Image-guided robotic interventions have revolutionized the treatment of musculoskeletal (MSK) diseases, combining the precision of robotics with advanced imaging to improve procedural accuracy and patient outcomes. This review delves into the evolution, current applications, and future prospects of robotic systems in managing MSK disorders. Special attention is given to the integration of various imaging modalities, the clinical impact on patient care, and the ongoing challenges that need to be addressed to enhance the adoption and efficacy of these technologies.
Introduction
Musculoskeletal diseases, encompassing a broad range of conditions both benign and malignant affecting bones, joints, muscles, and connective tissues, are prevalent and a leading cause of pain and disability worldwide. Traditional treatment strategies often include surgical interventions or minimally invasive procedures guided by imaging techniques such as fluoroscopy, computed tomography (CT), and magnetic resonance imaging (MRI). While effective, these methods have limitations related to operator dependency, equipment availability, and variability of techniques among different practice settings. The integration of robotic technology into image-guided interventions has addressed many of these challenges by improving precision, safety, and reproducibility.
Historical development of robotic-assisted musculoskeletal interventions
The history of robotic technology in surgery and interventional radiology dates back to the late 20th century, with some of the first robotic systems being used for neurosurgical and urological procedures. The application of robotics in orthopedic and musculoskeletal disease management evolved as imaging modalities improved and computer-assisted navigation became more sophisticated. Early systems, such as the ROBODOC (THINK SURGICAL) for hip arthroplasty and the first FDA approved robot da Vinci Robotic Surgical System (Intuitive Surgical, USA) for general surgery, paved the way for specialized MSK robotic technologies.
Overview of robotic systems and imaging modalities in interventional radiology
Robotic systems used in musculoskeletal interventions have evolved significantly, driven by advances in engineering, computer science, and medical imaging. These systems are designed to improve the precision, safety, and efficacy of various procedures, offering interventional radiologists enhanced tools for addressing complex medical challenges. The main types of robotic systems utilized in MSK interventions can be categorized into 3 primary types: passive, semi-active, and fully active systems. Each type serves a unique role in supporting and improving the procedural workflow, with varying degrees of automation and operator interaction.
Passive Robotic Systems
Passive robotic systems act as stabilizing platforms or guides, enabling interventional radiologists to perform precise procedures without the system actively moving or performing tasks autonomously. These systems are often used as adjuncts to improve the accuracy of manual techniques by holding instruments steady, ensuring that movements are precise and controlled. For example, the Epione robotic system (Quantum Surgical, France) assists in the accurate needle placement with stabilization and trajectory planning. This support minimizes the potential for deviation, even during prolonged or complex procedures.
Passive robotic systems can be particularly beneficial when combined with preoperative imaging data, such as CT scans, which provide a detailed anatomical map. The IR can align the robotic arm based on these images, and the system will hold the instrument in place, allowing for the accurate execution of procedures with minimal human error. While these systems do not perform automated actions, they provide significant assistance in ensuring that the intervention follows the planned path and reduces tremors or unintentional movements from the operator.
Semi-Active Robotic Systems
Semi-active robotic systems offer a blend of manual control and robotic precision, making them ideal for procedures that require both human expertise and robotic assistance. These systems work in tandem with the provider, performing specific controlled movements while allowing the operator to retain overall control. This hybrid approach enhances the operator’s capabilities without completely removing their input, providing an additional layer of safety and precision.
One of the most prominent applications of semi-active robotic systems is in joint replacement surgeries, such as total knee arthroplasty (TKA). In these procedures, semi-active robotic systems assist by guiding bone cutting and the placement of implants according to preoperative planning data. The system ensures that the bone is prepared at the precise angles and depths needed for optimal prosthetic fit, leading to improved mechanical alignment and patient outcomes. Semi-active systems can also provide haptic feedback, alerting the operator if the instrument strays beyond predefined safe boundaries, thus enhancing both accuracy and safety.
In interventional radiology, semi-active robotic systems may be employed in procedures such as tumor ablation and percutaneous biopsies. The system can guide the needle or ablation probe along a pre-programmed trajectory, allowing the operator to make real-time adjustments if necessary, such as the ACE robotic system (XACT Robotics, Israel). This combination of robotic precision and operator flexibility enables more consistent results, particularly in challenging anatomical regions or cases involving critical structures.
Fully Active Robotic Systems
Fully active robotic systems represent the most advanced category of robotic assistance, capable of performing procedural tasks autonomously based on preoperative planning and intraoperative imaging data. These systems are designed to carry out specific movements without the need for continuous human guidance, although operator oversight is essential to monitor the process and intervene if needed, such as the optically tracked iSYS-1 robot (iSYS Medizintechnik GmbH, Austria). Fully active systems are equipped with sophisticated software that integrates imaging data, such as CT or MRI, to map out a precise plan for the intervention and execute it with minimal deviation.
In MSK interventions, fully active robotic systems are used for tasks like percutaneous screw placement, complex joint reconstructions, and even tumor ablations where high levels of accuracy are required. The robotic system can autonomously position the needle or surgical instrument according to the preoperative plan, ensuring that it reaches the targeted site with unparalleled precision. This capability significantly reduces the risk of complications related to human error and variability, making fully active robotic systems especially valuable in procedures involving small or deeply situated anatomical targets.
Imaging modalities supporting robotic-assisted interventions
Robotic systems rely heavily on advanced imaging modalities to function effectively. These imaging techniques provide the detailed visualization necessary for planning and guiding procedures, ensuring that the robotic system can accurately interpret the anatomical landscape and execute tasks with precision.
- •
Computed Tomography (CT) : CT imaging is a cornerstone of robotic-assisted interventions, providing high-resolution cross-sectional images that help in creating detailed 3D models of the patient’s anatomy. These models are essential for planning complex procedures such as spinal screw placement or tumor ablation, allowing the robotic system to map out and execute precise movements.
- •
Magnetic Resonance Imaging (MRI) : MRI offers superior soft tissue contrast and is used for procedures that require detailed visualization of muscles, tendons, and other soft tissue structures. Robotic systems equipped with MRI-guided capabilities can assist in interventions where distinguishing between different tissue types is crucial, such as in joint or soft tissue tumor ablations.
- •
Fluoroscopy : Fluoroscopy provides real-time X-ray imaging, which is valuable for guiding dynamic procedures such as fracture repairs and spinal injections. Robotic systems integrated with fluoroscopic imaging can adjust their positioning during the procedure, ensuring that instruments are accurately guided as the anatomy shifts.
- •
Ultrasound : Ultrasound imaging is a non-ionizing, real-time modality that is especially useful for guiding procedures involving superficial structures such as tendons and ligaments. Robotic systems can leverage ultrasound guidance to assist in minimally invasive interventions, offering enhanced visualization and targeting.
Integration of imaging and robotics
The integration of imaging modalities with robotic systems is central to the success of MSK interventions. Advanced software algorithms analyze the imaging data and translate it into actionable plans for the robotic system. These plans are either followed autonomously by fully active systems or used as a guide for semi-active and passive systems. For instance, in robotic-assisted tumor ablation, preoperative CT or MRI scans are used to identify the tumor margins and determine the ideal trajectory for the ablation probe. The robotic system then follows this trajectory with a high degree of accuracy, ensuring comprehensive coverage of the tumor while minimizing damage to surrounding tissues.
Technological advancements and robotic-assisted procedures
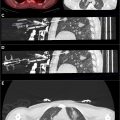
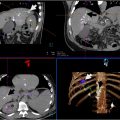
Regarding the role of musculoskeletal interventions of the interventional radiologist, robotic-assisted percutaneous interventions, such as biopsies, tumor ablation, and fracture repair, benefit from enhanced targeting and control. These procedures rely heavily on CT or ultrasound guidance to navigate the instruments precisely, minimizing collateral damage to surrounding tissues. Figure 1 demonstrates the planning of robot-assisted bone ablation to manage pain due to breast cancer lytic metastasis using the Epione system (Quantum Surgical, France). The process involves precise trajectory planning for ablation needle insertion. Multiple CT views are presented, including axial, coronal, sagittal, and 3D reconstructed images. The planned approach enables precise targeting of the lesion for thermal ablation. This as the opportunity to allow for decreased procedure and anesthesia or sedation time, with more accurate treatment based on probe and needle placement.