Entrapment neuropathies are the result of compression, displacement, traction, or irritation of peripheral nerves due to anatomic and/or dynamic factors at specific anatomic sites. This article reviews the current magnetic resonance neurography techniques, image evaluation considerations, and specific features of ulnar, median, and radial nerve entrapments at the most common locations at the elbow, forearm, and wrist.
Key points
- •
Entrapment neuropathies are the most common cause for neuropathic pain and appear in narrow anatomic areas.
- •
Magnetic resonance neurography (MRN) is the technique that enables a selective multiplanar evaluation of the nerves. A complete MRN protocol typically includes 2D T1-weighted and T2-weighted fat-suppressed sequences, 3D isotropic sequences, and diffusion-weighted sequences.
- •
A systematic evaluation of the nerve must include the assessment of signal intensity, the trajectory and possible discontinuities, the fascicular pattern, the changes in diameter, and the perineural fat.
- •
The muscle denervation in entrapment neuropathies may be acute, subacute, or chronic, and the MR findings vary from edema in the acute phase to fatty degeneration and atrophy in chronic phases.
- •
The newly developed reporting, interpretation, and classification system based on MRN (Neuropathy score reporting and data system) improves the multidisciplinary communication for MRN imaging diagnoses.
| AI | artificial intelligence |
| AIN | anterior interosseous nerve |
| CTS | carpal tunnel syndrome |
| CuTS | cubital tunnel syndrome |
| DWI | diffusion-weighted |
| MRN | magnetic resonance neurography |
| NS-RADS | neuropathy score reporting and data system |
| PIN | posterior interosseous nerve |
| SRN | superficial radial nerve |
| UTS | ulnar tunnel syndrome |
Introduction
Entrapment neuropathies are the result of compression, displacement, traction, or irritation of peripheral nerves due to anatomic and/or dynamic factors at specific anatomic sites. Entrapment of a peripheral nerve appears in narrow areas in which the nerve usually crosses a so-called tunnel formed by different structures (bones, ligaments, and muscles). When the tunnel is narrowed due to various structural causes the nerve is compressed. The resulting repetitive injuries are followed by nerve enlargement and fibrosis around the nerve leading to a further relative narrowing of the area and an exacerbation of the condition. ,
Entrapment neuropathies are the most common cause for neuropathic pain. The diagnosis is based on a thorough assessment of the personal medical history and physical examination, electrophysiological tests, and different imaging techniques. Ultrasonography and MR imaging are routinely used in clinical practice. High-resolution ultrasonography is a cost-efficient technique that is especially useful in cases in which the nerve is superficial and when the main cause of entrapment is a dynamic one. However, the technique does not provide a large enough panoramic view of the anatomic area, identifies the muscle denervation changes much later than MR imaging, and is highly operator-dependent. Magnetic resonance neurography (MRN) is defined as the technique that enables a selective multiplanar evaluation of the nerves using tailored protocols. The information provided by MRN may confirm nerve structural changes, secondary abnormalities of the innervated muscles, and identify the cause of the impingement. Recently, artificial intelligence (AI) has shown an increased role in the field of peripheral nerve pathology. AI has the potential not only to improve the quality of the images in a significantly shorter examination time but also to provide valuable information for the referring clinician (eg, reconstruction of the nerve course) and to address the segmentation of specific anatomic sites of nerve entrapments.
This article reviews the current MRN techniques, image evaluation considerations, and specific features of the ulnar, median, and radial nerves entrapment at the most common locations at the elbow, forearm, and wrist.
Magnetic resonance neurography technique
MRN should be performed with the purpose of confirming nerve involvement, identifying causes responsible for entrapment, and evaluating muscle denervation.
When choosing an MRN protocol one must consider several factors. First, the appropriate coil must be chosen according to the anatomy of the region to obtain the best contrast-to-noise ratio and the highest resolution. The axial planes (perpendicular to the nerve trajectory) represent the foundation of MRN examinations. Sagittal or coronal planes may add additional information. A complete MRN protocol typically includes two-dimensional (2D) T1-weighted and T2-weighted fat-suppressed sequences, three-dimensional (3D) isotropic sequences and diffusion-weighted (DWI) sequences ( Table 1 ). Since postcontrast T1-weighted sequences do not usually provide more information, they are not routinely used. The information summarized in Table 1 comprises the most used sequences and their contribution to MRN interpretation. The field-of-view should be adjusted to cover the entire anatomic area of interest, including at least a partial visualization of the innervated muscles. However, at the same time, the field-of-view should be tailored to be as small as reasonably possible to avoid either low-resolution or long examination times. Nowadays, by using AI capabilities at the time of acquisition, a complete MRN examination can be performed in much shorter examination times and AI segmentation enables the longitudinal reconstruction of the entire nerve course in seconds.
| Basic Sequences | Contribution in Nerve Assessment |
|---|---|
| 2D T1-weighted |
|
| 2D PD weighted |
|
| T2-weighted fat-suppressed (preferable with high TE values) OR STIR sequences (more homogeneous but lower SNR) |
|
| Optional sequences | |
| 3D isotropic T2 fat-suppressed |
|
| DWI/DTI |
|
| DESS-WE or similar MR sequences (vendor-specific) |
|
Imaging evaluation—general considerations
The evaluation of MRN images for potential nerve entrapment should be focused on 2 different entities: the nerve and the innervated muscles. Sometimes the diagnosis may be implicated by knowing the corresponding innervated area of the nerve.
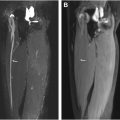
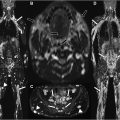
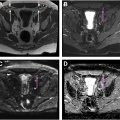
A systematic evaluation of the nerve includes the assessment of signal intensity, of the trajectory, the fascicular pattern, the diameter, and the perineural fat. The damage at the entrapment site is followed by edema and hyperemia, which translates into an increased signal intensity of the nerve on T2-weighted images (higher than the muscles and similar to the venous vessels). The length of the pathologic signal intensity should also be reported since the increased nerve signal may extend both proximal and distal to the compression site. In severe nerve entrapments, the nerve demonstrates a decreased T2-weighted signal at the point of entrapment with increased T2-weighted signal proximal and distal to the entrapment point known as the triple B sign (bright, black, bright nerve). On DWI, the affected nerve shows an increase in water mobility and this increased signal might be more sensitive than T2-weighted fat-suppressed images having a higher correlation with the electrophysiological studies. In patients with chronic entrapment neuropathies, the hyperintense signal may persist for a long period of time after the original condition is back to normal and the clinical symptoms are no longer present. Meandering, discontinuities, or changes of the normal nerve course may be seen. Commonly, the affected nerve loses the normal fascicular pattern and is enlarged or flattened near the compression. However, in prolonged cases of entrapment, the nerve may become atrophic as a result of perineural fibrosis. Special attention should be given to the perineural fat planes and prominent vessels around the nerve.
Muscle denervation in entrapment neuropathies may be acute, subacute, or chronic ( Table 2 ). Unlike electromyography that may be normal up to 2 to 3 weeks after the onset of the nerve lesion, the muscle edema is identified on MR imaging as early as 3 to 5 days after the injury. Nerve and muscle changes may not always be present at the same time depending on the specific anatomic area and the underlying etiology. Therefore, knowing the group of muscles innervated by a specific nerve may guide the diagnosis to a specific nerve location.
| Neuropathy Score Reporting and Data System Class, Subclass | Description |
|---|---|
| 0 | Incomplete imaging set or nondiagnostic study |
| U | Normal or unremarkable study |
| E (nerve entrapment) | |
| E1 | Mild: mild focal or short-segment nerve hyperintensity on T2-weighted imaging at the entrapment site |
| E2 | Moderate: moderate focal or short-segment nerve hyperintensity on T2-weighted imaging, with proximal enlargement and flattening at the entrapment site |
| E3 | Severe: focal or short-segment nerve hyperintensity on T2-weighted imaging with proximal enlargement, flattening at the entrapment site and distal enlargement |
| M (muscle abnormality) | |
| M0 | Normal |
| M1 | Acute phase: <4 wk. Neurogenic edema due to capillaries enlargement MR imaging: Diffuse T2 fat-suppressed hyperintense signal |
| M2 | Subacute phase: 4 wk–1 y. Edema and fatty atrophy (fibers degeneration and development of subsarcolemmal vacuoles) and mild muscle atrophy MR imaging: T2 fat-suppressed hyperintense signal mixed with T1 hyperintense signal due to fatty replacement |
| M3 | Chronic phase: more than 1 y. Partial or complete fatty replacement and moderate to severe atrophy MR imaging: Reduced muscle volume and T1-weighted hyperintense signal |
| MNOS | Known muscle denervation, unsure about denervation or myopathy |
| PI or surgical cases | |
| PI1 | Near normal |
| PI2 | Possible persistent neuropathy |
| PI3 | Definitely persistent or worsening neuropathy |
Several different classification systems are used for grading nerve injuries aimed at optimizing treatment decisions. Most of them are based on morphopathological criteria, using correlation with electrophysiological tests (Seddon grading) or with prognosis and need for surgery (Sunderland grading). , However, exclusive use of the aforementioned classification systems for radiology reporting is incomplete. There is important information that is not included in these classifications (eg, exact location of the lesion, the nerve caliber, the nerve trajectory, the underlying cause of compression, and the neuromuscular changes). To fill in the missing gaps and provide additional guiding information, a new standardized reporting, interpretation, and classification system (neuropathy score reporting and data system, NS-RADS) was proposed by Chhabra and colleagues (see Table 2 ).
Upper extremity nerve anatomy
The median, radial, and ulnar nerves may be entrapped at various locations. The median nerve originates from the medial cord (C5-7) and the lateral cord (C8-T1) of the brachial plexus and descends along the arm close to the brachial artery. It provides motor and sensory innervation to the flexor muscles of the forearm and hand ( Tables 3 and 4 ). The radial nerve originates from the C5-T1 posterior cord and is situated at the upper arm level close to the humerus, between the long and the medial head of the triceps. It provides motor and sensory innervation to muscles of the forearm, wrist, the dorsal hand, and fingers. The ulnar nerve is formed from C8-T1 dorsal rami, passing along the medial upper arm. It provides motor innervation to muscles responsible for flexing the wrist and fingers and sensorial innervation to the hypothenar muscle.
| Entrapment Location | Causes | Affected Areas/Muscles | |
|---|---|---|---|
| Median nerve Largest diameter in asymptomatic subjects: 5.00 mm | |||
| Supracondylar process syndrome | Elbow : distal humerus |
|
|
| Pronator syndrome | Elbow : at the level of pronator teres muscle |
|
|
| Anterior interosseous nerve syndrome (Kiloh-Nevin syndrome) | Elbow : anteriorly, distal to the articular line |
|
|
| Ulnar nerve Largest diameter in asymptomatic subjects: 4.00 mm | |||
| CuTS | Elbow : cubital tunnel |
|
|
| Radial nerve Largest diameter in asymptomatic subjects: 5.00 mm | |||
| Radial and posterior interosseous nerve syndrome (radial tunnel syndrome, deep radial nerve syndrome, or supinator syndrome) | Proximal forearm : supinator tunnel |
|
|
| Superficial radial nerve syndrome (Wartenberg syndrome) | Distal forearm : proximal two-thirds to distal one-third of the forearm |
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree