Pulmonary hypertension is a rare but important clinical problem that presents a sometimes challenging diagnostic dilemma. The diagnosis of pulmonary hypertension relies on a combination of clinical testing and radiologic imaging, with chest computed tomography (CT) often serving as the primary imaging modality for comprehensive evaluation of the chest. Chest CT can be used to evaluate for causes of pulmonary hypertension including chronic lung disease, pulmonary artery obstruction, and congenital heart disease. Recognizing common appearances of these conditions will enable expedient diagnosis.
Key points
- •
Pulmonary hypertension can cause significant morbidity and mortality.
- •
Diagnosis of pulmonary hypertension proceeds stepwise, with tests ordered to exclude the most to least common causes of pulmonary hypertension.
- •
Pulmonary hypertension is classified into 5 groups in the World Health Organization (WHO) classification.
- •
Patients can have pulmonary hypertension from more than one WHO group.
- •
Chest computed tomography is useful in evaluating for conditions in all 5 WHO groups.
Introduction
Pulmonary hypertension (PH) is a pathologic state characterized by elevated pressure in the pulmonary arteries and sometimes the pulmonary veins. If left untreated, PH can lead to significant morbidity and mortality. Epidemiologic data on PH of all causes are sparse. One population-based cohort study in Canada showed the annual incidence and prevalence to be 0.029% and 0.127% in 2012, respectively. Interestingly, this represented an increase in incidence and prevalence by 20% and 28%, respectively, from 2002.
Suspicion for PH may arise from abnormal clinical presentation or incidental detection of secondary features of PH on diagnostic testing. When there is sufficient concern, a diagnostic workup is pursued to first confirm a diagnosis of PH and followed by determination of the underlying cause. Imaging plays an important role in the detection, diagnosis, and management of PH. It is important for radiologists to recognize the underlying causes of PH and their respective imaging findings because identification of these patients allows for initiation of treatment strategies to mitigate the detrimental effects of longstanding PH. The following discussion will focus on the evaluation of PH, utility of imaging, and imaging appearance of common causes of PH.
Definition of pulmonary hypertension
PH occurs with elevated pulmonary vascular resistance and pulmonary artery pressure, which may be caused by 1 or more factors including abnormalities of pulmonary blood flow and cardiac function, hypoxic vasoconstriction, or exposure to toxins or metabolites.
Sustained elevation of the mean pulmonary artery pressure (mPAP) is diagnostic of PH. Normal mPAP is 14 ± 3 mm Hg at rest and mPAP greater than 20 mm Hg is considered elevated. Previously, PH was defined by an mPAP ≥25 mm Hg, with mPAP of 21 to 24 mm Hg classified as borderline PH, necessitating further evaluation. , However, increasing evidence has shown greater mortality in patients with mPAP of 21 to 24 mm Hg compared to those with mPAP ≤20 mm Hg. As a result, the 2022 European Society of Cardiology /European Respiratory Society Guidelines for the diagnosis and treatment of PH reclassified mPAP greater than 20 mm Hg as diagnostic of PH. ,
Classification of pulmonary hypertension
The World Health Organization (WHO) classification of PH is the most widely recognized and used classification system for the diagnosis and management of patients with PH ( Table 1 ). This system divides cases of PH into 5 groups based on underlying etiology and is helpful for offering insight into potential management strategies.
| World Health Organization (WHO) Group | Disorders | Pathogenesis | Radiologic Imaging | Treatment Approach |
|---|---|---|---|---|
| 1 | Idiopathic, heritable, substance-induced, CTD, human immunodeficiency virus, portal hypertension, simple cardiovascular shunts, PVOD, PCH | Proliferative vasculopathy affecting pre-capillary pulmonary arterioles or venules | Chest computed tomography | Vasodilators, treatment of underlying problem (eg, congenital heart disease) |
| 2 | Left heart failure, valvular heart disease | Pulmonary venous hypertension due to poor forward flow | Cardiac CT/MR imaging in specific cases | Treatment of heart failure or heart transplant |
| 3 | Lung disease, hypoxia | Poorly understood pathogenesis | High-resolution chest CT | Treatment of lung disease or lung transplant |
| 4 | Pulmonary artery obstruction | Mechanical flow obstruction | Chest computed tomography angiography (CTA) | Removal of pulmonary artery obstruction |
| 5 | Hematologic disorders, metabolic disorders, complex CHD | Multifactorial or idiopathic | Chest CT/CTA Cardiac CT/MR imaging | Treatment of underlying factors, vasodilators may be considered |
Diagnostic evaluation of pulmonary hypertension
PH is sometimes discovered during an investigation into the cause of various symptoms such as progressive shortness of breath, chest pressure/pain, and dizziness. , Due to the nonspecific nature of these symptoms and insidious onset, there is often a diagnostic delay of about 2 years from initial onset of symptoms, often longer in younger patients. Once clinical suspicion for PH is raised, several diagnostic tests are performed including pulmonary function testing, arterial blood gases, and various blood tests such as complete blood count and human immunodeficiency virus assay. Additional laboratory tests may be considered in select cases, such as connective tissue disease serologies. Finally, a variety of imaging tests are used.
As left heart failure is the most common cause of PH, echocardiography is often the first diagnostic examination in the evaluation of PH. Beyond cardiac function, echocardiography can detect secondary features suggestive of PH such as right ventricular hypertrophy or dilation as well as indirectly estimate pulmonary arterial pressures. , In select cases, cardiac MR imaging can be used to assess cardiac function and morphology and to detect underlying cardiomyopathies contributing to or causing PH.
The second most common cause of PH is chronic lung disease. As a result, chest radiographs and noncontrast chest computed tomography (CT) are often performed early in the evaluation of PH to identify chronic lung conditions such as chronic obstructive pulmonary disease (COPD) and fibrotic interstitial lung disease (ILD), which are associated with development of PH. Noncontrast chest CT enables accurate characterization of the severity and extent of lung disease if present.
If cardiac and pulmonary parenchymal causes are not thought to be the cause of PH, ventilation-perfusion scan and CT pulmonary angiography are performed to evaluate for pulmonary artery obstructions.
If noninvasive testing does not reveal a cause for PH, right heart catheterization (RHC) can confirm a diagnosis of WHO Group 1 PH. Furthermore, RHC offers the ability to measure the (mPAP) and determine whether the patient has pre-capillary and/or post-capillary PH as well as ascertain disease severity. Becoming familiar with the results of RHC is helpful for understanding potential causes of PH ( Table 2 ).
| Hemodynamic Type | Right Heart Catheterization Metrics | WHO Group |
|---|---|---|
| Precapillary | Pulmonary venous hypertension: Absent | 1, 3, 4, 5 |
| Pulmonary vascular resistance: High | ||
| Postcapillary | Pulmonary venous hypertension: Present | 2, 5 |
| Pulmonary vascular resistance: Low | ||
| Precapillary and postcapillary | Pulmonary venous hypertension: Present | 2, 5 |
| Pulmonary vascular resistance: High |
Approach to pulmonary hypertension on radiologic imaging
Although knowing the typical sequence of diagnostic testing for PH is helpful, the etiology is not always clear. Patients do not always fall under a single WHO Group. Furthermore, suspicion for PH may be raised either through clinical assessment or through imaging. As such, the role the radiologist plays can differ depending on the stage of the diagnostic evaluation.
Because chest radiographs and CT are the most common initial imaging tests performed in patients being evaluated for PH, the remainder of this article will focus on these 2 modalities and potential findings signaling specific causes of PH.
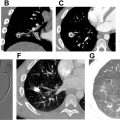
Chest radiography
Chest radiography is a first-line imaging test to evaluate for signs of PH and detect overt heart or lung disease as a potential etiology. Features of PH on chest radiography include dilation of the main, hilar, and intrapulmonary pulmonary arteries, vascular pruning, pronounced definition of intrapulmonary vascular margins, and right atrial and ventricular dilation ( Fig. 1 ). Heart disease can manifest with cardiac silhouette enlargement and pulmonary edema, which can be suggested by indistinct vascular margins, increased central pulmonary vascular caliber, vascular redistribution, Kerley B lines, perihilar opacities, and pleural effusion. Pulmonary causes of PH are grouped into obstructive and restrictive lung diseases. Obstructive lung disease such as COPD can produce pulmonary hyperlucency and hyperinflation, with widening of the AP thoracic diameter and flattening of the diaphragm. Restrictive lung disease such as pulmonary fibrosis can cause coarse reticular opacities, traction bronchiectasis, architectural distortion, and reduced lung volume. Further characterization of these findings is performed with chest CT.

Chest computed tomography
The typical protocol for a comprehensive evaluation of ILD is a helical scan from the clavicles through the diaphragm with less than 1.5 mm axial reconstructions in sharp and soft tissue kernels with coronal and sagittal multiplanar reformats. Additionally, expiratory imaging, either static or dynamic, is necessary to assess for air trapping. Depending on institutional protocol or ordering physician preference, intravenous contrast may or may not be administered for the examination. If evaluation of the pulmonary arteries in the setting of chronic thromboembolic disease is desired, it is advisable to perform the study using bolus tracking with the trigger region of interest (ROI) placed on the main pulmonary artery, with trigger threshold set to 150 to 200 Hounsfield unit (HU), or on the left atrium with a trigger threshold set to blood pool + 60 HU to ensure adequate enhancement of the pulmonary arteries. The next sections discuss the typical findings of PH grouped by organ system.
Vascular findings
Pulmonary Artery Dilation
Often PH is discovered incidentally when the pulmonary arteries are dilated. The Framingham Heart Study found that the 90th percentile for main pulmonary artery (MPA) size on noncontrast thoracic CT is 29 mm in males and 27 mm in females. When the ratio of the MPA to the ascending aorta at the level of the bifurcation of the right pulmonary artery was measured, the 90th percentile for MPA-to-ascending aorta ratio was 0.91. Studies show that MPA diameter ≥ 29 mm is predictive of PH with sensitivity, specificity, positive predictive value, and negative predictive value of 87% to 88%, 42% to 89%, 70% to 97%, and 70%, respectively. , To avoid overdiagnosis of PH, some groups advocate a higher size threshold to raise the concern for PH. One study found that a threshold of MPA diameter greater than 29.5 mm was 71% sensitive and 79% specific for PH while raising the threshold to 31.5 mm increased the specificity to 90% at the cost of a sensitivity of 52%. An improved specificity can reduce the need for further invasive testing to workup for PH.
Pulmonary Artery Filling Defects
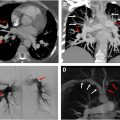
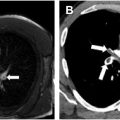
Pulmonary artery filling defects, most commonly pulmonary embolism, can cause elevation of pulmonary artery pressures. Acute elevation of pulmonary artery pressure results in dilation of the main pulmonary artery, offering insight into the hemodynamic significance of the filling defect ( Fig. 2 ). Chronic pulmonary artery mechanical obstruction leading to PH is quite rare. Causes of WHO Group 4 PH include flow obstruction due to chronic thromboembolic PH (discussed in a separate article in this issue) and, rarely, neoplasms such as pulmonary artery intimal sarcoma ( Fig. 3 ).



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree