Abstract
Vascular complications, though rare, significantly increase the morbidity and mortality associated with necrotizing pancreatitis (NP). While arterial pseudoaneurysms are well-documented, major venous injuries, particularly superior mesenteric vein (SMV) erosion, are exceedingly uncommon, with only 2 cases previously reported in the literature. We describe a 41-year-old male with severe necrotizing pancreatitis complicated by abdominal compartment syndrome, who developed acute, life-threatening hemorrhage due to pancreatic enzyme erosion of the SMV. Surgical attempts to control the bleeding were unsuccessful, and the hemorrhage was ultimately managed with endovascular stent grafting of the SMV. This case underscores the complexity of vascular injuries in pancreatitis and highlights the potential role of endovascular interventions, such as venous stent grafting, as life-saving procedures when conventional surgical techniques fail. Our case adds to the limited but growing body of evidence supporting the use of venous stenting for mesenteric venous injuries in NP.
Introduction
Vascular complications in necrotizing pancreatitis (NP) significantly increase morbidity and mortality, affecting approximately 25% of patients with NP [ ]. These complications can manifest as pseudoaneurysm formation, thrombosis, stenosis, or, more rarely, complete venous disruption. While arterial injuries are more common, venous injuries are particularly challenging due to their rarity and the lack of established management guidelines. The complexity of the superior mesenteric vein (SMV) anatomy, its critical role in mesenteric circulation, and the proximity of other vital structures make injuries in this area especially challenging to treat. Endovascular stenting has emerged as a viable therapeutic option for venous injury, particularly in high-risk cases where surgical repair is not feasible.
To our knowledge, no prior cases of SMV erosion treated with endovascular stent grafting in the context of NP have been reported. We present the case of a 41-year-old male with necrotizing pancreatitis complicated by abdominal compartment syndrome and refractory hemorrhage from SMV erosion. The bleeding was successfully controlled with SMV stenting, with subsequent surgical confirmation of the exposed stent within the disrupted venous wall.
Case presentation
A 41-year-old male with a medical history of hypertension and hyperlipidemia presented with acute pancreatitis and acute kidney injury. His condition rapidly deteriorated, requiring mechanical ventilation for hypoxic respiratory failure. Computed tomography (CT) of the abdomen revealed acute interstitial pancreatitis ( Fig. 1 ), and endoscopic retrograde cholangiopancreatography (ERCP) confirmed the absence of gallstones. Due to worsening necrosis, pseudocyst formation, and nontraumatic abdominal compartment syndrome leading to end organ damage, the patient underwent decompressive laparotomies and necrosectomies.

Frank bloody output from his Jackson-Pratt (JP) drain prompted an urgent computed tomography angiography (CTA), which revealed an arterial source of bleeding from a branch of the celiac artery.
Interventional radiology (IR) embolized a 12 mm dorsal pancreatic artery pseudoaneurysm ( Fig. 2 ), but the patient’s critical condition persisted. Multiple exploratory laparotomies and necrosectomies evacuated significant volumes of necrotic tissue and old blood from the abdominal cavity.

Subsequently, the patient experienced hemodynamic collapse with severe hypotension and copious hemorrhagic output from his abdominal drains. Emergent exploratory laparotomy revealed significant bleeding from a large venous vessel and near-complete pancreatic necrosis. Intraoperative attempts to control the bleeding were unsuccessful, leading to temporizing abdominal packing.
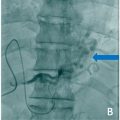
Postoperative CTA and CT venogram showed left hepatic and splenic infarctions, a compressed mid-SMV with patent distal segments, and a hyperdense hematoma near the inferior vena cava (IVC) ( Fig. 3 ). The IR team was consulted for possible SMV repair.