Esophageal Stents
Ho-Young Song
Ji Hoon Shin
Chang Jin Yoon
Fluoroscopic or endoscopic placement of a covered or bare expandable metallic stent is increasingly being used for the treatment of malignant (1,2,3,4,5,6,7,8,9,10,11,12,13,14) and benign (15,16,17) esophageal strictures. These stents are thought to provide superior mortality and morbidity benefits and more effective relief of dysphagia when compared with other conventional esophageal prostheses.
Indications
1. Unresectable or inoperable esophagogastric neoplasms
2. Patients with resectable esophageal neoplasms who wish to avoid surgery
3. Patients who need nourishment prior to surgery or chemoradiation therapy
4. Esophagorespiratory fistula (ERF) due to a malignant tumor
5. Extraluminal compression by neoplasms or adenopathy
6. Benign esophageal strictures refractory to balloon dilation
Removal of placed stents (14,17,18) is indicated for (a) patients with complications after stent placement such as severe pain, stent migration, or stent deformity; (b) patients with stent placement for the sole purpose of nourishment prior to surgery or chemoradiation therapy; and (c) patients with a benign stricture who only need temporary treatment.
Contraindications
Relative
1. Uncontrollable bleeding diathesis
2. Severely ill patients with a very limited life expectancy
3. Severe vocal cord palsy
4. Multiple obstructive lesions of the small bowel (e.g., peritoneal seeding)
5. Neoplasms involving the upper esophageal sphincter
Preprocedure Preparation
1. Obtain informed consent.
2. Stop all oral intake for 8 hours before procedure.
3. Check hematocrit, platelet count, prothrombin time (PT), and partial thromboplastin time (PTT) and correct as necessary.
4. Perform esophagography and/or endoscopy to assess location and length of the stricture.
Procedure
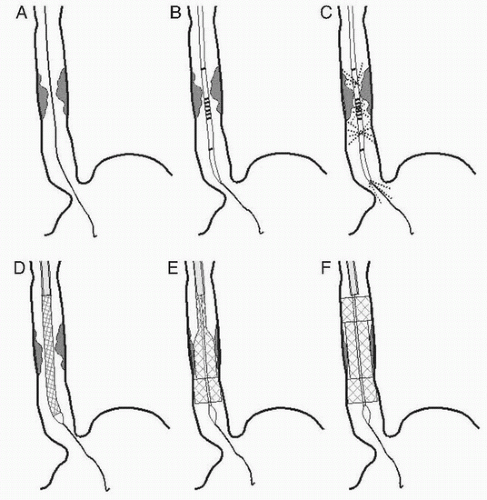
Stent Placement (Fig. e-79.1A-F)
1. A variety of instruments and techniques for stent placement have been developed (2,3,4,5,6,7,8,9,10,11,12,13,19,20,21). Stents available in the United States are listed in Table e-79.1.
2. The pharynx is topically anesthetized (aerosol lidocaine spray), and conscious sedation is administered according to institutional protocols.
3. Extending the patient’s neck and placement of an oral airway may facilitate the procedure. Atropine may be useful for managing vagal tone or copious secretions.
4. With the patient in the left anterior oblique position, a 0.035-in. stiff guidewire (Radifocus Guide Wire M, Terumo Corp, Tokyo, Japan) is inserted—with or without the help of an angiographic catheter—through the mouth across the stricture into the distal esophagus or stomach (Fig. e-79.1A).
5. A sizing catheter (S&G Biotech, Seongnam, South Korea) is passed over the guidewire to inject water-soluble contrast medium and to measure the length of stricture (Fig. e-79.1B,C).
6. The location of the stricture is marked on the patient’s skin under fluoroscopic control.
Table e-79.1 Characteristics of Currently Available Esophageal Stents | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
7. The sizing catheter is removed, leaving the guidewire in place.
8. A preloaded stent-delivery system, whose proximal part is lubricated with jelly, is passed over the guidewire into the esophagus and advanced until the distal end of the stent reaches beyond the stricture (Fig. e-79.1D). If the stricture is too tight to accommodate the stent-delivery system, balloon predilation is needed up to maximum 10 mm.
9. The position of the stent relative to the stricture is confirmed with contrast injection. Allow 1 to 2 cm of the stent to extend beyond both ends of the lesion.
10. The introducing sheath is slowly withdrawn over the pusher in a continuous motion, freeing the stent to expand within the stricture (Fig. e-79.1E,F). The delivery system and guidewire are then removed.
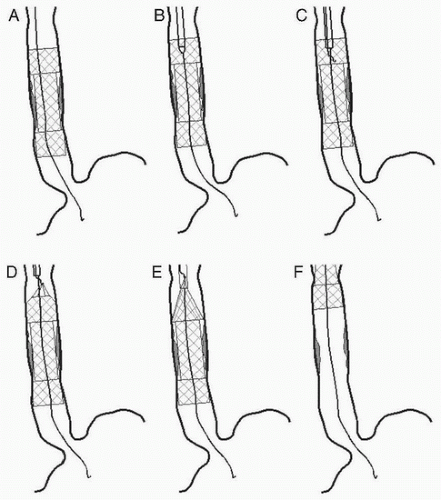
Stent Removal (Fig. e-79.2A-F)
1. To facilitate stent removal, nylon drawstrings are attached to the upper inner margin of a retrievable stent (Taewoong Medical, Goyang, South Korea) (8,14,17).
2. After topical anesthesia of the pharynx with an aerosol spray, a 0.035-in. stiff guidewire (Radifocus Guide Wire M) is introduced through the mouth and then across the stent into the distal esophagus or stomach (Fig. e-79.2A).
3. A sheath with a dilator is passed down over the guidewire into the proximal stent lumen (Fig. e-79.2B).
4. After the guidewire and the dilator are removed from the sheath, a hook catheter is introduced into the sheath and advanced until its metal part passes through the sheath into the stent lumen (Fig. e-79.2C).
5. The sheath with the hook catheter is then pulled out of the stent so that its metal part hooks onto the nylon thread (Fig. e-79.2D). Then the hook catheter is withdrawn through the sheath to collapse the proximal stent when it reaches the sheath tip (Fig. e-79.2E).
6. The sheath, hook catheter, and stent are then pulled together out of the esophagus (Fig. e-79.2F).
Postprocedure Management
Postplacement
1. Patients can be allowed a liquid diet 1 hour after the procedure. A patient with an ERF is restricted to food until the 1-day follow-up esophagography.
2. Patients in whom the stent straddles the distal esophageal sphincter are advised to sleep in a semierect position to minimize reflux and aspiration of gastric contents. Proton pump inhibitor (lansoprazole 15 mg) should be used to reduce reflux through the stent.
3. Esophagography is performed 1 day after stent placement to verify the position and patency of the stent.
4. Diet can be advanced to soft and solid diet after confirmation of stent expansion and position.
5. Advise proper chewing of food and use of carbonated drinks to reduce risk of food impaction.
Postretrieval
1. Patients can be allowed a liquid diet 1 hour after the procedure.
2. Esophagography is performed just after stent removal to check any complications.
3. Diet can be advanced to soft and solid diet, if there are no issues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree