who was treated with 157 mCi of I-131 7 days ago. What is the significance of radiopharmaceutical uptake within the liver?
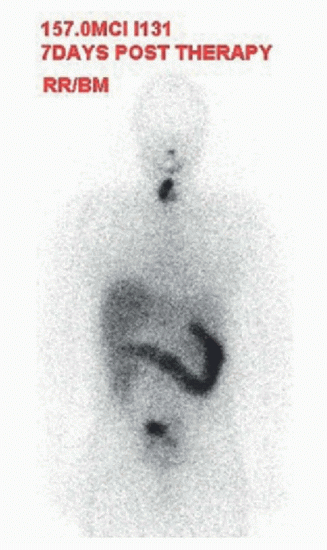 |
A. Physiologic distribution
B. Liver metastasis
C. Fatty liver
D. Hepatitis
E. Cirrhosis
View Answer
19 Answer A. A large focus of intense activity within the right thyroid bed and a small focus of mild activity within the left thyroid bed likely represent remnant thyroid tissue in this patient with clean surgical margins on pathology. Physiologic radioiodine distribution is seen in the salivary glands, the oral cavity, liver, bowel, and bladder. Thyroid hormone undergoes conversion from T4 to T3 by type I iodothyronine deiodinase within the liver. Thus, presence of liver uptake suggests evidence of functioning thyroid tissue elsewhere in the body. In this patient with remnant thyroid tissue in the neck, this finding is physiologic and requires no further workup.
References: Oh JR, Ahn BC. False-positive uptake on radioiodine whole-body scintigraphy: physiologic and pathologic variants unrelated to thyroid cancer. Am J Nucl Med Mol Imaging 2012;2(3):362-385.
Shapiro B, Rufini V, Jarwan A, et al. Artifacts, anatomical and physiological variants, and unrelated diseases that might cause false-positive whole-body 131-I scans in patients with thyroid cancer. Semin Nucl Med 2000;30(2):115-132.
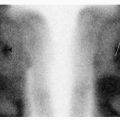
20 The following whole-body I-123 scintigraphy is of a patient who underwent thyroidectomy and radioiodine ablation for differentiated thyroid carcinoma 5 years ago. She now has progressively increasing serum thyroglobulin (Tg) levels, and her recent Thyrogen-stimulated Tg level was 23 ng/mL. What is the most appropriate next step?
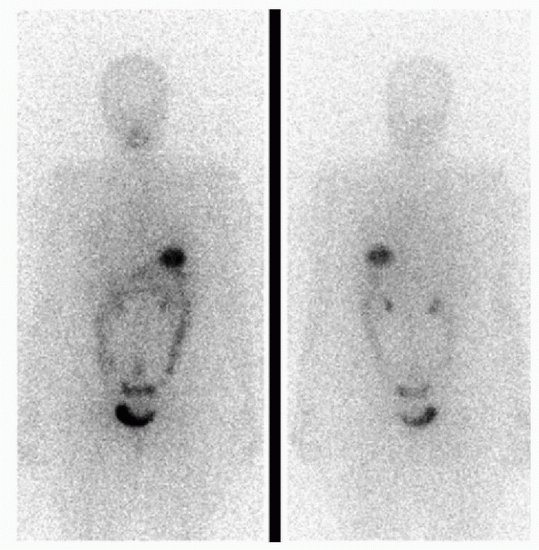 |
A. Follow-up I-123 scan in 6 months
B. Follow-up I-123 scan in 1 year
C. CT of the abdomen
D. I-131 therapy
E. FDG PET/CT
View Answer
20 Answer E. Delayed anterior and posterior whole body images demonstrate physiologic radiotracer uptake within the nasal mucosa, oral cavity, stomach, bowel, renal collecting system, and bladder. There are no foci of abnormal activity identified. F-18 FDG uptake in differentiated thyroid carcinoma (DTC) is related to the loss of differentiation and transformation of the tumor into a higher grade. As such, FDG PET/CT is useful in the detection and localization of recurrent DTC in patients with negative diagnostic radioiodine imaging despite elevated thyroglobulin (Tg) levels; Centers for Medicare and Medicaid Services requires serum TG level of >10 ng/mL for approval of the procedure. The diagnostic accuracy of FDG PET/CT increases with increasing stimulated Tg levels and is most promising at levels >20 ng/mL.
References: Na SJ, Yoo Ie R, O JH, et al. Diagnostic accuracy of (18)F-fluorodeoxyglucose positron emission tomography/computed tomography in differentiated thyroid cancer patients with elevated thyroglobulin and negative (131)I whole body scan: evaluation by thyroglobulin level. Ann Nucl Med 2012;26(1):26-34.
Schlüter B, Bohuslavizki KH, Beyer W, et al. Impact of FDG PET on patients with differentiated thyroid cancer who present with elevated thyroglobulin and negative 131I scan. J Nucl Med 2001;42:71-76.
21 A patient with high-risk differentiated thyroid carcinoma (DTC) is undergoing thyroid hormone withdrawal prior to radioiodine ablation therapy. Serum TSH value greater than what level is desirable to ensure maximal effect of the ablation?
A. 10 mIU/L
B. 15 mIU/L
C. 30 mIU/L
D. 60 mIU/L
View Answer
21 Answer C. The patients undergoing radioiodine ablation therapy (RIAT) for DTC should undergo thyroid hormone withdrawal by stopping tetraiodothyronine (LT4, Synthroid) for 4 weeks or triiodothyronine (LT3, Cytomel) for 2 weeks before RIAT. The resultant elevation in the endogenous TSH levels ensures proper stimulation of the thyroid tissue to allow poorly functioning or small amount of residual thyroid tissue to take up maximal amount of radioiodine. Serum TSH value greater than 30 mIU/L is desirable, and a level greater than 50 mIU/L is optimal for this purpose. For patients who are unable to tolerate hypothyroidism or unable to generate an elevated TSH level, remnant ablation can be achieved with two doses of rhTSH (Thyrogen) given intramuscularly 48 and 24 hours before RIAT.
Reference: Ziessman HA, O’Malley JP, Thrall JH. Nuclear medicine: the requisites, 4th ed. Philadelphia, PA: Saunders, 2014:84-86.
22 What is the radiopharmaceutical of choice for the evaluation of substernal goiter/anterior mediastinal mass?
A. I-131
B. I-123
C. Tc-99m pertechnetate
D. Tc-99m sestamibi
View Answer




22 Answer B. Benefits of I-123 radioiodine imaging are better target to background ratio, better tissue penetration, and improved specificity (compared to pertechnetate) as well as ability to perform SPECT-CT images (compared to I-131). As such, it is the radiopharmaceutical of choice for the evaluation of substernal goiter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree