Abstract
A 45-year-old male with chronic hepatitis B presented with an advanced hepatocellular carcinoma (HCC) occupying the entire left liver and invading the left portal vein. Despite multiple poor prognostic imaging features, including vascular invasion, corona enhancement, an incomplete capsule, intratumoral necrosis, intratumoral arteries, and irregular tumor borders, the patient elected to undergo a left hepatectomy. Although Barcelona Clinic Liver Cancer (BCLC) staging classified the case as stage C, a resection was successfully performed. Remarkably, 6 years postsurgery, the patient remains recurrence-free. This report highlights a rare, fortunate outcome in a high-risk HCC case and underscores the potential of surgical intervention even in advanced HCC.
Introduction
Hepatocellular carcinoma (HCC) remains a leading cause of cancer-related mortality worldwide, particularly in patients with chronic hepatitis virus infection and cirrhosis [ ]. Typically, patients with advanced HCC and poor prognostic features on imaging are considered candidates for systemic therapy rather than resection [ ]. However, in select cases, surgical resection may provide a unique opportunity for extended survival, even in advanced disease stages [ ].
We report on a case with BCLC stage C HCC, who, despite extensive tumor involvement and portal vein invasion, underwent a left hepatectomy without postoperative adjuvant therapy and remains recurrence-free 6 years postsurgery. This case underscores the importance of individualized treatment decisions and the potential for positive outcomes in high-risk cases.
Case presentation
A 45-year-old male with a history of chronic hepatitis B virus (HBV) infection presented to our hospital with complaints of epigastric discomfort and weight loss over the past few months. His liver function tests were within acceptable limits (AST 61 U/L, ALT 39 U/L, serum albumin 39.3 g/L, total bilirubin 15.06 µmol/L, INR 1.04), placing him in the Child–Pugh A category. Alpha-fetoprotein (AFP) levels were also within the normal range at 6.4 ng/mL. Initial abdominal ultrasound detected a large mass in the left liver, raising suspicion of malignancy. Subsequent multiphase contrast-enhanced CT revealed an extensive HCC occupying the entire left liver with invasion of the left portal vein, along with multiple poor prognostic imaging features. Despite these findings, the patient expressed a strong preference for surgical intervention.
After a multidisciplinary discussion, the decision was made to proceed with a left hepatectomy. The patient tolerated the surgery well, with no postoperative complications. Histopathological examination of the resected liver confirmed a moderate differentiated HCC with vascular invasion and negative resection margins ( Fig. 3 ). He has been closely monitored postoperatively and followed up for 6 years, during which imaging confirmed no evidence of residual or recurrent disease.
Imaging findings
Multiphase contrast-enhanced CT provided a comprehensive view of the tumor’s characteristics, which indicated an advanced stage with poor prognostic markers.
- •
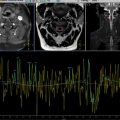
Tumor size and location: Imaging revealed a large hepatic mass occupying the entire left lobe, specifically involving segments II, III, and IV. The tumor measured approximately 12 × 10 × 9 cm and was notably expansive, filling the entire anatomical space of the left lobe ( Fig. 1 ).

Fig. 1
Contrast-enhanced CT scan revealed a large, necrotic HCC occupying the entire left liver lobe with invasion into the left portal vein. Axial (A, B) and coronal (C, D) reconstructions depicted the arterial phase (A, C) and portal venous phase (B, D). The mass (M) demonstrated characteristic features of HCC, including arterial phase hyperenhancement and washout, consistent with LI-RADS 5. Tumor invasion was evident within the entire left portal venous system (yellow arrow, A-C), sparing the right and main portal veins. Despite its size, the tumor remained confined to the left liver lobe, displacing the middle hepatic vein towards the right (white arrow, D). Areas of necrosis within the tumor were apparent as nonenhancing hypodense regions (white arrow, B). Additionally, a structure adjacent to the left adrenal gland, presumed to be residual splenic tissue from a prior splenectomy, was visible (A, B) and remained stable in postoperative imaging, ruling out metastasis.
- •
Vascular invasion: The mass was seen infiltrating the left portal vein, indicating direct vascular involvement. This invasion of the portal vein appeared as an extension of tumor tissue within and expanding the vessel lumen, presenting as a filling defect with partial enhancement. The tumor, however, did not invade the right and main portal veins ( Fig. 1 ).
- •
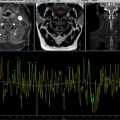
Corona enhancement: The arterial phase images demonstrated corona enhancement around the tumor, which appeared as an area of hyperenhancement adjacent to the tumor’s outer edges and became isodense in later phases ( Fig. 2 ).

Fig. 2
Axial contrast-enhanced CT scan illustrated additional prognostic imaging features, including corona enhancement, intratumoral arteries, irregular borders, and incomplete capsulation. Corona enhancement appeared as a hyper-enhanced area adjacent to the tumor (M) in the arterial phase (yellow arrow, A), becoming isodense in the portal venous phase (yellow arrow, B). Tumor borders were better depicted in portal venous phase images (solid blue line, B). Maximum intensity projection imaging in the arterial phase revealed multiple intratumoral arteries (white arrow, C). Delayed-phase imaging showed regions of enhancing tumor capsule (solid blue line, D) alongside areas with irregular borders and incomplete capsulation (dashed white line, D).

Fig. 3
Postoperative pathological examination revealed features consistent with moderately differentiated HCC. The tumor is composed of hepatocytes with hyperchromatic, pleomorphic nuclei, prominent nucleoli, and abundant, granular eosinophilic cytoplasm (M). Numerous mitoticures are observed. These tumor cells are arranged in trabecular or solid patterns. Lymphovascular invasion is present (L). No malignant cells are observed at the resection margin. No evidence of cirrhosis is present in the nontumorous liver tissue.
- •
Capsular incompleteness: The lesion displayed incomplete capsulation on imaging, where certain portions of the tumor margin lacked a defined enhancing capsule. The areas without a complete capsule appeared irregular and less demarcated compared to portions with capsular tissue, giving the tumor a partly uncontained appearance ( Fig. 2 ).
- •
Intratumoral necrosis: Central regions within the tumor showed areas of necrosis, appearing as nonenhancing zones within the mass. This necrotic tissue presented as a hypodense area on contrast-enhanced imaging, indicating sections where the tumor tissue had undergone degeneration ( Fig. 1 ).
- •
Intratumoral arteries: Multiple intratumoral arteries were identified within the mass, visualized as discrete, branching vessels coursing through the tumor in arterial phase imaging. These arteries appeared hyperdense relative to surrounding tissue and to the lesion’s enhancing parts ( Fig. 2 ).
- •
Irregular tumor borders: The tumor margins were irregular and infiltrative, with jagged edges that extended unevenly into surrounding liver tissue. This irregular contour was evident in both axial and coronal planes, giving the mass a less defined and invasive appearance ( Fig. 2 ).
The constellation of these imaging findings painted a picture of an aggressive, high-risk HCC. Nonetheless, a left hepatectomy was performed without postoperative adjuvant therapy, and the patient has maintained a recurrence-free status 6 years postsurgery. A contrast-enhanced CT scan performed 1.5 years postsurgery confirmed the absence of residual disease after left hepatectomy ( Fig. 4 ). Regular follow-up with abdominal ultrasound and AFP monitoring has consistently shown stable and normal results.