KEY FACTS
Terminology
- •
Inflammation of epididymis &/or testis
Imaging
- •
Grayscale US
- ○
Epididymis enlarged and hypoechoic
- ○
Testes mildly heterogeneous
- ○
- •
Color Doppler US
- ○
Diffuse or focal hyperemia in body and tail of epididymis ± increased vascularity of testis
- ○
In severe cases can cause vascular compromise and ischemia or infarction
- ○
Reversal of arterial diastolic flow of testis is ominous finding associated with testicular infarction
- ○
- •
Orchitis is usually secondary, occurring in 20-40% of epididymitis due to contiguous spread of infection
Top Differential Diagnoses
- •
Testicular torsion
- •
Testicular lymphoma
- •
Testicular trauma
Pathology
- •
Starts within tail of epididymis → body → testis
Clinical Issues
- •
Commonest cause of acute scrotal pain in adolescent boys and adults (15-35 years)
- •
Males 14-35 years of age: Most commonly caused by Neisseria gonorrhoeae and Chlamydia trachomatis
- •
Scrotal swelling, erythema; fever; dysuria
- ○
Scrotal pain due to epididymitis is usually relieved after elevation of testes (scrotum) over symphysis pubis (Prehn sign)
- ○
Associated lower urinary tract infection and its symptoms, urethral discharge
- ○
- •
Prognosis excellent if treated early with antibiotics; follow-up scans to exclude abscess if no improvement
Scanning Tips
- •
Compare side by side with contralateral asymptomatic side with both color and power Doppler in single image
- ○
Avoid using dual image for side-by-side comparison
- ○
Suggested setting for color Doppler: 5 cm/s
- ○
- •
Head, body, and tail of epididymis should be carefully evaluated
- •
Use high-frequency transducers (9-15 MHz)
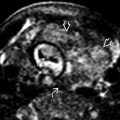
 enveloping the testis posteriorly. Note that the testis
enveloping the testis posteriorly. Note that the testis  appears normal in size and configuration.
appears normal in size and configuration.
 compared to the left, and there is a small right hydrocele
compared to the left, and there is a small right hydrocele  .
.
 .
.
 of the epididymis consistent with acute epididymitis.
of the epididymis consistent with acute epididymitis.
 in appearance compared to the left, consistent with right-sided orchitis. In addition, there are associated findings of scrotal wall thickening
in appearance compared to the left, consistent with right-sided orchitis. In addition, there are associated findings of scrotal wall thickening  and a small hydrocele
and a small hydrocele  .
.
 in a patient with a history of epididymo-orchitis. The findings are consistent with a pyocele.
in a patient with a history of epididymo-orchitis. The findings are consistent with a pyocele.