Progressively less invasive neurosurgical approaches for the treatment of movement disorders have evolved, beginning with open craniotomy for placement of lesions within pyramidal structures followed by refined stereotactic ablation of extrapyramidal targets that encouraged nondestructive electrode stimulation of deep brain structures. A noninvasive approach using transcranial high-energy focused ultrasound has emerged for the treatment of intractable tremor. The ability to target discreet intracranial sites millimeters in size through the intact skull using focused acoustic energy marks an important milestone in movement disorders surgery. This article describes the evolution of magnetic resonance-guided focused ultrasound for ventrolateral thalamotomy for tremor.
Key points
- •
Historically, patients with tremor of various causes, including essential tremor (ET), parkinsonian rest tremor, and action tremor, have been treated with stimulation or lesions placed in the ventrolateral thalamus.
- •
The most effective antitremor target in the brain may be the ventrointermedius (Vim) nucleus of the thalamus, a small subnucleus of the ventrolateral thalamus.
- •
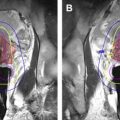
It is now possible to create a lesion in the Vim nucleus using magnetic resonance (MR) imaging–guided high-energy focused ultrasound in a patient who is awake without a skin incision or craniotomy.
History of movement disorders surgery
Gildenberg describes five major epochs in the evolution of modern movement disorders surgery: (1) the prestereotactic era before 1947, (2) the early stereotactic revolution between 1947 and 1969, (3) the latent period after the introduction of levodopa in the 1970s and 1980s, (4) the stereotactic revival of ablative surgery in the 1990s, and (5) the current modern period of deep brain stimulation. At present, with the advent of high-energy transcranial focused ultrasound, movement disorders surgery may be about to enter a sixth epoch. This article traces the historical progression of movement disorders surgery from early open craniotomy to the so-called incisionless image-guided ultrasound surgery that is now being developed to treat ET. It also describes relevant history of focused ultrasound and a few general principles that have allowed neurosurgeons to treat intractable tremor with acoustic ablation.
The Prestereotactic Era
An early experimental understanding of motor systems began in the late 1800s, when Fritsch and Hitzig conducted the first investigations into mammalian motor circuitry by applying local electrical stimulation to the cortical surface in dogs. Based on this pioneering work, Horsley, in 1909, resected a portion of the contralateral precentral gyrus in a 15-year-old boy for the treatment of postcarlatina hemiathetosis but acknowledged in later reports that these procedures often resulted in severe paralysis and paresis. Hoping to alleviate tremor without weakness, Horsley and Clarke attempted to target specific structures outside primary motor centers, for example, the deep cerebellar nuclei and other subcortical structures. They used the first skull-mounted stereotactic frame using external landmarks to guide slender probes and initiated the first use of discrete electrolytic lesions. The goal of these elegant preclinical investigations in the monkey was to find areas in the brain where small lesions could be accurately placed to control unwanted movements but not abolish movement altogether. This pioneering work in intracranial stereotaxy had to wait until the 1940s to finally be applied to human surgery (see later discussion).
Although Horsley and Clarke laid the groundwork for an understanding of nonprimary motor areas in the brain, other investigators were beginning to study extracranial approaches to abnormal movements. As early as 1908, Foerster reported posterior rhizotomy for control of spasticity and rigidity, leading others to try sympathetic ramisection and various ganglionectomies for similar indications throughout the 1920s and 1930s. During this same period, surgical interest in open craniotomy for ablation of primary cortical structures continued despite permanent loss of function and high mortality. For example, Bucy and colleagues continued to report their series treating athetosis and parkinsonism with ablation of both the supplementary and primary motor cortices despite accruing evidence from Meyers and others that lesions confined strictly to the extrapyramidal system controlled tremor without weakness. Meyers reported excellent tremor control in a patient with hemiparkinsonism by resection of the contralateral caudate head through a transventricular approach, confirming that the basal ganglia is a viable extrapyramidal target for tremor. For other patients, Meyers also explored sectioning of the anterior internal capsule, ansa lenticularis (ansotomy), and internal pallidum. Despite the success of these transventricular extrapyramidal operations, postoperative mortality was never reduced less than 10%, deterring others from adopting similar free-hand transventricular approaches. Nevertheless, Meyers’ contributions clearly showed that basal ganglia lesions could effectively treat tremor without causing paralysis or coma. These decisive observations set the stage for future stereotactic surgical methods in targeting extrapyramidal subcortical structures for the treatment of refractory movement disorders.
The Early Stereotactic Revolution
It was not until after 1947, when Spiegel and colleagues described a procedure to ablate discrete targets in the human brain using a modification of the Horsley-Clarke frame, that the era of stereotactic surgery clinically emerged. The major advantage of their approach was the use of indirect internal landmarks based on ventricular encephalography to identify particular sites in the brain, making it possible to introduce a probe through a small burr hole to the intended target without the need for direct open visualization. The first stereotactic operation was for the treatment of Huntington chorea in which alcohol injections were made into the pallidum and dorsomedian nucleus. Frame-based stereotaxy opened new doors for further exploration of other subcortical targets and ushered in a remarkably innovative period during which a variety of lesioning methods were explored, including chemical, cryo, thermal, physical, and ionizing energy methods. Stereotaxy improved surgical safety, dramatically reducing the 10% to 15% mortality rates previously reported for open approaches to less than 1% by 1950.
Target discovery was the major development of movement disorder surgery during this early exploratory period, and stereotactians focused predominantly on alleviating tremor and rigidity associated with Parkinson’s disease. Based on Meyers’ observations, several groups in the United States developed operations that lesioned the pallidum and/or its associated efferent tracts. Other groups working in France and Germany found that lesion of the motor thalamus, the downstream target of the pallidum, produced complete arrest for virtually any type of tremor, including rest, intention, and postural types. Hassler and Riechert refined the subnuclei nomenclature and boundaries of this part of the ventrolateral thalamus and, together with others, defined and demonstrated the small subnucleus they called the Vim nucleus (Vim) as the most effective antitremor target in the brain. This part of the thalamus links the deep cerebellar nuclei to the motor cortex and still remains the most common target used for the treatment of ET (see later discussion). The demonstrated safety of the stereotactic approach coupled with the discovery of symptom-specific targets set the stage for a short-lived heyday of stereotaxy during a golden period in the 1960s. Surgeons worldwide readily adopted the stereotactic methods as reflected in the large numbers of patients treated. By 1965, approximately 25,000 operations had been performed, and Spiegel estimates that this number increased to approximately 37, 000 by 1969, the same year that Cotzias introduced levodopa.
The Latent Period After the Introduction of Levodopa
During the early 1970s, levodopa advanced as the primary treatment method for disease, and the number of patients referred for surgery declined precipitously. This development, coupled with growing public discussions over psychiatric surgery, led many surgeons to stereotactic interventions altogether by the early 1980s. Only a handful of centers maintained their stereotactic capability through this gloomy period, treating a small number of refractory parkinsonian cases and other types of tremors. However, within a few years of its introduction, the enthusiasm for levodopa therapy was checked by the development of chronic drug-induced side effects. Severe peak-dose dyskinesia and end-dose freezing began to be widely reported in patients with long-term administration of levodopa. Oddly, these so-called on-off effects would be the salvation of modern movement disorders surgery a few years later.
The Stereotactic Revival
In 1992, Laitinen showed that the classic posteroventral pallidotomy not only controlled the cardinal motor manifestation of disease but most extraordinarily also abolished the effects of prolonged levodopa exposure. The finding that an old ablative procedure treated not only the disease but also the problems associate with the side effects of the medicine to treat the disease was something of a renaissance moment for movement disorders surgery. Laitinen’s findings rekindled the movement disorders neurologist’s interest in surgery. At present, the major indication and common time for a surgical referral in patients with Parkinson’s disease occurs at the onset of uncontrolled and unpredictable effects. In addition to Parkinson’s disease, neurologists increasingly began to refer patients with dystonia and the more-difficult-to-treat tremors including poststroke, multiple sclerosis, and ET. This clinical revival of ablative stereotaxy came when deep brain stimulation (DBS) was beginning to gain recognition and, probably to a large extent, was one of the major drivers leading the remarkable success of the modern DBS.
Modern Period of Deep Brain Stimulation
In general, contemporary targets for DBS for both movement disorders and psychiatric indications were derived from the same targets historically used for ablations. However, this recent period has also seen the discovery of novel targets for movement disorders surgery for Parkinson disease in the form of the subthalamic nucleus and the pedunculopontine reticular formation. Although the DBS mechanisms are incompletely understood, high-frequency stimulation (>100 Hz) manifests functionally in the same way as a lesion. Neurosurgeons have, for some time, used intraoperative high-frequency stimulation at the intended target to predict whether a lesion would be effective. The primary practical advantage of DBS over ablative procedures is usually said to be the ability to refine the physiologic postoperative response by changing electrical stimulation parameters. DBS is adjustable and reversible, whereas lesions are not. On the other hand, a well-placed lesion avoids implantation of hardware, concomitant risks of infection, and breakage that are associated with DBS.
Several studies with class I level evidence confirmed the long-term control of the cardinal manifestations of essential and parkinsonian tremor, and in 1997 and 2001, the US Food and Drug Administration approved DBS in the United States for ET and parkinsonian tremor, respectively. Despite its high cost, DBS has now virtually replaced lesion surgery as the dominant stereotactic surgical method in most movement disorders centers; this is in part because of better outcomes when examined head-to-head and also because its seems that traditional radiofrequency lesion surgery carries a higher rate of complications.
Despite several modern refinements in image guidance and target refinement, both conventional lesion surgery and DBS essentially rely on the same basic stereotactic principles introduced in the late 1940s. In particular, both require passage of probes through the skull and intervening brain to the desired target, and even though rates of complication in modern series are low, it may be possible to achieve substantially similar outcomes using completely noninvasive technology. High-energy transcranial focused ultrasound has emerged for the treatment of tremor, and a few proof-of-concept studies ablating the Vim nucleus for ET have been encouraging.
History of movement disorders surgery
Gildenberg describes five major epochs in the evolution of modern movement disorders surgery: (1) the prestereotactic era before 1947, (2) the early stereotactic revolution between 1947 and 1969, (3) the latent period after the introduction of levodopa in the 1970s and 1980s, (4) the stereotactic revival of ablative surgery in the 1990s, and (5) the current modern period of deep brain stimulation. At present, with the advent of high-energy transcranial focused ultrasound, movement disorders surgery may be about to enter a sixth epoch. This article traces the historical progression of movement disorders surgery from early open craniotomy to the so-called incisionless image-guided ultrasound surgery that is now being developed to treat ET. It also describes relevant history of focused ultrasound and a few general principles that have allowed neurosurgeons to treat intractable tremor with acoustic ablation.
The Prestereotactic Era
An early experimental understanding of motor systems began in the late 1800s, when Fritsch and Hitzig conducted the first investigations into mammalian motor circuitry by applying local electrical stimulation to the cortical surface in dogs. Based on this pioneering work, Horsley, in 1909, resected a portion of the contralateral precentral gyrus in a 15-year-old boy for the treatment of postcarlatina hemiathetosis but acknowledged in later reports that these procedures often resulted in severe paralysis and paresis. Hoping to alleviate tremor without weakness, Horsley and Clarke attempted to target specific structures outside primary motor centers, for example, the deep cerebellar nuclei and other subcortical structures. They used the first skull-mounted stereotactic frame using external landmarks to guide slender probes and initiated the first use of discrete electrolytic lesions. The goal of these elegant preclinical investigations in the monkey was to find areas in the brain where small lesions could be accurately placed to control unwanted movements but not abolish movement altogether. This pioneering work in intracranial stereotaxy had to wait until the 1940s to finally be applied to human surgery (see later discussion).
Although Horsley and Clarke laid the groundwork for an understanding of nonprimary motor areas in the brain, other investigators were beginning to study extracranial approaches to abnormal movements. As early as 1908, Foerster reported posterior rhizotomy for control of spasticity and rigidity, leading others to try sympathetic ramisection and various ganglionectomies for similar indications throughout the 1920s and 1930s. During this same period, surgical interest in open craniotomy for ablation of primary cortical structures continued despite permanent loss of function and high mortality. For example, Bucy and colleagues continued to report their series treating athetosis and parkinsonism with ablation of both the supplementary and primary motor cortices despite accruing evidence from Meyers and others that lesions confined strictly to the extrapyramidal system controlled tremor without weakness. Meyers reported excellent tremor control in a patient with hemiparkinsonism by resection of the contralateral caudate head through a transventricular approach, confirming that the basal ganglia is a viable extrapyramidal target for tremor. For other patients, Meyers also explored sectioning of the anterior internal capsule, ansa lenticularis (ansotomy), and internal pallidum. Despite the success of these transventricular extrapyramidal operations, postoperative mortality was never reduced less than 10%, deterring others from adopting similar free-hand transventricular approaches. Nevertheless, Meyers’ contributions clearly showed that basal ganglia lesions could effectively treat tremor without causing paralysis or coma. These decisive observations set the stage for future stereotactic surgical methods in targeting extrapyramidal subcortical structures for the treatment of refractory movement disorders.
The Early Stereotactic Revolution
It was not until after 1947, when Spiegel and colleagues described a procedure to ablate discrete targets in the human brain using a modification of the Horsley-Clarke frame, that the era of stereotactic surgery clinically emerged. The major advantage of their approach was the use of indirect internal landmarks based on ventricular encephalography to identify particular sites in the brain, making it possible to introduce a probe through a small burr hole to the intended target without the need for direct open visualization. The first stereotactic operation was for the treatment of Huntington chorea in which alcohol injections were made into the pallidum and dorsomedian nucleus. Frame-based stereotaxy opened new doors for further exploration of other subcortical targets and ushered in a remarkably innovative period during which a variety of lesioning methods were explored, including chemical, cryo, thermal, physical, and ionizing energy methods. Stereotaxy improved surgical safety, dramatically reducing the 10% to 15% mortality rates previously reported for open approaches to less than 1% by 1950.
Target discovery was the major development of movement disorder surgery during this early exploratory period, and stereotactians focused predominantly on alleviating tremor and rigidity associated with Parkinson’s disease. Based on Meyers’ observations, several groups in the United States developed operations that lesioned the pallidum and/or its associated efferent tracts. Other groups working in France and Germany found that lesion of the motor thalamus, the downstream target of the pallidum, produced complete arrest for virtually any type of tremor, including rest, intention, and postural types. Hassler and Riechert refined the subnuclei nomenclature and boundaries of this part of the ventrolateral thalamus and, together with others, defined and demonstrated the small subnucleus they called the Vim nucleus (Vim) as the most effective antitremor target in the brain. This part of the thalamus links the deep cerebellar nuclei to the motor cortex and still remains the most common target used for the treatment of ET (see later discussion). The demonstrated safety of the stereotactic approach coupled with the discovery of symptom-specific targets set the stage for a short-lived heyday of stereotaxy during a golden period in the 1960s. Surgeons worldwide readily adopted the stereotactic methods as reflected in the large numbers of patients treated. By 1965, approximately 25,000 operations had been performed, and Spiegel estimates that this number increased to approximately 37, 000 by 1969, the same year that Cotzias introduced levodopa.
The Latent Period After the Introduction of Levodopa
During the early 1970s, levodopa advanced as the primary treatment method for disease, and the number of patients referred for surgery declined precipitously. This development, coupled with growing public discussions over psychiatric surgery, led many surgeons to stereotactic interventions altogether by the early 1980s. Only a handful of centers maintained their stereotactic capability through this gloomy period, treating a small number of refractory parkinsonian cases and other types of tremors. However, within a few years of its introduction, the enthusiasm for levodopa therapy was checked by the development of chronic drug-induced side effects. Severe peak-dose dyskinesia and end-dose freezing began to be widely reported in patients with long-term administration of levodopa. Oddly, these so-called on-off effects would be the salvation of modern movement disorders surgery a few years later.
The Stereotactic Revival
In 1992, Laitinen showed that the classic posteroventral pallidotomy not only controlled the cardinal motor manifestation of disease but most extraordinarily also abolished the effects of prolonged levodopa exposure. The finding that an old ablative procedure treated not only the disease but also the problems associate with the side effects of the medicine to treat the disease was something of a renaissance moment for movement disorders surgery. Laitinen’s findings rekindled the movement disorders neurologist’s interest in surgery. At present, the major indication and common time for a surgical referral in patients with Parkinson’s disease occurs at the onset of uncontrolled and unpredictable effects. In addition to Parkinson’s disease, neurologists increasingly began to refer patients with dystonia and the more-difficult-to-treat tremors including poststroke, multiple sclerosis, and ET. This clinical revival of ablative stereotaxy came when deep brain stimulation (DBS) was beginning to gain recognition and, probably to a large extent, was one of the major drivers leading the remarkable success of the modern DBS.
Modern Period of Deep Brain Stimulation
In general, contemporary targets for DBS for both movement disorders and psychiatric indications were derived from the same targets historically used for ablations. However, this recent period has also seen the discovery of novel targets for movement disorders surgery for Parkinson disease in the form of the subthalamic nucleus and the pedunculopontine reticular formation. Although the DBS mechanisms are incompletely understood, high-frequency stimulation (>100 Hz) manifests functionally in the same way as a lesion. Neurosurgeons have, for some time, used intraoperative high-frequency stimulation at the intended target to predict whether a lesion would be effective. The primary practical advantage of DBS over ablative procedures is usually said to be the ability to refine the physiologic postoperative response by changing electrical stimulation parameters. DBS is adjustable and reversible, whereas lesions are not. On the other hand, a well-placed lesion avoids implantation of hardware, concomitant risks of infection, and breakage that are associated with DBS.
Several studies with class I level evidence confirmed the long-term control of the cardinal manifestations of essential and parkinsonian tremor, and in 1997 and 2001, the US Food and Drug Administration approved DBS in the United States for ET and parkinsonian tremor, respectively. Despite its high cost, DBS has now virtually replaced lesion surgery as the dominant stereotactic surgical method in most movement disorders centers; this is in part because of better outcomes when examined head-to-head and also because its seems that traditional radiofrequency lesion surgery carries a higher rate of complications.
Despite several modern refinements in image guidance and target refinement, both conventional lesion surgery and DBS essentially rely on the same basic stereotactic principles introduced in the late 1940s. In particular, both require passage of probes through the skull and intervening brain to the desired target, and even though rates of complication in modern series are low, it may be possible to achieve substantially similar outcomes using completely noninvasive technology. High-energy transcranial focused ultrasound has emerged for the treatment of tremor, and a few proof-of-concept studies ablating the Vim nucleus for ET have been encouraging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree