Interventional radiology continues to be at the forefront of acute and chronic pain management. Our unique imaging expertise and ability to target difficult to reach structures allows for the continuous development of new ways to treat a variety of pain generators. In addition, the advent of thermal ablation techniques and technologies has provided a unique opportunity to offer patients more durable and predictable options to treat their pain. This is particularly important during the opioid epidemic, as multiple local and international governmental bodies push for physicians to create ways to manage pain while reducing the need for long-term opioid dependence. This article aims to review various image-guided techniques and tools for the treatment of pain related to peripheral pain generators, with a focus on the extremities, lumbosacral and pelvic region, and the chest wall. For each target and pathology, we will discuss general etiology, anatomy, procedural approach, and briefly evaluate the supporting literature in each clinical situation.
Introduction
Interventional radiology has had an increasing role in the treatment of various pain syndromes over the last few years. Nonetheless, the treatment of both chronic and acute pain remains challenging given its relation to and exacerbation by patients’ various medical comorbidities, mental health issues, and socioeconomic factors. The continuous development of minimally invasive procedures for the treatment of pain syndromes, although exciting, poses a constant challenge to stay current with the various techniques, tools, and their associated nuances. , This article aims to review commonly used techniques and tools for treating pain related to peripheral pain generators with a focus on the extremities, lumbosacral and pelvic region, and the chest wall. For each, we will discuss general etiology and associated nerve anatomy, a case-based procedural approach, common imaging modalities and tools used in each scenario, as well as possible but infrequent complications. Finally, we will evaluate some of the available literature to help support the various treatment options for each clinical situation with a focus on nerve blocks and ablations.
Upper and lower extremity interventions
Shoulders
Shoulder pain is the third most common musculoskeletal complaint seen in primary care, with approximately 50% of patients continuing to have pain 6 months after their initial visit. The etiology is multifactorial but usually related to degenerative changes, rotator cuff injuries, adhesive capsulitis, bursitis, among others, with significant personal and economic burden. , Initial treatment depends on etiology and consists of pain control and improvement in range of motion through physical therapy. Surgery is considered in severe cases or cases related to rotator cuff injury, particularly in younger patients.
The major nerve supply to the shoulder includes the suprascapular and axillary nerves posteriorly, and the lateral pectoral nerve anteriorly. , The suprascapular nerve supplies the posterior glenohumeral joint capsule and humeral head, which comprises most of the glenohumeral joint sensory innervation. On the other hand, the axillary and lateral pectoral nerves provide sensation to the more lateral and anterior parts of the joint capsule, respectively.
Fluoroscopy is the mainstay modality for targeting the sensory supply to the glenohumeral joint capsule, particularly the suprascapular nerve. , Patients are typically prone with the affected upper extremity flexed and internally rotated while the hand is tucked away underneath their head. A second position, with the arm down by their side, has also been described and can be used for patients that cannot keep their arm flexed during the procedure. The C-arm is then angled so that the suprascapular notch is visualized. The needle can then be introduced by aiming at the inferior suprascapular notch while remaining parallel to the X-ray beam and creating the bull’s eye appearance of the hub overlying the tip. Ultrasound guidance is commonly used peri-operatively by anesthesiologists and in the emergency department by emergency medicine physicians as it provides an effective way to identify the suprascapular notch while reducing ionizing radiation. , However, cadaveric studies suggest that the suprascapular notch can be confused with the suprascapular fossa which may lead to a less reliable block.
Fluoroscopic or CT-guided radiofrequency ablation (RFA) has also been described as an option for patients with recurrent shoulder pain who have previously responded to an anesthetic block. , In this case, all 3 of the aforementioned nerves supplying the glenohumeral joint capsule can be targeted at the same time. Both the suprascapular and axillary nerves are targeted in the prone position as previously described, followed by the lateral pectoral nerve in the supine position. Landmarks include the anterior coracoid process and inferolateral border of the greater tuberosity for the lateral pectoral and axillary nerves, respectively. ,
Knees
Knee osteoarthritis (OA) affects approximately 23% of patients over the age of 40 and significantly contributes to quality-of-life reduction, as well as disability and loss of independence. Various grading scales have been used to gauge the severity of knee OA including the clinical Western Ontario and McMaster Osteoarthritis (WOMAC) index and the radiologic Kellgren and Lawrence (KL) score. The main targets for genicular nerve interventions include the superior medial and lateral genicular nerves at the metaphyseal shaft junction of the femur and the inferior medial genicular nerve at the tibia. , Although fluoroscopy is more commonly used by interventional radiologists, both fluoroscopy and ultrasound provide a safe way to identify the aforementioned nerves and respective landmarks, with neither being significantly more effective than the other when it comes to pain control. ,
The inferior lateral genicular nerve is generally avoided given its proximity to the common peroneal nerve; however, CT-guidance can be used to safely target the nerve on the Gerdy tubercle if the patient’s pain is in the inferolateral knee. Under fluoroscopic guidance, the same landmarks are used for both anesthetic blocks and ablations. The radiographic antero-posterior (AP) view is used to place the probes at the medial and lateral metaphyseal shaft junctions of the femur and the medial tibia. The lateral radiograph is used to confirm positioning of the ablation probes past the mid shaft depth ,
Two options are currently available for genicular nerve ablation including cooled nerve radiofrequency ablation (RFA) and cryoneurolysis. Both techniques have shown promise for the treatment of knee OA, with a larger body of literature on safety and efficacy available for RFA and multiple ongoing randomized controlled trials comparing the 2. A unique indication for cryoneurolysis is for patients who may not tolerate heat-based ablation techniques despite optimized sedation or preprocedural nerve blocks.
Superficial peroneal nerve
Targeting of the superficial peroneal nerve has been described in the literature for the management of pain related to nerve injury, injury to surrounding structures, or as a preoperative block for lower extremity surgery. Less commonly, superficial peroneal nerve blocks have been used for cancer related pain refractory to oral and intravenous pain regimens. The superficial peroneal nerve is a branch of the sciatic nerve that supplies sensation and motor innervation to the lateral lower leg and dorsum of the foot. , It can often be injured in the setting of trauma or surgery, usually at the level of the lateral popliteal fossa or ankle. , It is also this very superficial location that makes it a good target for intervention.
Ultrasound has been previously used for superficial peroneal nerve anesthetic blocks in office and emergency room settings. Canella et al. demonstrated that on ultrasound, the superficial peroneal nerve was found between the peroneus longus muscle and the anterior crural intermuscular septum in most patients. The nerve could be targeted on ultrasound as it came close to piercing the crural fascia. CT and fluoroscopic guidance can also be used for both anesthetic blocks and ablations. During CT-guidance, the needle or ablation probe is placed in the posterolateral popliteal fossa where the nerve is known to course through. For fluoroscopic guidance, the anterolateral aspect of the fibular head is targeted instead, with the needle or probe positioned a couple of millimeters away from it.
In terms of ablation modalities to choose from, RFA has been described in a few instances and only in the setting of knee pain for patients who have failed the traditional genicular nerve targets or pain related to entrapment syndrome. , Cryoneurolysis has been more frequently described and shown to be effective in a few case series for post-traumatic pain, neuropathic pain related to diabetes and multiple sclerosis, as well as symptomatic ankle OA. ,
Chest wall interventions
Intercostal nerve
Intercostal nerve blocks have been shown to significantly reduce chest wall pain and decrease the need for opioid medications in the setting of trauma, cancer, post thoracotomy, and even post herpetic neuralgia. , The intercostal nerves carry motor innervation to the intercostal muscles and transmit nociceptive signals from the skin and parietal pleura back to the spine. These nerves arise from the anterior rami of T1 to T11 and travel within the neurovascular bundle along each subcostal space.
Fluoroscopic and CT-guidance is often reserved for more complex cases such as in the setting of ablation or targeting of metastatic lesions. , Most patients are placed in the prone or decubitus position, with the needle or probe advanced directly into the subcostal space. Alternatively, the needle or probe can be advanced until there is contact with the periosteum and then “walked” caudally towards the subcostal space. , Some operators may prefer cryoneurolysis over RFA for intercostal nerve ablations given the proximity to critical structures and direct visualization of the ice ball under CT-guidance.
Anterior and lateral cutaneous nerves of the chest
The anterior and lateral cutaneous chest wall nerve (fascial plane) blocks are a more recently developed approach for the management of chest wall pain and have been shown to be effective particularly in the setting of cardiothoracic surgery. These nerves usually arise as branches of the T2-T6 intercostal nerves and provide sensory innervation to most of the axilla, anterolateral, and anteromedial chest wall. Although anesthetic blocks are the mainstay for image-guided treatment, RFA has been described for the treatment of anterior cutaneous nerve entrapment syndrome (ACNES) in the setting of upper abdominal wall pain. However, the cutaneous nerves responsible for ACNES usually arise from the lower T7-L1 levels.
Ultrasound is the main modality for fascial plane blocks of the chest, although CT-guidance can also be used. With the probe in the transverse or para-sagittal plane, general landmarks for the anterior cutaneous nerve include the fascial planes between the pectoralis major and the internal intercostal muscle or between the internal intercostal and the transversus thoracic muscle, just lateral the sternum. There are various techniques to access the lateral cutaneous nerve depending on the location of the pain (anterolateral or posterior chest wall), with one of the main ones being the placement of the probe in an oblique position while injecting the plane between the intercostal muscles and overlying erector spinae muscles.
Pelvic interventions
Lateral femoral cutaneous nerve
The lateral femoral cutaneous nerve arises from the L2 to L3 ventral rami and courses inferiorly towards the notch of the anterior superior iliac spine to supply sensory innervation to the anterolateral thigh. The most commonly associated pathology is meralgia paresthetica which leads to neuropathic pain in this region, usually related to obesity, diabetes, or tight clothing. However, it has also been targeted with good success in the setting of total hip arthroplasty and even in patients with neuropathic pain from skin grafting for burns. Anesthetic blocks and thermal ablation can also be used in these patients. RFA and cryoneurolysis have both shown prolonged pain control ranging from a few weeks up to as long as 12 months. ,
Ultrasound and CT-guidance are used as the main modalities to identify the lateral femoral cutaneous nerve. Under ultrasound, the probe is oriented in the transverse plane and ran from lateral to medial along the inguinal ligament, with the nerve found between the fascia lata and fascia iliaca. , On CT, the nerve is targeted on the axial plane by aiming just anterior to the iliac bone.
Obturator nerve
The obturator nerve arises from the ventral rami of L2-L4 and reliably courses medial to the acetabulum. It passes through the obturator canal to provide motor and sensory innervation to multiple anteromedial muscles of the thigh and sensation to the anteromedial hip joint capsule. , Hence, a history of isolated proximal anteromedial thigh pain should make you think of the obturator nerve as a possible pain generator.
Obturator nerve blocks have been widely used for pain control prior to hip and knee surgery, adductor spasticity, and even in the setting of transurethral bladder tumor resection. RFA and cryoneurolysis have also been effective not only in patients with chronic hip pain from OA, but also in the setting of metastatic disease to the osseous hip and soft tissues of the lateral pelvic wall. , Hydrodissection can be used in the cases of lateral pelvic wall lesions to protect surrounding structures, with cryoneurolysis being preferred by some operators given direct control and visualization of the ice ball.
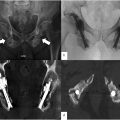
In most cases, patients are supine with their hips slightly abducted. Under ultrasound, the probe is placed in the medial inguinal crease while targeting the junction between the pectineus muscle and the adductor brevis where the obturator nerve generally resides. On fluoroscopy, the AP view is used to target the “teardrop” shaped acetabular incisura between the junction of the ischium and the inferior pubic ramus. On CT, the medial acetabulum is targeted, with the caveat that CT can be used to target deeper structures or lesions if needed.
Pudendal nerve
The pudendal nerve, much like the intercostal nerves, has been a consistent subject of research in the image-guided pain interventions arena, from which many other pain interventions and targets have been derived. This nerve arises from the anterior rami of S2-S4 and provides sensory innervation to the perineum, pelvic musculature, rectum, and genitalia. Pudendal neuralgia is the main indication for pudendal nerve interventions. This is a chronic condition usually related to injury to the nerve in the setting of prolonged sitting, horseback riding or biking, surgery, and postpartum. Less commonly, it can be related to pelvic neoplasms from primary or metastatic disease. Interestingly, prior small prospective studies have also shown good safety, efficacy, and technical feasibility for the treatment of premature ejaculation.
The nerve can be treated by anesthetic blocks and thermal ablation. , Neurectomy and neurostimulation are also in the treatment algorithm but are generally not offered given their associated morbidity. RFA and cryoneurolysis have been used, however, cryoneurolysis is thought of as the workhorse in the treatment of pudendal neuralgia. Cryoneurolysis is particularly helpful in the pelvis given the proximity of the pudendal nerve to adjacent visceral structures.
CT is the main modality for targeting the easily identifiable Alcock’s canal, formed by the medial fascia of the obturator internus at the lateral aspect of the ischiorectal fossa, where the nerve reliably resides in the pelvis. Fluoroscopy and ultrasound have also been used to target the pudendal nerve but unfortunately do not offer the ability to visualize the expansion of the Alcock’s canal from anesthetic injectate. Hence, patients who fail to respond to treatment after fluoroscopic or ultrasound guidance cannot be ruled out from having pudendal neuralgia, as the injection or ablation zone may not have accurately targeted Alcock’s canal.
Sacral plexus and sacroiliac joint
The sacral plexus is a complex group of nerves composed of branches from S1 to S5 with minor contributions from L5 descending nerve root branches. The sacral plexus gives rise to a large portion of the individual nerves we have discussed in the previous sections. However, the plexus can be targeted more proximally before it branches, as the individual sacral nerve roots pass through their respective neural foramina. , Although the majority of sacral pain is related to benign etiologies such as trauma or degenerative changes, osseous and pelvic metastatic disease affecting these nerve roots is another indication for sacral plexus interventions. In addition, sensory branches from the lower lumbar and sacral plexus innervate the sacroiliac (SI) joints which are another common site of degenerative changes and pain generation related to hip and lower back pain. ,
Fluoroscopy and CT are the preferred modalities for interventions involving the sacral plexus and sacroiliac joints. Under fluoroscopy, patients may be in the prone or decubitus position with the AP or oblique views used to target the sacral neural foramina or SI joints. Similarly, when using CT-guidance, patients will be in the prone position and the same targets are identified in the axial plane. Even though the majority of sacral plexus and SI joint interventions are in the form of anesthetic blocks, recent meta-analyses have shown similar efficacy but longer duration of pain control for RFA, sometimes as long as 9 months or more. Although literature is scarce for cryoneurolysis in this patient population, the use of cryoneurolysis along with alcohol ablation has been reported for the treatment of pain related to sacral metastases with complete resolution at follow-up.
Pericapsular nerve group (PENG)
The pericapsular nerve group (PENG) block is a novel technique that was initially described by Girón-Arango et al in 2018. , Based on prior cadaveric studies, his group suggested that the hip capsule sensory innervation could be blocked under ultrasound by targeting articular branches of the obturator, femoral, and accessory obturator nerves, all at once. , Since then, its use has been described in a few small, randomized control trials mainly focused on perioperative analgesia in patients undergoing total hip arthroplasty. , In a recent meta-analysis, Andrade et al. showed that PENG blocks were associated with an overall decrease in pain scores at rest and a decrease in opioid consumption in the immediate postoperative period. A single case report in the literature describes RFA for chronic hip pain, achieving good pain control for up to 6 weeks after the procedure.
In terms of imaging modalities, ultrasound has been the only reliably cited tool for performing PENG interventions. In these cases, patients are supine, and the probe is positioned in the transverse plane at the level of the anterior superior iliac spine with the needle targeted at the fascial plane between the psoas tendon anteriorly and the pubic ramus posteriorly. As far as we are aware, there are no reports in the literature on the use of CT-guidance for PENG blocks or ablations Figures 1-16 .






Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree