Pelvic bone metastases frequently result in severe pain and disability. Open surgical reconstruction is associated with a high complication and mortality rate. Percutaneous screw fixation is a minimally invasive treatment that is safe and effective for the management of periacetabular metastases. This article details our technique for pelvic screw fixation, including (1) perioperative care, (2) navigation and needle guidance, (3) access, (4) biopsy and ablation, (5) screw placement, and (6) cement augmentation.
Introduction
Bone metastases are the most common cause of cancer pain and result in significant morbidity. On average, skeletal-related events (eg, pathologic fracture) occur every 3 to 6 months, clustering around progression of disease and reduced treatment options. The pelvis is the second most common site of bone metastases after spine and is a major source of disability.
Treatment goals for pelvic bone metastases are predominantly palliative. Nonacetabular pathologic fractures (eg, iliac crest and inferior pubic ramus) are often managed nonoperatively, including bisphosphonates, systemic and radiation therapy. Open surgical reconstruction typically involves variations of total hip arthroplasty (THA), including THA augmentation with cement, pins (eg, Harrington procedure), or antiprotrusio cages. Although these constructs can last the lifetime of the patient, the overall complication and mortality rate is high and should be reserved for patients whose life expectancy is not significantly limited due to cancer. Additionally, if the hip joint is uninvolved, arthroplasty may not be required if pelvic disease is controlled. Over the last several years, percutaneous fixation has emerged as a safe and effective treatment for management of periacetabular pathologic fractures. Compared to open surgical reconstruction, this minimally invasive approach offers less operative time, less blood loss, allows for early weight-bearing, and independently stabilizes both anterior and posterior acetabular columns. Perhaps most importantly, a less invasive approach affords continuation of systemic and radiation therapy.
Patient selection
Patients with periacetabular metastases typically report groin or deep buttock pain worse with standing or walking. This is usually secondary to a lytic defect and/or pathologic fracture involving the ilium, ischium or superior pubic ramus. This functional pain contrasts with tumor pain, which is present at rest and/or at night. While tumor pain may respond well to ablation, radiation, or systemic therapy, structural pain requires a structural solution (eg, screws, cement). Functional status is often significantly impaired and can be quantitatively assessed using the validated Patient-Reported Outcomes Measurement Information System (PROMIS) questionnaire. In the absence of significant hip articular surface disruption or acetabular protrusion, percutaneous screw fixation is indicated for patients with mechanical pain secondary to periacetabular metastases. Ablation is usually combined with internal fixation in patients with active disease and/or tumor pain. Contraindications include uncorrectable coagulopathy and infection. Primary bone sarcoma is a relative contraindication as surgical resection is considered the gold standard.
Preoperative planning
Structural assessment
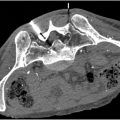
Bone quality and fracture morphology is best assessed with computed tomography (CT). CT abdomen/pelvis performed as part of patient’s routine cancer surveillance imaging is usually used. In patients who have not had imaging within 1 month of procedure, CT pelvis without contrast is obtained. Magnetic resonance imaging (MRI) is sometimes useful to assess large soft tissue masses, joint invasion, and neurovascular structures, and is ordered on a case-by-case basis. There are several anatomic classification systems for metastatic disease of the pelvis, including the modified Harrington system and metastatic acetabular classification (MAC). , While these systems provide a useful paradigm for grading disease extent about the acetabulum, they are rarely used formally in practice. Rather, localization of pathologic fractures into either anterior and/or posterior columns is the standard. This simple approach relies on 3 potential screw corridors for periacetabular lesion stabilization: anterior column screw (ramus screw), posterior column screw (ischial screw), and trans-columnar screw (anterior-posterior screw from anteroinferior iliac spine to posterosuperior iliac spine) ( Fig. 1 ). The goal is to structurally connect the leg to the spine and prevent acetabular protrusio. When a structural defect or pathologic fracture is identified in any one of these corridors, a screw should be placed across that corridor. When all 3 screws are placed, a tripod configuration is conferred, which reinforces the mechanical axis of the acetabulum ( Fig. 2 ). If disease progresses, a tripod screw fixation can subsequently be converted to a THA ( Fig. 3 ).



The quality of bone surrounding a lytic defect or pathologic fracture is important for determining feasibility and approach for screw placement. With underlying lytic disease coupled with systemic therapies and radiation, bone quality is often severely degraded. The goal of screw fixation is to fasten 2 segments of bone across a fracture site and eliminate abnormal internal movement with weight-bearing. Therefore, the screw trajectory must be carefully planned to ensure good bicortical purchase on both sides of the fracture. While bicortical fixation is ideal, it is frequently not possible in the setting of lytic tumors. In such cases, cement augmentation is utilized on 1 or both sides of the defect to anchor the screw into the diseased bone. In patients with large expansile lytic defects or nonlinear screw corridor, an expandable photodynamic stabilization balloon implant (IlluminOss, East Providence, RI) may be indicated, which is often combined with locking screws ( Fig. 4 ). In contrast, fractures that are sclerotic either because of tumor type (eg, prostate cancer) or post radiation changes, cement augmentation is not necessary. Access and drilling techniques however may require modification to overcome challenges related to dense sclerotic bone.

Equipment
Percutaneous screw fixation uses essentially a Seldinger technique modified for bone: needle, guide wire (K-wire), dilator (reaming drill), and device placement over wire (screw). For needle, we use a standard 8g bone access cannula with diamond tip stylet. A beveled stylet is frequently used to adjust needle trajectory along desired path. For K-wire, drill, and screws, there are various manufacturer options with slight variation in instrumentation. We have used several of these, including DePuy Synthes cannulated screws (Raynham, MA), Zimmer cannulated screw system (Warsaw, IN), OsteoCentric cannulated fastener system (Austin, TX), and Stryker ASNIS III cannulated screw system with Stryker System 8 Power (Stryker, Kalamazoo, MI). Instrument tray includes K-wire, drill, direct measuring gauge, and cannulated hand screwdriver. In addition, we created a small custom tray with basic instruments, including needle drivers, clamps, mallet, forceps, etc. We predominantly use the 3.2 mm × 300 mm threaded K-wire, which is short enough to allow space for cone beam CT after placement. While threaded tip K-wire allows for better bone purchase and reduced chance for migration, smooth tip K-wire is less difficult to remove and often easier to redirect or “bounce” off of cortical bone to continue down a corridor (eg, superior pubic ramus). Although screws are self-drilling, we typically ream (eg, create a pilot hole) the length of the screw tract prior to screw placement. Screws are also self-tapping and only rarely in hard sclerotic bone will we use a cannulated tap to cut threads into the bone prior to screw insertion.
We prefer 8.0 mm diameter stainless steel screws if anatomy allows, though will place as small as 4.5 mm screws depending on space within the corridor, with attention to the hip joint, adjacent cortex and other intersecting screws. Our screw caddy includes lengths ranging from 40 to 120 mm with optional tray for lengths 130 to 180 mm. We frequently use fully-threaded screws to obtain as much purchase as possible on both sides of the fracture given diseased bone. If there is fracture distraction and sufficient tract length, then we sometimes use partially-threaded screws.
Anesthesia
We perform percutaneous screw fixation under general anesthesia. Immobilization of the patient is important to prevent needle guidance mis-registration during the procedure. Given fixation within the pelvis, a foley catheter is placed to decompress the bladder in case of inadvertent violation of the inner table of the pelvis.
Preoperative antibiotics include weight-based cefazolin or clindamycin if there is a penicillin allergy. Multimodal pain medications include acetaminophen 1 g IV, dexamethasone 8 mg IV, and ketorolac 15 mg IV. Bupivacaine 0.25% is used intraoperatively at the periosteum at the time of bone access.
Patient positioning and preparation
Patient positioning is determined by planned screw placement. If an ischial screw is planned, prone positioning is required. Technically, ramus and anterior-posterior screws can be placed in either supine or prone positioning. Despite that, we prefer prone positioning for ramus screws, especially in women with gynecoid pelvic type, which can make it difficult to achieve bicortical fixation using a retrograde approach (eg, pubic tubercle access). In addition, a retrograde approach can be challenging in a man given the proximity of the base of the penis and spermatic cord. Given the superficial location, this pubic area is also more to prone to hematoma and post procedure pain. Therefore, unless performing trans-columnar screw fixation only, we typically position patients prone.
Patient preparation is critical for successful procedure. For either supine or prone positioning, we use a pelvic raising operative positioner (BoneFoam, Corcoran, MN). The positioner elevates the pelvis off the procedure table to allow for easier access, especially for ischial screw placement. This should be secured to the table to avoid movement during the procedure. The patient’s head is brought to the very top of the procedure table and the arms are at the side without arm boards. We use a cross-wise sheet from the top of the shoulder to the hands of the patient with padding to support the patients arms. The sheet is then either tucked between the arm and the torso or wrapped asymmetrically to the upper torso. A Velcro strap is used for the upper torso as well as at the thighs to prevent any movement of the pelvis. Foam padding is used for the knees and pillow under the ankles with Bair Hugger (3M, Maplewood, MN) and sequential compression devices in place. A wide field including all access sites is draped using Steri-Drape 1010 (3M, Maplewood, MN). This often extends from the ribs down to the proximal thigh. At this point and before sterile prep, we will typically perform cone beam CT. While cone beam CT is reviewed and needle trajectories are planned in the control suite, the field is sterilely prepped, including Ioban antimicrobial impregnated adhesive drape (3M, Maplewood, MN). Standard half drape and femoral drapes are used with sterile covers for the fluoroscopy unit ( Fig. 5 ). Whenever a cone beam CT is performed during the procedure (eg, screw length measurement), a half drape is placed over the procedure field.