Abstract
Rectus sheath hematomas are most commonly observed in elderly patients on anticoagulation and may require embolization when there is accompanying hemodynamic instability or vascular injury. We present a case of an inferior epigastric pseudoaneurysm and rectus sheath hematoma treated by percutaneous direct sac puncture with N‑butyl cyanoacrylate (NBCA) glue due to complex vascular anatomy and body habitus which limited an intra-arterial approach. While superficial pseudoaneurysms are often managed with thrombin, liquid embolics may offer improved penetration into the afferent and efferent supply of the pseudoaneurysm, thereby limiting re-bleeding risk.
Introduction
Rectus sheath hematomas (RSH) are a rare cause of abdominal pain, often associated with abdominal wall trauma and anticoagulation, particularly in elderly patients [ ]. Vascular injury, especially involving the inferior epigastric artery, is more common below the arcuate line due to the absence of a posterior sheath. Additional vascular supply to the rectus sheath includes the superficial epigastric artery and rarely the deep circumflex iliac artery [ ].
While most RSHs are managed conservatively, those with vascular complications or hemodynamic instability may require embolization. Transcatheter arterial embolization (TAE) is well-documented for RSH management, with microcoils and gelfoam being the most commonly used embolic agents (3). However, re-bleeding remains a problem due to retrograde flow from collaterals, vessel recanalization, and loss of tamponade effect. Several studies have demonstrated the safety and efficacy of liquid embolic agents such as NBCA for RSH treatment. NBCA offers advantages including controlled penetration into both afferent and efferent feeders, reducing recanalization risk, and maintaining its effectiveness regardless of coagulopathic status [ ]. Superficial pseudoaneurysms with challenging vascular anatomy may benefit from direct percutaneous approaches, often treated with thrombin [ ].
This case highlights the use of NBCA for direct sac puncture and embolization of an inferior epigastric pseudoaneurysm, providing an alternative to conventional thrombin injection or TAE.
Case presentation
A 72-year-old female with a past medical history of heart failure with preserved ejection fraction (HFpEF), atrial fibrillation on Eliquis, and an abdominal aortic aneurysm (AAA) status post endovascular aneurysm repair (EVAR), complicated by Type 2 endoleak, presented with abdominal pain and swelling at an outside hospital after straining to use the restroom. She was diagnosed with an abdominal wall hematoma, treated conservatively, and subsequently discharged. She then presented to our ED with worsening abdominal swelling and pain.
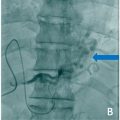
The patient was hemodynamically stable on presentation with hemoglobin of 8.5 which subsequently downtrended to 6.3. CTA of the abdomen and pelvis revealed a large left rectus sheath hematoma with a left inferior epigastric pseudoaneurysm, but no evidence of active extravasation ( Figs. 1 and 2 ). IR was consulted for embolization ( Fig. 3 ).