MR imaging evaluation of hamstring tendons reveals their association with subgluteal posterior hip pain, emphasizing the superiority of MR imaging over ultrasound due to the deep location of the hamstrings. This review encompasses various conditions, including overuse tendinopathy, metabolic disorders, and sports-related injuries prevalent in elite and recreational athletes. Practical MR imaging-guided approaches tailored to clinical needs and therapeutic options are discussed, highlighting MR imaging’s crucial role in monitoring postinjury healing. Furthermore, potential residual complications are outlined, underscoring MR imaging’s significance in diagnosing, treating, and evaluating hamstring tendon-related ailments comprehensively.
Key points
- •
Accurate MR imaging assessment relies on comprehensive anatomic knowledge and specific acquisition protocols, essential for diagnosing hamstring tendon issues associated with subgluteal posterior hip pain effectively.
- •
The diverse range of conditions, from overuse or mechanical load tendinopathy to metabolic disorders and sports-related injuries, affects athletes across all levels and can be differentiated by specific imaging features discernible through MR imaging.
- •
Utilizing practical MR imaging-guided approaches enables the tailoring of therapeutic options, ensuring personalized treatment plans ranging from conservative management for tendinopathy, apophysitis, or some partial tendon injuries to surgical intervention for complete ruptures or avulsions.
- •
MR imaging plays a crucial role in monitoring the recovery journey postinjury, providing vital information about treatment efficacy, and identifying potential complications such as muscle atrophy, fatty muscle degeneration, chronic cystic hematomas, abnormal calcifications, fibrous tracts, or sciatic nerve issues.
Introduction
Hamstring tendon injuries (HTIs) are the most common muscle injuries in sports. Despite recent advances in injury risk mitigation initiatives and therapeutic rehabilitation strategies, the rates of hamstring muscle injuries have increased over time with a high rate of recurrence. This has motivated the world of professional sports to focus on the study of these injuries. , Additionally, proximal hamstring tendinopathies not only affect the realm of professional sports but also affect recreational and amateur sports, as well as middle-aged and elderly patients. Factors such as overuse and other conditions, metabolic diseases that predispose to tendon degeneration and calcifications, can lead to limitations in performing routine daily activities.
The hamstring tendons include the semimembranosus (SM), semitendinosus (ST), and the biceps femoris long head (BFlh), all of which have their origin along the ischial tuberosity. , However, the complex anatomy, structure, and function of the hamstrings , make it difficult to approach these injuries in terms of imaging diagnosis and prognosis.
MR imaging has established itself as the most precise imaging technique in the assessment of tendon structures at this level, giving rise to several classification systems for acute hamstring injuries. MR imaging has proven to be useful not only in the initial diagnosis of hamstring injuries but also as follow-up to assess the reparative process. When assessing HTIs, it is crucial to have a dedicated MR imaging protocol as well as a systematic interpretation algorithm focused on pattern recognition of acute hamstring injuries.
In a patient presenting with deep buttock pain, MR imaging can reveal a wide array of conditions, which may depend on the clinical history of the affected individual. In younger patients, involvement often occurs at secondary ossification centers, giving rise to a condition known as apophysitis. Conversely, in patients with a mature skeleton, tendon abnormalities are more common and may even involve tendon rupture. The spectrum of hamstring tear ranges from a small insertional or noninsertional partial tendon tear to an avulsion of one or both tendon origins from the ischial tuberosity, which impacts management. Although many of these lesions are treated conservatively, an accurate evaluation of the extent and exact location of the lesions is essential for identifying potentially surgical cases.
The diagnosis of hamstring injury can be made in the acute or chronic phase. Adequate MR imaging characterization of the type of lesion is important both at the time of initial diagnosis as well as when assessing the progression of the healing process. , , During the follow-up of injuries, MR imaging has proven effective not only in recognizing healing but also in identifying the cause of persistent pain due to complications such as refractory tendinopathies, severe atrophy, chronic hematomas, calcifications, or involvement of the sciatic nerve.
The aim of this study is to highlight the role of MR imaging in the diagnosis and follow-up of acute hamstring injuries including the expected evolution of MR imaging findings during rehabilitation or after surgery.
Anatomic and histologic features
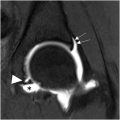
The hamstring tendons originate at the ischial tuberosity at distinct bony facets. , The tendons of the BFlh and ST are typically conjoined and take off from a larger ovoid inferomedial facet located more posteriorly and are reinforced by the sacrotuberous ligament. In addition to the common tendon origin, muscle fibers of the ST are often seen attaching directly into the ischial tuberosity (myo-osseous insertion). , As this portion of the tendon does not have anchored muscle fibers of the long head of the biceps, some authors call it the free tendon. It is important to highlight the relationship between the tendon insertion of the hamstrings and the ischiocondylar portion of the adductor magnus, which inserts into the same ischial tuberosity but more caudally. Below the ischium, the muscle bellies of the BFlh and ST meet the conjoint tendon, with the ST appearing immediately below the ischium medial to the tendon. The biceps femoris muscle belly appears more distally, lateral to its tendon longer free tendon approximately 10 cm below the ischium. , Understanding these specific characteristics aids in recognizing that, depending on the lesion’s location, either both muscular bellies or only one muscle belly may be affected ( Fig. 1 ).

Standardized nomenclature has been proposed to describe tendon structure and the distribution of the extracellular matrix (ECM) with the aim of understanding the transitions among the tendon origin, the free tendon, and the intramuscular tendon. The structural composition of the isolated intramuscular tendon significantly differs from that of the free tendon. Histologically, it is unlikely to exhibit the well-aligned fascicular bundles and specialized interfascicular matrix characteristic of free tendon tissue. Instead, the intramuscular tendon primarily consists of type 1 collagen, with a more reticular organization at the ECM level likely related to the accumulation of muscle forces from varying angles of pennation. , While the free tendon can withstand high strain rates for energy storage and release, the intramuscular tendon, lacking fascicular bundles and interfascicular matrix, exhibits greater functional stiffness. It is crucial to know these characteristics to accurately determine the exact location of the injury and thus ensure correct patient management.
MR imaging protocol
Although ultrasound has proven to be sensitive and cost-effective in the early detection and grading of muscle injuries and is widely used in this regard, it has limitations in discerning connective tissue injuries of deep tendon structures.
Specialized imaging techniques such as 3 Tesla (T) or optimized 1.5 T MR imaging offer exquisite resolution for defining muscle injuries, allowing acquisitions in 3 planes facilitating assessment of the hamstrings. , , To achieve higher resolution images, it is recommended to use a multipurpose surface coil with high channel density. It is essential to mark the site of symptoms to ensure comprehensive coverage and accurate assessment, especially in cases with multiple imaging findings. Typically, the patient is positioned in a supine position, and after an initial coronal bilateral acquisition, the examination focuses exclusively on the injured limb area marked with a vitamin E capsule, as determined by clinical findings.
Protocols should be tailored to ensure thin sections (eg, <4 mm), appropriately small field of view (FOV; eg, <30 × 30 cm), , and multiplanar acquisitions (axial, coronal, and sagittal). Utilizing fluid-sensitive sequences with an intermediate echo time (TE; eg, <65 milliseconds) is advantageous as it provides sufficient contrast and spatial resolution for examining connective tissues. These sequences are instrumental in delineating connective tissue with precision and in identifying edematous changes surrounding the tendons and myoconnective junctions, thereby facilitating the detection of intramuscular or intermuscular fluid collections or hematomas. , Additionally, T1-weighted sequences are crucial for assessing subacute hemorrhage or hematoma, detecting atrophy and fatty infiltration, and revealing scar tissue, thus contributing to a clearer understanding of the healing process. ,
The recommended MR imaging protocol for acute and follow-up assessment in proximal hamstring injuries is shown in Table 1 .
| MR Imaging Characteristics | |||||
|---|---|---|---|---|---|
| Parameters | Bilateral | Unilateral | |||
| Sequences | Coronal TSE intermediate-weighted image | Axial fat-suppressed TSE intermediate-weighted image a | Axial TSE T1-weighted image a | Coronal fat-suppressed TSE intermediate-weighted image a | Coronal TSE T1-weighted image |
| TE, ms | 44 | 44 | 11 | 44 | 11 |
| Repetition time, s | 2700 | 2900 | 750 | 2700 | 980 |
| Section thickness, mm | 2.5 | 3.5 | 3.5 | 2.5 | 2.5 |
| Interslice distance, mm | 0.6 | 0 | 0 | 0.6 | 0.6 |
| Field of view, cm | 30 × 40 | 25 × 25 | 25 × 25 | 26 × 29 | 26 × 29 |
Diagnostic and treatment approach for acute injuries
MR imaging strategies for acute musculoskeletal injuries enable the diagnosis of conditions, such as apophysitis, avulsions, tendinopathy, or tears, tailored to factors like patient age, trauma mechanism, and injury characteristics. Additionally, MR imaging serves as a valuable tool for monitoring the healing process, offering precise evaluation, treatment guidance, and identification of potential complications. Table 2 shows the MR imaging findings in acute spectrum of proximal HTIs.
| Type of Injury | Clinical Peculiarities | MR Imaging Findings |
|---|---|---|
| Apophysitis | Deep subgluteal pain that affects patients with immature skeletal development over time, following repetitive thigh flexions and extensions of the knee | Marrow edema around the physeal cartilage without disruption or displacement. Usually not associated with hematoma or peritendinous fluid |
| Avulsion fracture | Pain associated with a “popping” sensation that affects patients with immature skeletal development following a rapid forced hyperflexion of the hip and extension of the knee | An avulsed bone fragment of the ischial tuberosity is observed, usually associated with hematoma and/or peritendinous fluid |
| Overuse (mechanical loading) tendinopathy | Discomfort and/or pain in the lower gluteal area, occasionally extending along the hamstring muscles to the back of the thigh | Thickened tendons with a slight increase in signal intensity on fluid-sensitive sequences, without discontinuities. Sometimes are associated with peritendinous edematous changes |
| Calcific tendinopathy | Deep subgluteal pain that usually affects middle-aged patients. Associated with diabetes, thyroid and estrogen endocrine disorders | Common findings with overuse tendinopathy including calcific deposits, which appear as focal areas of low signal on all MR imaging sequences, typically near tendon insertions |
| Avulsion tendon and complete tendon rupture | Pain associated with a “popping” sensation that affects patients with mature skeletal development following a rapid forced hyperflexion of the hip and extension of the knee | Complete tendon tear at the bone–tendon junction or at the tendon, presenting as a hyperintense transversal gap on T2 imaging with evident loss of tendon continuity, often with tendinous retraction and loss of tension. Usually associated with hematoma or peritendinous fluid |
| Partial tendon Tear | Pain and discomfort following a rapid forced hyperflexion of the hip and extension of the knee | Tendinous hyperintense transverse or longitudinal gaps on T2, which do not affect the full thickness of the tendon and are not associated with retraction or only with minimal retraction, sometimes accompany hematoma or peritendinous fluid |
Apophysitis and Avulsion Injuries
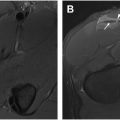
The diagnostic approach to HTIs depends on many factors such as the age of the patient. In skeletally immature children, since the weak point in the bone–tendon–muscle chain is the open physis, an acute hamstring injury often leads to injury of the ischial apophysis. Avulsion injuries at the origin of the hamstrings result from forceful eccentric muscle contraction or excessive passive lengthening. In less severe cases of repetitive injury, apophysitis may occur, resulting in marrow edema around the physeal cartilage without actual disruption or displacement. This can be challenging if not impossible to detect without MR imaging. , In apophysitis, the typical presentation is that of pain in the deep gluteal/ischial tuberosity region. When the pain is accompanied by loss of function and severe tenderness, one should suspect an avulsion injury. Avulsion fractures of the ischial apophysis typically present as a crescent-shaped bone fragment inferiorly adjacent to the ischium on radiographs. , On MR imaging, the avulsed fragment is accompanied by a significant increase in fluid signal intensity at this level. Fractures with displacement greater than 2 cm are often treated surgically, whereas less displaced avulsed apophysis may be treated conservatively depending on the sport and level of the player. MR imaging can also reveal associated hematoma, periosteal stripping, and laxity of the avulsed tendons. Fig. 1 and Fig. 2 show the different appearances of apophysitis and apophyseal fractures.

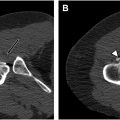
In the mature skeleton, especially in professional athletes, avulsions may involve both tendons or selectively involve the common tendon BFlh/ST or the SM tendon. Patients frequently describe experiencing pain accompanied by a “popping” sensation when sustaining this injury. , Typically, MR imaging reveals a complete tendon tear at the bone–tendon junction, presenting as a hyperintense gap on T2 imaging with evident loss of tendon continuity, often with tendon retraction and loss of tension ( Fig. 3 ). Traumatic hamstring avulsion injuries in athletes necessitate prompt surgical intervention to reattach the tendon to the ischial tuberosity. , Neglecting to address this could result in irreversible consequences such as atrophy and fatty infiltration of the hamstring muscles. Another potential complication, less frequent but nonetheless important, is the involvement of the sciatic nerve, which can occur due to compression by the avulsed fragment, irritation from the hemorrhage, and subsequently from perineural adhesions in the context of healing.

Hamstring Proximal Tendinopathy
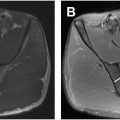
Proximal hamstring tendinopathy manifests as enduring buttock discomfort occurring during activities such as running, sitting, and lunging. It predominantly impacts not only active individuals in sports like track and field, long-distance running, soccer, and rugby but can nonathletes. , The primary symptom of proximal hamstring tendinopathy is discomfort in the lower gluteal area, occasionally extending along the hamstring muscles to the back of the thigh. During clinical assessment, tenderness over the ischial tuberosity is sometimes observed. Tendinopathy is the preferred term for persistent tendon pain and loss of function related to mechanical loading, with specialists advocating against the use of alternative terms like tendinosis. Thickened tendons with a slight increase in signal intensity on fluid-sensitive sequences are classic MR signs of tendinopathy ( Fig. 4 ). It is common to have bilateral hamstring tendinopathy. This may be symmetric or asymmetric, and it may or may not be associated with symptoms. Imaging findings such as peritendinous edema, fibrillar tears, or bone marrow edema can be associated with tendinopathy ( Fig. 5 ). , , Zissen and colleagues reported greater overall sensitivity for MR imaging in identifying pathologic abnormalities in both chronic and acute-on-chronic hamstring conditions, particularly peritendinitis, with peritendinous fluid or edema seen in 62.9% of patients on MR imaging compared to only 20% on ultrasound. As expected, MR imaging was the sole modality capable of detecting associated bone marrow edema within the ischial tuberosity.


Managing proximal hamstring tendinopathy poses a significant challenge. Typically, treatment of overuse tendinopathy relies on conservative management, such as stretching exercises and peritendinous corticosteroid injections. However, if these methods prove ineffective, surgery may be considered. Surgical treatment involves tenotomy of the SM tendon, followed by suturing it to the BFlh tendon, followed by release of any possible adhesions around the sciatic nerve.
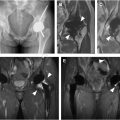
But not all tendon pathologies are solely attributed to overuse or mechanical loading; some are determined by metabolic factors that predispose individuals to develop them. An increased occurrence of hydroxyapatite crystal deposition disease (HADD) has been observed in patients with diabetes, thyroid and estrogen endocrine disorders, as well as certain genes such as the human leukocyte antigen serotype A1 (HLA-A1) genotype, and variations in tissue transglutaminase 2 and osteopontin. Nevertheless, the precise correlation and underlying pathogenesis remain unclear. An example of this is crystal deposition tendinopathy, which typically involves the accumulation of crystals such as calcium pyrophosphate dihydrate (CPPD) or hydroxyapatite within tendons, leading to inflammation and structural changes ( Fig. 6 ). Calcific deposits appear as focal areas of low signal on all MR imaging sequences, typically near tendon insertions. While MR imaging is the best modality for the assessment of inflammatory changes and for other causes of hip pain, it is important to note that HADD can have an aggressive appearance. During the acute resorptive phase, associated edema can be extensive and mimic trauma or infection. Cortical erosion, periosteal reaction, and marrow involvement have been described and may be confused for an infectious or neoplastic process such as a chondroid lesion. Scientific research has shown that MR imaging is highly effective in detecting and characterizing crystal deposition tendinopathy. For example, a study by Filippou and colleagues reported good sensitivity of MR imaging in identifying CPPD crystal deposition within tendons. Similarly, a review by Mallinson and colleagues underscored the importance of MR imaging in distinguishing crystal deposition tendinopathy from other tendon pathologies, enabling targeted interventions and improved patient outcomes. However, small deposits may present difficulties in visualization on MR imaging scans; therefore, if HADD is suspected, particularly in an atypical location, radiographs can be obtained to validate the diagnosis. Moreover, integrating gradient echo pulse sequences into the protocol could enhance the detection of calcification by leveraging susceptibility artifacts.