Abstract
Acquired thrombotic thrombocytopenic purpura (TTP) is a rare haematological emergency characterised by severe ADAMTS13 deficiency, leading to thrombotic microangiopathy and multiorgan dysfunction. Posterior reversible encephalopathy syndrome (PRES) is a neurological disorder associated with endothelial dysfunction, often secondary to uncontrolled hypertension or autoimmune conditions. We present a case of a 22-year-old male who presented with vomiting, headache, and right upper limb weakness, followed by a hypertensive crisis and generalised seizures. Initial investigations revealed severe thrombocytopenia, microangiopathic hemolytic anaemia, and acute kidney injury, raising suspicion for thrombotic microangiopathy. MRI findings confirmed PRES, while the presence of schistocytes and markedly reduced ADAMTS13 activity led to the diagnosis of acquired TTP. The patient was treated with plasma exchange, immunosuppressive therapy, corticosteroids, and antihypertensive agents. Despite aggressive management, the disease progressed to multiorgan failure, and the patient succumbed to the illness. This case highlights the fatal interplay between TTP and PRES, emphasising the need for early recognition and timely intervention. The coexistence of these 2 rare conditions presents a diagnostic and therapeutic challenge, underscoring the importance of prompt plasma exchange and immunosuppressive therapy in such critically ill patients.
Background
Thrombotic thrombocytopenic purpura (TTP) is a rare but life-threatening thrombotic microangiopathy characterised by severe thrombocytopenia, microangiopathic hemolytic anaemia, and multiorgan dysfunction due to disseminated microvascular thrombosis [ ]. The disease is caused by a severe deficiency of ADAMTS13, a von Willebrand factor-cleaving protease, leading to the accumulation of ultra-large von Willebrand factor (vWF) multimers and excessive platelet aggregation in the microcirculation [ ]. The deficiency of ADAMTS13 can be congenital (Upshaw-Schulman syndrome) due to genetic mutations in the ADAMTS13 gene or acquired, which is primarily due to autoantibody-mediated inhibition of ADAMTS13 activity [ ]. Acquired TTP is the predominant form and is frequently associated with autoimmune diseases, malignancies, pregnancy, infections, and certain medications [ ]. The incidence of acquired TTP is estimated to be 3–6 cases per million per year, with a higher prevalence among females and young adults [ ]. Without appropriate treatment, the mortality rate exceeds 90%; however, with early intervention, including plasma exchange and immunosuppressive therapy, the survival rate improves significantly, exceeding 80% [ ].
Neurological manifestations are common in TTP, occurring in over 50% of cases, and range from mild confusion to seizures and coma due to microvascular thrombosis and endothelial injury [ ]. One of the severe neurological complications associated with TTP is posterior reversible encephalopathy syndrome (PRES), a disorder characterized by reversible vasogenic oedema due to endothelial dysfunction [ ]. PRES is commonly associated with hypertensive encephalopathy, autoimmune disorders, renal dysfunction, and cytotoxic treatments and presents clinically with headaches, visual disturbances, altered mental status, and seizures [ ]. Magnetic resonance imaging (MRI) findings typically demonstrate symmetrical hyperintensities in the parieto-occipital regions, consistent with vasogenic oedema [ ]. The pathophysiology of PRES involves endothelial dysfunction, breakdown of the blood-brain barrier, and dysregulation of cerebral autoregulation, leading to vasogenic edema and neurological impairment [ ].
The coexistence of TTP and PRES is rare but poses significant diagnostic and therapeutic challenges due to their overlapping pathophysiology, both involving endothelial dysfunction and microvascular injury. PRES in TTP may result from severe hypertension, endothelial damage, and thrombotic microangiopathy, leading to increased cerebrovascular permeability and oedema formation [ ]. Studies have reported cases of PRES occurring in the setting of TTP, particularly in patients with hypertensive crises and acute kidney injury [ ]. While PRES is typically reversible with blood pressure control and resolution of the underlying pathology, delayed recognition or persistent endothelial injury can lead to permanent neurological deficits or mortality [ ].
This case report presents a young male with acquired TTP complicated by PRES, manifesting as hypertensive encephalopathy and recurrent seizures. The case highlights the fatal interplay between these 2 rare conditions and underscores the importance of early diagnosis, aggressive plasma exchange, and immunosuppressive therapy. Despite the availability of effective treatment strategies, the presence of PRES in TTP significantly worsens prognosis, necessitating close monitoring and prompt intervention to improve clinical outcomes.
Case presentation
A 22-year-old male was brought to the emergency department by his relatives with complaints of recurrent vomiting, headache, and right upper limb weakness. The vomiting was nonprojectile, nonfoul-smelling, and nonbilious, containing food particles. The headache was described as dull in nature, localized to the bitemporal and occipital regions. The patient had no history of seizures, loss of consciousness, trauma, fever, recent infections, or similar complaints in the past. His medical and family history was unremarkable, with no known hereditary or autoimmune conditions. He was initially admitted to the neurology department for further evaluation.
On arrival at the emergency room, the patient was hemodynamically stable but hypertensive, with a blood pressure of 170/100 mmHg. His respiratory rate was 22 breaths per minute, and oxygen saturation was maintained at 99% on room air. The pulse rate was recorded at 88 beats per minute. Initial systemic examination findings were unremarkable for the cardiovascular, respiratory, and gastrointestinal systems. However, on neurological examination, the patient was drowsy but arousable. He followed verbal commands appropriately, and his Glasgow Coma Scale (GCS) score was 15/15. The pupils were bilaterally equal and reactive to light. The most notable finding was mild weakness in the right upper limb, while the rest of the neurological examination was within normal limits. Given his hypertensive state and neurological symptoms, a comprehensive diagnostic workup was initiated, and the patient was started on conservative management.
Laboratory investigations upon admission revealed anaemia with a haemoglobin level of 8 g/dL and thrombocytopenia with a platelet count of 0.70 × 10⁶ cells/cumm. White blood cell counts were within normal limits. Biochemical analysis showed elevated urea (113 mg/dL) and creatinine (4.9 mg/dL), suggestive of acute kidney injury. The liver function tests showed mildly elevated alanine transaminase (ALT) levels at 80 IU/L, with normal aspartate transaminase (AST) and alkaline phosphatase levels. Serum LDH was significantly elevated at 1403 IU/L, raising suspicion of hemolysis. Urinalysis showed 2+ albuminuria, with a urine protein/creatinine ratio of 5.9 mg/mg and 24-hour urinary protein excretion of 8674 mg/day, indicating severe proteinuria. Electrolyte levels were within normal ranges, and the coagulation profile, including prothrombin time (PT), activated partial thromboplastin time (APTT), and international normalized ratio (INR), showed no major abnormalities. These findings pointed towards potential thrombotic microangiopathy, warranting further investigations.
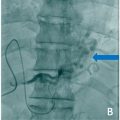
On the second day of hospitalization, the patient developed 2 episodes of generalized tonic-clonic seizures. There was no preceding aura, and postictal confusion was noted following each episode. A computed tomography (CT) scan of the brain was performed immediately but showed no acute intracranial abnormalities Fig. 1 . An electroencephalogram (EEG) revealed a diffuse spike-and-wave pattern consistent with generalized seizure activity. Given the hypertensive state and new-onset seizures, an MRI of the brain was conducted, which showed hyperintense lesions involving the cortical and subcortical regions of the bilateral occipito-parieto-frontal areas, cerebellar hemispheres, pons, and right lentiform nucleus. These findings were highly suggestive of PRES, a condition commonly associated with hypertensive encephalopathy and thrombotic microangiopathy.