Abstract
Heterotopic cervical ectopic pregnancy (CEP) is a rare form of ectopic pregnancy, that involves implantation of gestational sac in both the cervical canal and uterine cavity. This condition poses high risks of severe complications like lethal vaginal bleeding and abortion. Transvaginal ultrasonography is the primary diagnostic tool. Risk factors may vary from prior cesarean delivery to the utilization of Assisted Reproductive Technologies (ART). Despite the research conducted on this condition, the best treatment strategy has not been established. This study discusses a rare case of cervical heterotopic pregnancy, emphasizing early diagnosis. Our case underwent in-vitro fertilization (IVF). We used potassium chloride (KCL) and methotrexate (MTX) as treatment. At first, the cervical gestational sac was expelled but unfortunately, later, the intrauterine gestational sac was also aborted. We also reviewed 25 cases (1980-2024) which demonstrated the importance of early diagnosis of heterotopic cervical pregnancy and that most cases are likely to have positive outcomes.
Introduction
Ectopic pregnancy, characterized by the implantation of a fertilized ovum outside the uterine cavity or in an inappropriate place in the uterus such as interstetium, cornual part or cervix, affects approximately 1%-2% of pregnancies in the United States. However, due to the potential for early diagnosis and treatment in outpatient settings, the true prevalence may be higher [ , ]. Patients with EP may experience nonspecific symptoms, including lower abdominal pain and vaginal bleeding. These symptoms can also represent other conditions, such as appendicitis, urinary tract infections, early pregnancy loss, or pelvic trauma [ ].
Cervical ectopic pregnancy (CEP) is a rare form of ectopic pregnancy, occurring in approximately 1 in 8,600 to 12,400 pregnancies [ ]. It is represented by the implantation of the fertilized ovum within the cervical canal, below the internal OS [ ]. Spontaneous heterotopic pregnancy is also a rare condition characterized by the simultaneous occurrence of both intrauterine and extrauterine gestations [ ]. The most common type of heterotopic pregnancy is intrauterine pregnancy combined with tubal pregnancy, while intrauterine pregnancy combined with cervical pregnancy is very rare. CEP is a serious condition associated with significant morbidity and mortality. Delayed diagnosis and treatment can lead to severe complications, including severe bleeding requiring hysterectomy [ ]. Previous cesarean deliveries, dilation and curettage procedures, history of pelvic inflammatory disease, cigarette smoking, fallopian tube surgery, prior ectopic pregnancy, infertility, and assisted reproductive technologies (ART) are risk factors for cervical implantation [ , ]. Despite advancements in ultrasound technology, early diagnosis of heterotopic pregnancy remains challenging due to its often-asymptomatic nature in the initial stages.
We present a case of rare cervical heterotopic ectopic pregnancy, concentrating more on the significance of early diagnosis for optimal maternal and fetal management. We also present a literature review of 25 cases, reported from 1980 to 2024.s
Case presentation
A 32-year-old primigravida female with a history of endometriosis, who got pregnant via in vitro fertilization (IVF), presented for routine check-ups at Shahid Akbarabadi Hospital of Tehran. A transvaginal ultrasound of the uterus and adnexa revealed a gestational sac (GS) in the proximal uterine cavity containing a yolk sac but no fetal pole (FP). Based on a mean sac diameter (MSD) of 13 mm, the gestational age was estimated to be 6 weeks and 1 day. An intramural to submucosal fibroid measuring 29 × 19 mm was also noted, exerting mild pressure on the posterior aspect of the gestational sac in the uterine body.
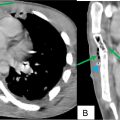
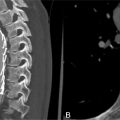
A smaller gestational sac containing a viable embryo with a crown-rump length (CRL) of 3 mm, corresponding to a gestational age of 5 weeks and 6 days, was visualized in the posterior distal cervix, indicative of a cervical ectopic pregnancy (CEP). The distance from the cervical gestational sac to the external OS, considering the decidual reaction, was approximately 5 mm. Myometrial thickness was 9 mm anteriorly and 4 mm posteriorly, excluding the decidual reaction. Based on the findings, a heterotopic pregnancy was diagnosed, comprising an intrauterine pregnancy without a visible embryo and an ectopic gestational sac in the cervix ( Figs. 1–3 ).



Six days after the initial diagnosis, intracervical injections of potassium chloride (KCl) and methotrexate (MTX) were administered for the cervical ectopic pregnancy. A follow-up ultrasound at the same day showed a subchorionic hematoma measuring 16 × 18 mm adjacent to the intrauterine gestational sac. The intrauterine pregnancy was located appropriately, containing a FP with fetal heart rate (FHR) = 138 beats/min (bpm) and CRL corresponding to 6 weeks and 2 days ( Fig. 4 ). The cervical gestational sac measured 15 × 14 mm, and no cardiac activity was detected in the FP anymore suggestive of embryo demise ( Fig. 5 ).


On the next day, the patient experienced pain, and the cervical gestational sac was expelled.
In a color doppler ultrasound performed that day, the intrauterine GS contained a fetal pole with FHR of 126 bpm. Subchorionic hematoma measuring 19 × 26 mm, encompassing approximately 5% of the sac circumference, was observed.
The day after the abortion of cervical GS, the patient experienced pain and went through heavy bleeding, the intrauterine GS was also aborted. Misoprostol was prescribed to facilitate the evacuation of retained products of conception, blood and clots.
In a follow-up color Doppler ultrasound performed the day after the abortion of intrauterine GS, the uterus measured 90×60×46 mm. No distinct gestational sac was visible within the endometrial cavity. Two hyperechoic heterogeneous areas measuring 23×16 mm and 32×19 mm with internal vascularity lower than the adjacent myometrium and, suggestive of retained products of conception (RPOC) grade I, were noted in the cervical canal and the proximal part of the endometrial cavity respectively.
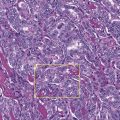
The patient underwent dilation and curettage (D&C), and Samples of uterine contents, preserved in 2 formalin containers, were sent to the pathology laboratory for microscopic and macroscopic evaluation. One container containing expelled uterine contents was macroscopically described as multiple pieces of creamy-brown soft tissue with a total size of 4 × 3 × 1.5 cm. Half of this volume was transferred to a basket, and 50% of the sample was passed. The second container contained curettage material, similarly, described macroscopically as creamy-brown soft tissue, with a total size of 3 × 2 × 1 cm. Half of this sample was transferred to a basket, and 70% of the sample was passed. Microscopic examination confirmed the presence of products of conception (POC) in both samples.
Discussion
In this study, we presented the diagnostic and therapeutic process of a case of heterotopic cervical pregnancy (CP) after IVF. The diagnosis was made using transvaginal ultrasound and achieved in a timely manner. Fortunately, the ectopic pregnancy (EP) was successfully expelled, and maternal health was preserved. However, despite all efforts, we were unable to sustain the intrauterine pregnancy. Additionally, we conducted a literature review focusing on the diagnosis and management of CP to provide further context and insight.
The first documented ultrasound findings of cervical pregnancy were described by Raski in 1978 [ ]. The prevalence of cervical pregnancy (CP) is exceedingly rare, accounting for less than 1% of all EPs [ ]. Studies indicate that a significant proportion of EP patients, ranging from 50% to 90%, have previously undergone uterine curettage [ ]. Additional potential risk factors have been recognized, such as endometrial inflammation, disruptions in the intrauterine environment, the use of intrauterine devices (IUDs), structural uterine anomalies, the presence of uterine fibroids, congenital fetal defects, and the application of assisted reproductive technologies (ART) [ ]. Untreated cervical pregnancy has significant risks, including severe bleeding, the potential need for hysterectomy, or even death. These dangers become more notable when a cervical pregnancy coexists with an intrauterine pregnancy, necessitating careful consideration of preserving the intrauterine pregnancy during the treatment process [ ]. The rise in ectopic pregnancies associated with IVF procedures remains inadequately understood. The transfer of multiple embryos during IVF could contribute to a higher likelihood of various implantations. Additionally, the elevated hormone levels induced during ovarian stimulation might negatively impact endometrial receptivity, potentially influencing implantation outcomes [ ]. Also, factors such as infertility, cervical injury, and embryo reflux resulting from embryo transfer (ET) may contribute to an increased risk [ ]. In most women with heterotopic pregnancy located in the cervical region of the uterus, symptoms typically present as vaginal bleeding [ ]. Diagnosis is often achieved through transvaginal ultrasonography. In some cases, pelvic Magnetic Resonance Imaging (MRI) examination is also utilized for diagnostic purposes [ , ]. Most cases of this type of pregnancy are identified and diagnosed between weeks 5 and 8 (approximately 70%). Diagnosis occurs in 20% of cases between weeks 9 and 10, and in 10% of cases after week 11 [ ]. The choice of treatment method for heterotopic cervical pregnancy depends on various factors, including the gestational age, the mode of conception, the fetal cardiac status, and the mother’s preference regarding the preservation or termination of the pregnancy [ ]. Treatment options can be surgical or conservative. Surgical methods include procedures such as aspiration, curettage, hysteroscopy, or uterine artery embolization. Conservative approaches involve the local or systemic injection of agents like methotrexate (MTX), potassium chloride (KCl), high-concentration sodium chloride (NaCl), or glucose. If the mother requests to preserve the pregnancy, it is essential to carefully consider the potential adverse effects of MTX and uterine artery embolization on the fetus and the pregnancy. This decision-making process requires a multidisciplinary approach to ensure maternal safety and the best possible outcome for the pregnancy [ ].
To analyze the symptoms, different forms of treatment, and relatable outcomes of heterotopic cervical pregnancy we reviewed 25 relevant case reports from 1980 to 2024 ( Table 1 ).
| Year | Authors | Maternal Age | Gravida | Para | Pregnancy way | Medical history | Symptoms | Embryos implanted | Embryo morphology | Time to first detect | Treatment | Pregnancy outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1980 | Giorgio et al. [ ] | 30 | Not mentioned | Not mentioned | Spontaneous | Not mentioned | Painless vaginal bleeding | One in the cervix | – | 9 wk pregnancy | Suction aspiration curettage and suture | Intentional abortion |
| 1994 | Centini et al. [ ] | 36 | 1 | 1 | Spontaneous | Cesarean section | diffuse pains in the lower pelvis | One in the cervix | – | 6 wk+ 2 d | Aspiration, curettage, and methotrexate | Intentional abortion |
| 2001 | Chen at al. [ ] | 35 | 1 | 0 | ICSI | Bilateral salpingectomy, polypectomy | Mild vaginal bleeding | One intrauterine and one in the cervix | Cleavage embryo | 25 d after ET | Aspiration, local injection of KCl, cerclage (10 wk) | Live birth through cesarean section at 38 wk |
| 2003 | Cepni I et al. [ ] | 27 | Not mentioned | 0 | Spontaneous | Unremarkable | vaginal bleeding, lower abdominal pain, and nausea | one in the cervix | – | 7 wk | Aspiration and systematic methotrexate | Intentional abortion |
| 2003 | Porpora et al. [ ] | 29 | 4 | 1 | Spontaneous | Left salpingectomy | Asymptomatic | One intrauterine and one in the cervix | – | 6 wk | Aspiration | Abortion (1 day after aspiration) |
| 2006 | Ujvari et al. [ ] | 27 | 0 | 0 | IVF-ET | bilateral occlusion of uterine tubes | Asymptomatic | Two intrauterine and one in the cervix | Cleavage embryo | 4 wk after ET | Aspiration | Two live births through cesarean section at 29 wk |
| 2007 | Cho et al. [ ] | 35 | Not mentioned | Not mentioned | IVF-ET | Not mentioned | Asymptomatic | One intrauterine and one in the cervix | Not mention | 7 wk | Aspiration | Delivery of a healthy infant at 35 wk |
| 2007 | Prorocic and Vasiljevic [ ] | 31 | Not mentioned | Not mentioned | IVF-ET | Bilateral salpingectomy | Vaginal bleeding | Two in the uterine and one in the external cervical ostium | Not mentioned | 6 wk | Aspiration and local injection of hypertonic solution of sodium chloride | Ongoing pregnancy |
| 2007 | Suzuki et al. [ ] | 35 | 0 | 0 | IVF-ET | Unremarkable | Asymptomatic | Two intrauterine and one in the cervix | Not mention | 24 d after ET | Aspiration and local injection of 33% glucose solution | Two live births through cesarean section at 34 wk |
| 2009 | Shah et al. [ ] | 34 | 4 | 2 | IVF/ICSI | Myomectomy, cesarean section, curettage | Asymptomatic/ painless vaginal bleeding after aspiration | One intrauterine and one in the cervix | Cleavage Embryo | 34 d after ET | Aspiration/ internal iliac artery balloon catheters placement before delivery | Live birth through cesarean section at 37 wk |
| 2009 | Kim et al. [ ] | 30 | 1 | 0 | Spontaneous | Not mentioned | Asymptomatic/ bleeding during aspiration | one intrauterine and one in the cervix | – | 8 wk | Aspiration and Foley catheter insertion | Live birth through cesarean section at 37 wk |
| 2010 | Faschingbauer et al. [ ] | 25 | Primigravida | 0 | clomiphene citrate/ spontaneous | Unremarkable | vaginal bleeding | One intrauterine and one in the cervix | – | 9 wk | Aspiration and cerclage | Live birth through vaginal delivery at 39 wk+3 d |
| 2015 | Tsakos et al. [ ] | 41 | 2 | 0 | IVF-ET | History of ectopic cervical pregnancy | Asymptomatic | One intrauterine and one in the cervix | Blastocyst‐stage embryo | 7 wk+ 5d | Aspiration, Foley catheter insertion, cerclage | Live birth through cesarean section at 38 wk |
| 2019 | Drezett et al. [ ] | 36 | 0 | 0 | IVF-ET | Hyperprolactinemia | Vaginal bleeding | One in the cervix | Cleavage embryo | 36 d after ET | Aspiration under laparoscopy | Intentional abortion |
| 2021 | Mu et al. [ ] | 34 | 5 | 2 | Not mentioned | Surgery for a left eye vascular tumor | Amenorrhea and irregular vaginal bleeding | One intrauterine and one endocervical gestational sac | Not mentioned | 7+ wk | Aspiration, uterine artery embolization | Total abortion |
| 2021 | Koutras et al. [ ] | 30 | 3 | 2 | Spontaneous | Unremarkable | Lower abdomen pain and vaginal bleeding | One intrauterine and one in the cervix | Not mentioned | 7W + 4d | Mifepristone, synthetic steroid, misoprostol, prostaglandin E1, curettage, Foley balloon | Total abortion |
| 2022 | Fan et al. [ ] | 29 | Not mentioned | 0 | IVF-ET | Not mentioned | Vaginal bleeding, abdominal pain, dizziness | One intrauterine and one endocervical gestational sac | Cleavage | 42 d after ET | CP aspiration under ultrasound guidance, tranexamic acid gauze, 800 mL blood transfusion | C-section delivery at 39 wk |
| 2022 | Fan et al. [ ] | 27 | 1 | 1 | ICSI-ET | Right salpingectomy, ART treatment | Mild vaginal bleeding | One intrauterine and one endocervical gestational sac | Cleavage | 36 d after ET | CP aspiration under ultrasound guidance, tranexamic acid gauze | Vaginal delivery at 27 wk |
| 2022 | Tan et al. [ ] | 29 | Not mentioned | Not mentioned | IVF-ET | Not mentioned | Not mentioned | One intrauterine and one endocervical gestational sac | D5 blastocysts | 20 d after ET | Aspiration of cervical gestational sac under vaginal ultrasound guidance | Delivery at 20 wk and 6 d |
| 2022 | Tan et al. [ ] | 30 | Not mentioned | Not mentioned | IVF-ET | Not mentioned | Asymptomatic | One intrauterine and one endocervical gestational sac | D3 blastocysts | 24 d after ET | Aspiration of cervical gestational sac under vaginal ultrasound guidance | Successful delivery |
| 2022 | Sheng et al. [ ] | 31 | 2 | 0 | IVF-ET | Left salpingectomy, lost left fallopian tube | Asymptomatic | One intrauterine and one endocervical gestational sac | Not mentioned | 33 d after ET | Ultrasound-guided hysteroscopic surgery, Foley catheter, iodine gauze | C-section delivery at 38 wk |
| 2023 | Valdés-Martínez et al. [ ] | 35 | Not mentioned | 0 | IVF-ET | History of infertility and C-section | Mild transvaginal bleeding | One intrauterine and one cervical gestational sac | Not mentioned | 6.2 wk | Puncture of cervical gestational sac with ultrasound guidance, aspiration of a milliliter of amniotic fluid, 100 mg of MTX | Live birth through cesarean section at 38.4 wk |
| 2023 | Valdés-Martínez et al. [ ] | 28 | 1 | 1 | Not mentioned | Previous C-section | Moderate transvaginal bleeding | Only one cervical gestational sac | Not mentioned | 7.1 wk | Puncture of cervical gestational sac with ultrasound guidance, aspiration of a milliliter of amniotic fluid, 100 mg of MTX | Intentional abortion |
| 2023 | Valdés-Martínez et al. [ ] | 40 | Not mentioned | 0 | IVF-ET | 2-yearof infertility | Asymptomatic | Only one cervical gestational sac | Not mentioned | 2 wk | Puncture of cervical gestational sac with ultrasound guidance, aspiration of a milliliter of amniotic fluid, 100 mg of MTX | Intentional abortion |
| 2024 | Alexakis et al. [ ] | 33 | 2 | 0 | IVF-ET | Not mentioned | Excessive nausea and vomiting | One intrauterine and one endocervical gestational sac | Blastocyst | 6 wk | Ultrasound-guided KCL injection in to cervical sac | Delivery at 36 wk and 6 d |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree