Image Sequencing: Problems and Solutions in Breast Evaluation
As is stressed throughout this text, imaging the breast can be divided into a few major tasks:
Find it.
Is it real?
Where is it?
What is it?
What should be done about it?
What was it?
What has been learned from it?
The major objective in breast imaging is the detection of breast cancers at a small size and early stage in an effort to reduce mortality. The screening mammogram is the most important study because it is the only opportunity to detect cancers earlier (find it). Once a potential abnormality is found, additional evaluation is frequently needed to determine the significance of the finding (Is it real?). If it is determined that a finding is real, then the radiologist must determine its location (Where is it?) so that he or she, if needed, can put a needle accurately into the lesion or guide a surgeon to the lesion. The radiologist must decide whether the lesion is benign or has the potential of being malignant and then what course of action to pursue to establish the diagnosis (What should be done about it). Following results (What was it?) is not only required by law, but is the only way to continue to improve. Learning what a lesion was helps to improve one’s interpretive skills (What has been learned from it?).
Basic Principles
Many of the “problem-solving” techniques described below are needed when using two-dimensional (2D) mammography (film/screen or digital). Once digital breast tomosynthesis (DBT) replaces conventional 2D mammography, many of the diagnostic problems described below will disappear. Superimposed tissues are eliminated by DBT. Margins can be more clearly analyzed using DBT. Morphology is more clearly defined, and the three-dimensional (3D) location of a lesion is easily determined using DBT.
Finding lesions requires high-quality imaging with proper positioning. Most problems in positioning can be avoided by having well-trained technologists who are compassionate and can work with the patient in an effort to obtain high-quality mammograms.
Assuming the images are of good quality, the first clinical problems that the radiologist is likely to encounter can frequently be resolved through additional images. These include altering the position of the breast relative to the x-ray beam, altering the angle that the x-ray beam takes as it passes through the breast, the use of spot compression to separate overlapping structures, and the use of magnification mammography to reduce noise and provide sharper images. Ultrasound is helpful in determining whether a lesion is cystic or solid, and whether it is amenable to ultrasound-guided aspiration, biopsy, or needle localization. Ultimately, computed tomography (CT), magnetic resonance imaging (MRI), and other tests may help resolve specific problems.
Mammographic Fluoroscopy
Mammographic evaluation is similar to fluoroscopy, without the fluoroscope. The principles used in fluoroscopy are those used to separate structures by mammography. Just as a compression paddle is used to separate overlapping loops of bowel under fluoroscopic observation, spot compression is used to separate overlapping breast structures. Rolling the breast and viewing it from different projections is the same as the fluoroscopist’s rolling the patient to use parallax shifts to distinguish separate structures. The only difference is that fluoroscopy is performed in real time, and with mammography it is the technologist who repositions and compresses the breast during the evaluation.
Is It Real?
Once a potential abnormality has been found, determining whether it is a real, 3D abnormality using 2D mammography can be a complicated process. Not all cancers form a visible mass, and there is the potential of dismissing an infiltrating process simply because a mass is not evident. The visualization of a finding on more than one additional projection may be required to determine whether it is three-dimensionally real or merely a projection artifact of superimposed normal structures. The tendency to rely only on conventional projections may be unnecessarily limiting. Although it is inconvenient, it is better to have the patient return for additional evaluation than to make a management decision based on insufficient information.
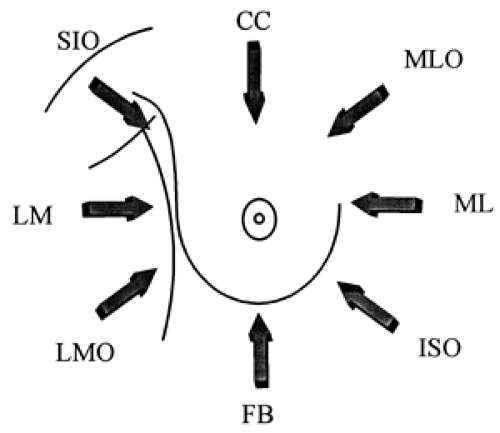
The basis of solving problems lies in varying the projections and reorienting the breast structures to provide a better understanding of the 3D relationships (Fig. 22-1).
Superimposed Normal Tissues Can Look Worrisome
Many names have been given to the fact that the projection of 3D structures within the breast as a 2D image can result in the superimposition of normal structures, one projected on another, creating the appearance of a worrisome finding. Sickles has termed these summation shadows. Whatever their name, 25% of the callbacks in our screening program prove to represent superimposed normal breast tissues. This is a bigger problem if single-view mammography is used for screening (1). Not only does single-view screening result in a higher recall rate, but more than 20% of cancers may be missed by using single-view screening (2). The available data suggest that screening should always use two-view mammography to reduce the recall rate and to diminish the chance that a cancer will be overlooked. DBT will eliminate callbacks for superimposed normal breast tissue.
Dissecting the Lesion
When an abnormality is suspected in one projection but is not evident in another, the radiologist should first try to dissect the various components of the finding to determine whether it is a true abnormality or merely a concatenation of separate structures. For example, it is not unusual for Cooper’s ligaments or small blood vessels to project over one another, forming an image that looks like a spiculated abnormality. True spicules do not pass across a lesion from one side to the other but rather emanate from and blend with its edge. If the abnormality can be made to fall apart as its components are dissected, it is not a real abnormality.
Comparing Projections
Another method of determining whether a suspected lesion is real is to determine its location on the projection on which it appears and then to evaluate the corresponding tissues in the other projection. There are two methods of triangulating a lesion in two projections: the arc method and the straight-line method. Neither is perfect, and the accuracy depends on positioning, compression, and the elasticity of the breast tissues.
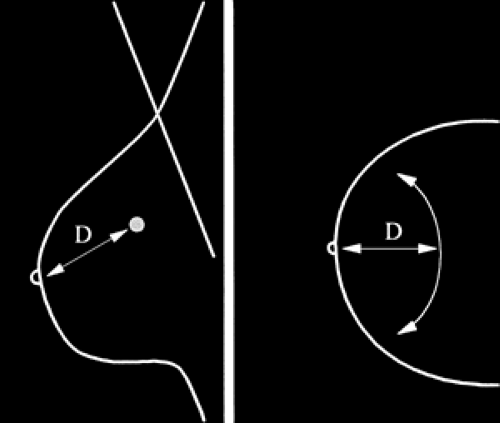
Arc Method of Triangulating Lesions
One of the methods commonly used for trying to find corresponding areas between mammographic projections involves using the distance from the nipple to the lesion as the radius of an arc with the nipple as its center. This distance is transferred to the other projection, and an arc is
swept with the nipple as the center. The tissue along this arc corresponds to the tissues that could contain the suspected lesion (Fig. 22-2). A real lesion should be found somewhere along (close to) this arc in the second image.
swept with the nipple as the center. The tissue along this arc corresponds to the tissues that could contain the suspected lesion (Fig. 22-2). A real lesion should be found somewhere along (close to) this arc in the second image.
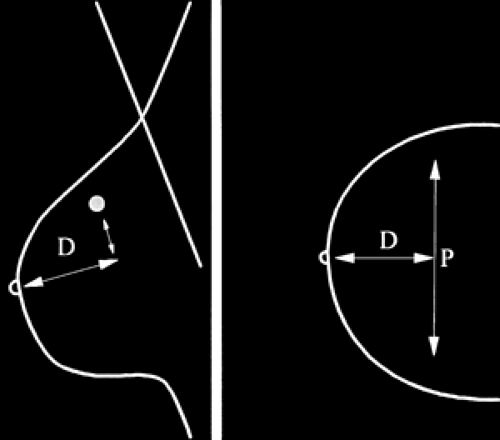
Cartesian, Straight-Line Method of Triangulating Lesions
A second method that is used to determine whether a lesion in one projection is the same as what is seen in the other is to measure the distance straight back from the nipple to a point where it is perpendicular to a line dropped from the lesion (Fig. 22-3). This distance is transferred to the other projection. If the lesion is real, it should be somewhere along a line perpendicular to the transferred line at the same distance from the nipple.
There have been two studies that compared these two methods, and they reached opposite conclusions as to which is the more accurate (3). We prefer the arc method.
These are crude measures. Since the breast is not a uniform shape, neither triangulation method is perfect, and lesions can sometimes seem to be at unexpected distances in the second projection. Once again, the use of DBT eliminates this problem.
Is It Reasonable to Expect That a Finding Is Real?
At times it is fairly obvious that a suspected abnormality is not real. If the breast tissues are predominantly fat and there is no suggestion of an abnormality in the corresponding location on the second view, then it is highly unlikely that the lesion is real. This decision should be made with caution, however, since cancers can be subtle.
Don’t Forget the Skin
If a lesion seen on one view is not immediately apparent on the second, the observer should also look carefully at the periphery of the breast at and just under the skin. This is especially true for calcifications seen in only one projection. They are frequently benign deposits in the skin. Methods to prove this are described later in this chapter.
Another possibility when something is seen in one view and not in the other is that it is an artifact. Scratches on the film, dust on the screen, and contaminants on the patient’s skin can all cause findings that are visible on a single view only.
Basic Approaches to Possible Superimposition of Tissues
Tissues that superimpose can be separated in several ways. By changing the path that the x-ray beam takes through the tissues or by changing the orientation of the tissues relative to the x-ray beam, what at first might appear to be a mass or a spiculated lesion can be shown to come apart when viewed from a different perspective.
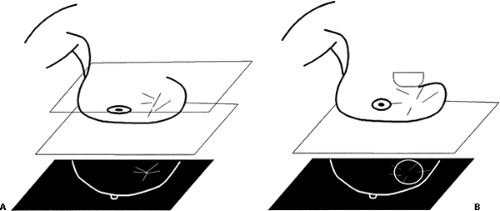
Spot Compression
Spot compression can be used to separate overlapping structures. The standard compression paddle presses on the tissues with only as much pressure as the least compressible
tissue volume. Spot compression places greater pressure on a smaller volume of tissue. This can displace tissues that overlap one another, reduce the amount of overlapping tissue, and push the tissues closer to the detector, reducing geometric blur (Fig. 22-4). What may initially appear as a significant abnormality can be shown to represent overlapping normal structures using spot compression (Fig. 22-5). It is often useful to use spot compression in addition to changing the position of the breast so that the same structures are not maintained in the same alignment as in the initial image.
tissue volume. Spot compression places greater pressure on a smaller volume of tissue. This can displace tissues that overlap one another, reduce the amount of overlapping tissue, and push the tissues closer to the detector, reducing geometric blur (Fig. 22-4). What may initially appear as a significant abnormality can be shown to represent overlapping normal structures using spot compression (Fig. 22-5). It is often useful to use spot compression in addition to changing the position of the breast so that the same structures are not maintained in the same alignment as in the initial image.
I have found that spot compression frequently demonstrates the same problem as standard compression despite the increased pressure. I prefer to use rolled views (described below) when trying to determine whether a finding is real or merely superimposed breast tissue.
Some radiologists like to perform the spot-compression images using magnification. This can be helpful, but it adds another layer of complexity and room for error because any motion can severely compromise the image sharpness, and this is more likely to occur due to the longer exposure times needed for magnification. The benefit of magnification is an improved ability to evaluate the margins of masses and the morphology of calcifications. If it is not certain whether a lesion is real, we generally use spot compression without magnification as the first step.
Angulation of the X-Ray System
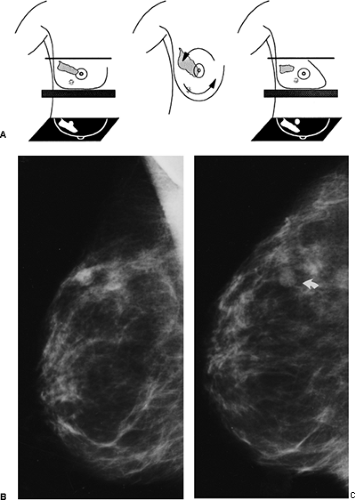
Another method for determining whether a finding is real is to change the angle at which that the x-ray beam passes through the tissues. If the breast is kept in the same position but the gantry is rotated 10 to 20 degrees and then the breast is recompressed, the x-ray beam will pass through different tissues, and a summation shadow can be made to fall apart into its normal tissue components (Fig. 22-6).
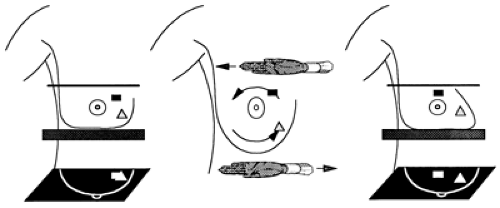
Modified Projections and Rolled Views
Just as the body is rolled under a fluoroscope to reorient overlapping structures, the breast may be rolled to accomplish the same result. The usual maneuver involves rolling the breast around the axis of the nipple (Fig. 22-7). By convention the direction of roll is determined by the movement of the top of the breast (e.g., top rolled laterally). It is occasionally useful to roll tissues from front to back (Fig. 22-8). This will also change the orientation of the various internal structures relative to the x-ray beam so that superimposed structures are not superimposed.
Not only are these maneuvers useful in determining if something is real, but by skillful and thoughtful repositioning, normal tissue that might obscure a lesion can be moved out of the way (Fig. 22-9).
Lesions Seen on Only One Projection
The most common problem occurs when a potential lesion is seen in one projection and not seen in the other view. This often means that the observation is the result of a benign superimposition of normal structures that has formed a summation shadow. The first question to be asked is, “Is it real?” and the following question is “Where is it?”
Additional evaluation should begin by determining whether the finding is a true abnormality.
Additional evaluation should begin by determining whether the finding is a true abnormality.
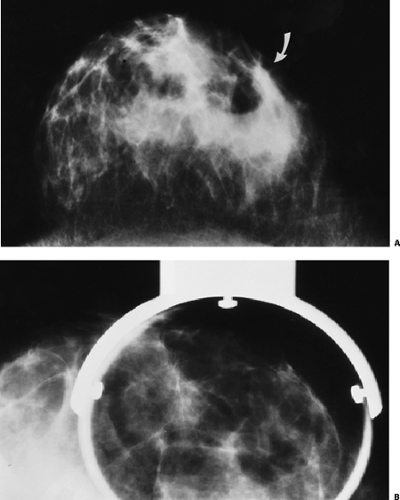 Figure 22-5 The initial CC projection (A) raised the question of a spiculated mass (arrow). On spot compression (B), however, this was clearly a superimposition of normal structures. |
Return to the Projection on Which the Lesion Appeared
When a suspected lesion is seen in only one projection, it is best to return to that projection and alter it slightly to determine whether the lesion is real or merely a superimposition of structures. If a potential abnormality is seen on the mediolateral oblique (MLO) projection, for example, and not seen on the craniocaudal (CC) projection, it is best to return to the MLO and work from there. If the lesion is not real, then it would be futile and would cause unnecessary radiation exposure to search for it by obtaining multiple altered CC projections. If it is not real, then it can never be found on the CC projection! If it is real, by imaging it using a projection that differs slightly from the original, in a predetermined fashion, the lesion can be shown to be real and its location can be determined by its apparent shift against the background of the normal breast structures between the two projections. Once the approximate location of the real abnormality is determined, the orthogonal
mammographic projection can be chosen appropriately to confirm the location and three dimensionality of the lesion.
mammographic projection can be chosen appropriately to confirm the location and three dimensionality of the lesion.
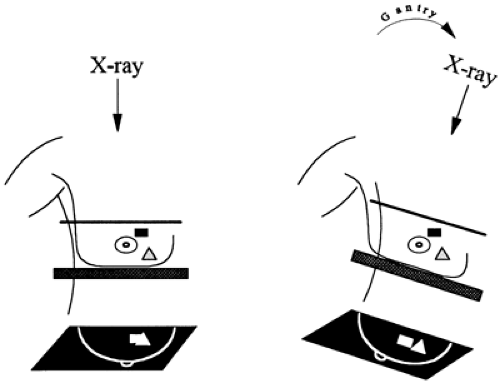 Figure 22-6 Rotating the gantry and recompressing at a different angle while the breast is kept in the same position can be used to separate normal overlapping structures. |
Problem: A lesion is seen on the MLO projection and not on the CC view. Is it real? The tendency is to obtain multiple projections in the CC position trying to identify the lesion. The fallacy in this approach is that the lesion may not, in fact, be real and thus will not be visible on these projections. It is best to obtain an additional image slightly altering the original position of the breast to determine whether the lesion is real. If a superimposition of structures is suspected, spot compression of the area may be sufficient to exclude a lesion.
Spot compression is a valuable technique, but the radiologist should always be aware that spot compression may squeeze a true lesion out from the field of view, leading to the incorrect impression that it is not real (Fig. 22-10). It is usually best to keep the collimation open on spot-compression views to permit the opportunity to recognize this problem (Fig. 22-11).
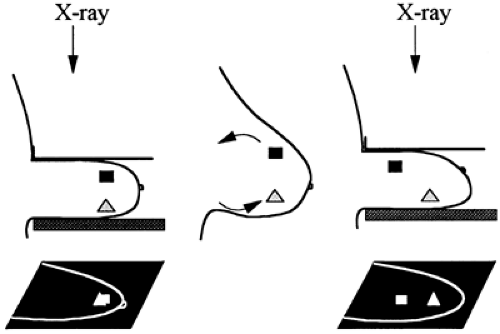 Figure 22-8 The breast can be rolled front to back to accomplish the same results as in the standard rolled views. |
The spot-compression view in the same projection may only produce the same superimposition of structures and not differentiate a true lesion from summation shadows. For lesions seen only on the MLO projection, it is frequently best to go immediately to the straight lateral projection. This slight shift in the orientation of the breast structures relative to the x-ray beam is often sufficient to demonstrate that an apparent abnormality is not real but rather a benign superimposition of normal structures (Fig. 22-12). If the lesion is real, its shift relative to the other structures of the breast between the two projections can help determine its location (see Triangulation of Breast Lesions), and this information can be used to guide positioning in the CC projection to confirm its 3D location.
Problem: A lesion is seen on the CC view and not on the MLO projection. When a lesion is seen only on the CC projection and not on the MLO, it is best to return to the CC position and alter the orientation of the breast relative to the x-ray beam to determine whether the lesion is real. This
may require only spot compression to demonstrate a benign superimposition of structures (Fig. 22-13).
may require only spot compression to demonstrate a benign superimposition of structures (Fig. 22-13).
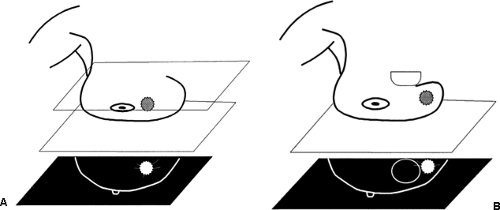 Figure 22-10 Spot compression can push the lesion out of the field of view. A suspicious lesion is evident with full compression (A). On spot compression the lesion is pushed out of the field of view (B)
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|