Hypopharynx
Key Points
The hypopharynx comprises pyriform sinuses and posterior pharyngeal wall. The pyriform sinus is conical in shape. Its medial wall is the lateral component of the supraglottic larynx, and the lateral wall is the lateral aspect of the pharynx. The majority of the posterior wall resides posterior to the larynx. Neoplasms in this location are referred to as postcricoid tumors.
As the larynx essentially “resides in” the hypopharynx, strategies for management are similar for carcinomas originating from these two sites. The major objectives are tumor eradication, preservation of the natural speech, swallowing function, and avoidance of permanent tracheostomy.
Hypopharyngeal carcinoma is usually diagnosed at more advanced T category with a higher incidence of nodal involvement than cancer of the larynx.
Early tumors can be effectively controlled with radiotherapy but, similar to laryngeal carcinoma, the current standard treatment for intermediate-stage disease (bulky T2 or T3) is radiation plus concurrent cisplatin.
More advanced, resectable tumor is often managed with pharyngolaryngectomy followed by adjuvant radiation alone or radiation plus concurrent cisplatin.
Induction chemotherapy (docetaxel, cisplatin, and fluorouracil) followed by radiation can be useful in driving the decision to attempt for larynx preservation in responders.
The overall prognosis of patients with hypopharyngeal carcinoma is worse than that of patients with laryngeal cancer.
PYRIFORM SINUS
Treatment Strategy
Primary radiotherapy is preferred for stage I and II tumors. Extrapolating from trials on laryngeal cancer (some European studies also enrolled hypopharyngeal carcinomas), radiation with three cycles of concurrent cisplatin (100 mg/m2, q 3 week) is the preferred organ-preserving treatment for bulky T2 and T3 tumors. Neck dissection is indicated in node-positive patients who have residual neck mass 6 to 10 weeks after completion of radiotherapy.
The standard treatment for resectable T4 tumors is total pharyngolaryngectomy usually with postoperative radiotherapy and, when indicated based on the presence of extracapsular extension (ECE) or positive margins, combined with concurrent cisplatin. Selected patients may be enrolled into ongoing trials; for example, testing combination of anti epidermal growth factor receptor antibody, cetuximab, with concurrent radiation-chemotherapy or induction chemotherapy followed by concurrent radiation-chemotherapy.
Indications for postoperative radiotherapy and irradiation of the tracheal stoma are similar to those for carcinoma of the larynx.
Primary Radiotherapy
Target Volume
The initial target volume encompasses the primary tumor with good margins and bilateral neck nodes, including the retropharyngeal, and level II to V nodes. The target volume also includes ipsilateral level IB in the presence of level II node (Case Studies 10-1 and 10-2).
The boost volume encompasses the primary tumor and involved nodes with 1- to 2-cm margins.
Case Study 10-1
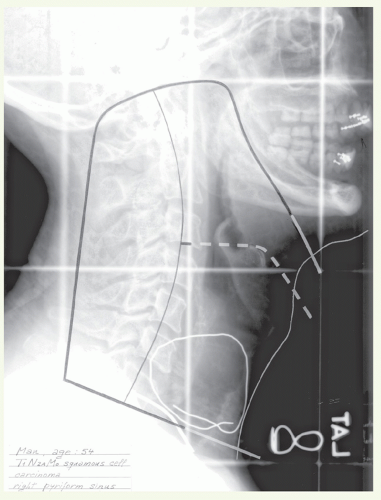
A 54-year-old man had a routine checkup and was found to have a right neck mass. He was referred for workup and treatment. Physical examination showed discrete redness and mucosal irregularity in the medial and lateral walls of the right pyriform sinus without changes at the apex. There was a 5-cm firm node, fixed to the sternocleidomastoid muscle, palpated in the right lower jugular area.
A biopsy from the right pyriform sinus showed moderately to well-differentiated squamous cell carcinoma. Stage: T1 N2a M0. The primary tumor, bilateral level II to IV, and retropharyngeal nodes were treated with lateral parallelopposed photon fields (Fig. 10.1). The inferior border was placed just above the shoulders to encompass the involved lower jugular node (wired). Since all disease was located on the right side, the fields were weighted 3:2 in favor of the right side. A total dose of 66.6 Gy was delivered to the isocenter, which resulted in a dose of 68 Gy to the primary and 72 Gy to the involved node in 7 weeks. Off-spinal cord reduction was made at 45 Gy. The posterior cervical nodes were supplemented with electrons to 54 Gy. The supraclavicular nodes were treated with an anterior appositional photon field to 54 Gy. Tissues directly posterior and inferior to the palpable node received additional irradiation to a cumulative dose of 63 Gy. Physical examination 6 weeks after completion of radiotherapy revealed a complete response at the primary site. In the neck, however, a 3-cm residual node was noted. Therefore, patient subsequently underwent a right neck dissection. He was alive and functioning well 2.5 years after therapy.
Case Study 10-2
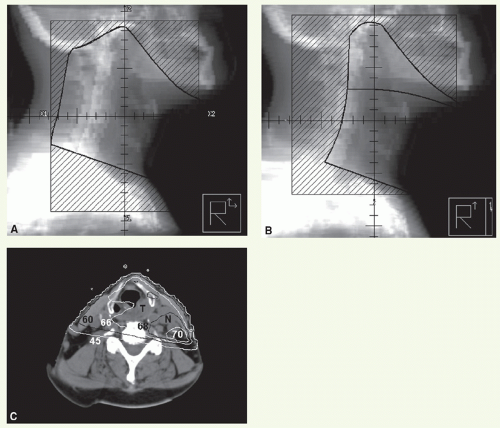
A 76-year-old man presented with a 10-month history of left-sided sore throat and otalgia. A 1.5-cm tumor was detected on the medial wall of the left pyriform sinus without extension to the apex. The larynx mobility was normal. A 1-cm lymph node was detected in level III in the left neck.
Biopsy of the primary tumor revealed moderately differentiated squamous cell carcinoma. Stage: T1 N1 M0. He was treated with 6 MV photons, with the primary tumor and upper and mid neck lymphatics as well as the retropharyngeal nodes encompassed in parallel-opposed fields (Fig. 10.2A). These portals received 42 Gy. An anterior supraclavicular and low neck field was matched on the skin and treated to 50 Gy. The upper fields were reduced off the spinal cord and continued to 54 Gy. An additional 12 Gy was delivered to coned-down portals to a final dose of 66 Gy. The off-spinal cord and boost fields were treated with parallel right anterior and left posterior oblique fields (Fig. 10.2B) to encompass the gross disease in the photon fields. The boost was preferentially weighted to the left. An isodose distribution through the central axis and primary tumor (T) and gross lymph node (N) is shown in Figure 10.2C. Both posterior cervical strips received 12 Gy supplement in six fractions with 9 MeV electrons, and then the left posterior strip received an additional boost of 12 Gy. The patient is without evidence of disease 2 years later.
Setup and Field Arrangement for Conventional Radiotherapy Technique
Marking of shoulders and palpable nodes facilitates portal design. The patient is immobilized in a supine position with the shoulders pulled down to the maximal extent. Lateral parallel-opposed photon fields are used to treat the primary tumor and upper and mid neck nodes.
Superior border: at the level of the skull base to include the upper jugular and parapharyngeal lymphatics.
Anterior border: 1-cm falloff.
Posterior border: behind the spinous processes or more posteriorly in the presence of large nodal mass.
Inferior border: encompasses primary lesion with margin (as low as possible while avoiding the shoulders).
A matching anterior portal is used to treat the lower neck nodes. It may be necessary to use anterior and inferior tilts for patients with a short neck or because of the inferior extent of the primary tumor or nodal mass. In this case, the supraclavicular fossae are included in the primary portal (see Fig. 9.11). For boost volume, reduced lateral fields are used as follows:
Superior and inferior borders: depends on the extent of the disease; at least include aryepiglottic folds superiorly and cricoid cartilage inferiorly.
Anterior border: 1-cm falloff, except when primary lesion is confined to the posterior structures where a small strip of anterior skin may be spared.
Posterior border: midvertebral bodies, or posterior one third of vertebral bodies when the primary involves posterior pharyngeal wall.
Involved upper and midjugular nodes receive boost dose through lateral fields along with the primary tumor and lower neck nodes through a reduced anterior portal.
Intensity-Modulated Radiation Therapy Planning
Most patients are now treated with intensity-modulated radiation therapy (IMRT) to spare parotid function (Case Study 10-3). The primary tumor and involved node(s) with a minimum of 1-cm margin constitutes CTVHD (CTV1). However, because of laryngeal motion, it is prudent to encompass the majority of the larynx in the high-dose target volume. CTVID (CTV2) defines the neck compartments outside CTVHD with a 2-cm (cranial-caudal) margin. The remaining nodal levels (II to V) are contoured as CTVED (CTV3). Level Ib on the side of involved node is included in CTVED.
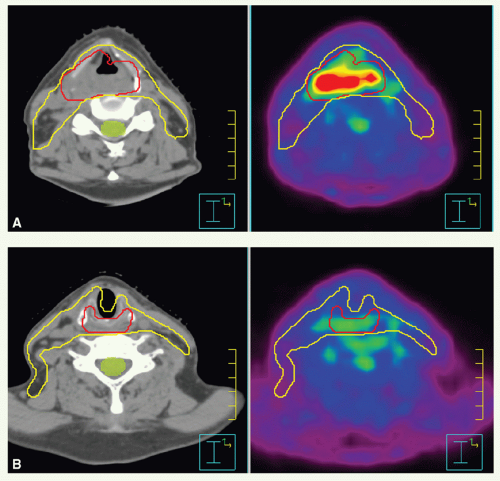
Case Study 10-3
A 61-year-old male, presented with sore throat, mild odynophagia, and weight loss. Examination revealed an extensive tumor of the oropharyngeal walls extending into the right pyriform sinus and postcricoid region, biopsy of which showed squamous cell carcinoma. There was no clinical evidence of lymphadenopathy. He received concurrent radiation and chemotherapy. While bulky disease was seen filling the right pyriform sinus, the disease had significant superficial spread.
A PET-CT simulation was performed to assist in defining the targets, particularly the inferior extent of disease that could not be visualized clinically (Fig. 10.3). An axial CT slice with adjacent fused PET image is shown in Figure 10.3A. The high dose CTV (red) and subclinical target (yellow) are shown on the CT scan. A more inferior slice through the postcricoid region (Fig. 10.3B) did not demonstrate an increase in FDG uptake. A high-dose clinical volume was outlined for boost volume definition, as this slice was approximately 1 cm below the identified gross target volume.
Dose
Stage I (T1 N0) tumors: 50 Gy in 25 fractions to the initial target volume and then 16 Gy in 8 fractions to the primary tumor. For patients treated with IMRT, a dose of 66 Gy is prescribed to CTVHD and 54 Gy to CTVED. An alternative option is to treat with two sequential plans. The first delivers 50 Gy in 25 fractions to CTVHD and CTVED followed by a plan that delivers 16 Gy in 8 fractions to CTVHD.
Stage II (T2 N0) tumors: hyperfractionated or concomitant boost regimen. Hyperfractionation delivers 55.2 Gy in
46 fractions to the initial target volume and then 21.6 Gy in 18 fractions (1.2-Gy fractions, twice daily, 6-hour interval); the spinal cord dose is limited to 44.4 to 45.6 Gy or less, and uninvolved posterior cervical nodes are supplemented with 2 Gy daily to approximately 55 Gy. Concomitant boost delivers 1.8-Gy fractions to 54 Gy in 30 fractions to the initial target volume and 1.5-Gy fractions to 15 to 18 Gy given as second daily fractions during the last 2 to 2.5 weeks; the spinal cord dose is limited to 45 Gy or less. For patients treated with IMRT, one option is to use the concomitant boost schedule, which requires two separate plans. The first plan delivers 54 Gy in 30 fractions to CTVHD and CTVED, and the second plan is for 18 Gy in 10 to 12 fractions to CTVHD (given as second daily fractions). An alternative choice is to use one plan that delivers 70 Gy to CTVHD and 56 Gy to CTVED. Treatment is given in 35 fractions over 30 treatment days, by delivering 6 fractions a week for 5 weeks with a 6-hour interfraction interval on the day 2 fractions are delivered.
46 fractions to the initial target volume and then 21.6 Gy in 18 fractions (1.2-Gy fractions, twice daily, 6-hour interval); the spinal cord dose is limited to 44.4 to 45.6 Gy or less, and uninvolved posterior cervical nodes are supplemented with 2 Gy daily to approximately 55 Gy. Concomitant boost delivers 1.8-Gy fractions to 54 Gy in 30 fractions to the initial target volume and 1.5-Gy fractions to 15 to 18 Gy given as second daily fractions during the last 2 to 2.5 weeks; the spinal cord dose is limited to 45 Gy or less. For patients treated with IMRT, one option is to use the concomitant boost schedule, which requires two separate plans. The first plan delivers 54 Gy in 30 fractions to CTVHD and CTVED, and the second plan is for 18 Gy in 10 to 12 fractions to CTVHD (given as second daily fractions). An alternative choice is to use one plan that delivers 70 Gy to CTVHD and 56 Gy to CTVED. Treatment is given in 35 fractions over 30 treatment days, by delivering 6 fractions a week for 5 weeks with a 6-hour interfraction interval on the day 2 fractions are delivered.
Stage III and IV tumors: in combination with three cycles of concurrent cisplatin, radiation is given in conventional 2-Gy fractions to a dose of 50 Gy to the initial target volume and 70 Gy to the boost volume. Differential loading may be preferred for lateralized lesions with ipsilateral nodal disease only. In this situation, the dose is specified at an isodose line with maximal allowable dose heterogeneity of ±2.5%. The spinal cord dose is limited to 45 Gy or less. For patients treated with IMRT, the commonly prescribed doses are 70 Gy to CTVHD 60 to 63 Gy to CTVID, and 56 to 57 Gy to CTVED, given once daily in 33 to 35 fractions (Case Studies 10-4 and 10-5).
Case Study 10-4
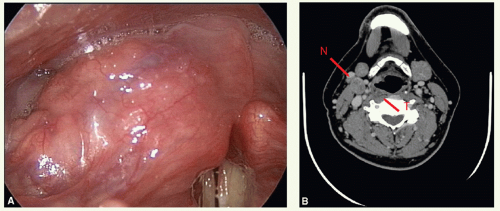
A 53-year-old male presented with a right upper neck mass and mild sore throat.
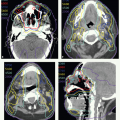
Examination revealed a 2.5 cm upper jugular node and a lesion on the medial wall of the pyriform sinus (Fig. 10.4A). Axial CT images (Fig. 10.4B,C) showed the right level II node and the superior aspect of the primary tumor at the vestibule of the right pyriform sinus and the bulk of the primary lesion at the level of the mid-pyriform sinus. The inferior aspect of the node can be seen abutting the anterior aspect of the sternocleidomastoid muscle. Biopsy of the primary tumor revealed squamous cell carcinoma. He was staged as having a T2 N1 M0 and treated with IMRT with three cycles of concurrent high-dose cisplatin.
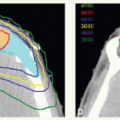
CTVHD (70 Gy) encompassed the primary tumor and involved node with margins, CTVID (60 Gy) the right posterior neck, and CTVED (56 Gy) the left neck (Fig. 10.4D). The ipsilateral hypopharyngeal wall down to the cricoid level was included in CTVHD, right level III nodal region in CTVID, and left level III, and bilateral level IV, nodes in CTVED (Fig. 10.4E,F). Figure 10.4G shows the sagittal isodose distribution through the primary tumor. The patient had good function without evidence of disease 3 years after completing treatment.
Postoperative Radiotherapy
The indications, technique, and dose prescriptions are similar to those for supraglottic carcinoma except that the target volume also encompasses the retropharyngeal nodes. The superior border of the lateral fields is placed at the level of the base of skull (Case Study 10-6). For IMRT treatment planning, CTVHD (CTV1) encompasses the preoperative tumor bed and involved nodal regions with margin, CTVID (CTV2) the operative bed, and CTVED (CTV3) the undissected nodal volumes at risk including the retropharyngeal nodes. The stoma can be delineated as CTVID or CTVED




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree