Ischiofemoral impingement is a syndrome defined by hip pain associated with narrowing of the space between ischial tuberosity and lesser trochanter. This phenomenon leads to abnormalities of the quadratus femoris muscle, ranging from deformity and edema to tears and atrophy. This review article presents an up-to-date discussion and imaging findings of ischiofemoral impingement, along with its related anatomy, clinical presentation, differential diagnosis and treatment.
Key Points
- •
Ischiofemoral impingement syndrome is defined by hip pain related to narrowing of the space between the ischial tuberosity and lesser trochanter, with abnormalities of the quadratus femoris muscle.
- •
Narrowing of the ischiofemoral space may be positional, congenital, or acquired.
- •
Plain radiographs may show chronic osseous changes of impaction between lesser trochanter and ischium. Magnetic resonance imaging is the standard imaging method to diagnose ischiofemoral impingement, showing edema and deformity of the quadratus femoris muscle belly at the site of maximal narrowing. In patients with long-standing impingement, quadratus femoris muscle fatty infiltration and atrophy may be present.
- •
Associated findings include abnormalities of the hamstring tendons, iliopsoas tendon insertion, and bursalike formations.
Introduction
Ischiofemoral impingement (IFI) syndrome is defined by hip pain related to narrowing of the space between the ischial tuberosity and lesser trochanter with abnormal morphology and/or magnetic resonance (MR) imaging signal intensity of the quadratus femoris muscle (QFM).
Ischiofemoral narrowing was first described by Johnson in 1977 in 3 patients with persistent hip pain after surgery, 2 of them after hip arthroplasty and 1 of them after proximal femoral osteotomy. In all cases, pain and narrowing of ischiofemoral space (IFS) were relieved after a lesser trochanter resection.
More recently, hip pain related to narrowing of IFS on cross-sectional imaging and abnormalities of QFM were reported in patients without history of surgery or trauma, supporting IFI as an entity that clinicians, orthopedic surgeons, and radiologists should be aware of.
IFI has been reported to be bilateral in 25% to 40% of cases. It is more frequent in women and affects all ages, ranging from 11 to 77 years. Nonspecific hip pain is a frequent symptom, with duration varying between months and several years.
Introduction
Ischiofemoral impingement (IFI) syndrome is defined by hip pain related to narrowing of the space between the ischial tuberosity and lesser trochanter with abnormal morphology and/or magnetic resonance (MR) imaging signal intensity of the quadratus femoris muscle (QFM).
Ischiofemoral narrowing was first described by Johnson in 1977 in 3 patients with persistent hip pain after surgery, 2 of them after hip arthroplasty and 1 of them after proximal femoral osteotomy. In all cases, pain and narrowing of ischiofemoral space (IFS) were relieved after a lesser trochanter resection.
More recently, hip pain related to narrowing of IFS on cross-sectional imaging and abnormalities of QFM were reported in patients without history of surgery or trauma, supporting IFI as an entity that clinicians, orthopedic surgeons, and radiologists should be aware of.
IFI has been reported to be bilateral in 25% to 40% of cases. It is more frequent in women and affects all ages, ranging from 11 to 77 years. Nonspecific hip pain is a frequent symptom, with duration varying between months and several years.
Anatomy
The QFM is a flat and quadrilateral muscle, situated along the posterior aspect of the hip joint. It originates at the anterior portion of the ischial tuberosity and inserts on the posteromedial aspect of the proximal femur. The QFM is bordered by the obturator externus muscle anteriorly, sciatic nerve posteriorly, inferior gemellus superiorly and adductor magnus inferiorly. The main role of the QFM is to assist in external rotation and adduction of the hip.
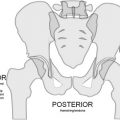
As suggested by Torriani and colleagues, ischiofemoral narrowing can be evaluated by measuring the following spaces ( Fig. 1 ):
- •
Ischiofemoral space (IFS): the narrowest distance between the lateral cortex of the ischial tuberosity and medial cortex of the lesser trochanter;
- •
Quadratus femoris space (QFS): the narrowest space for passage of the QFM delimited by the superolateral surface of the hamstring tendons and the posteromedial surface of the iliopsoas tendon or lesser trochanter.
Ischiofemoral narrowing may be positional, congenital, or acquired ( Box 1 ):
- •
Positional
- •
Congenital
- •
Acquired
- 1.
Positional factors that may affect the IFS and QFS include lower extremity internal/external rotation, adduction/abduction, and flexion/extension. Previous studies have controlled for these factors by comparing patients with suspected IFI with controls with similar leg positioning.
- 2.
Congenital ischiofemoral narrowing can be caused by a larger cross-section of the femur at the level of the lesser trochanter, a congenital posteromedial position of the femur, lower ischiopubic ramus with an angle closer to the coronal plane, prominence of the lesser trochanter, or configuration of the female pelvic bony anatomy, which shows greater width and lesser anteroposterior dimensions when compared with males ( Fig. 2 ).
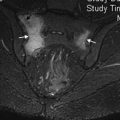
Fig. 2
56-year-old woman with lower back and right hip pain. Axial proton density-weighted MR image of right hip shows narrowed IFS and QFS with deformity of QFM ( straight arrow ).
- 3.
Acquired ischiofemoral narrowing may be seen as a result of fractures involving the lesser trochanter, valgus-producing intertrochanteric osteotomy, osteoarthritis leading to superior and medial migration of the femur in older patients, enthesopathy of the proximal hamstring insertion, or expansile bone lesions (eg, osteochondroma) ( Fig. 3 ).
Fig. 3
41-year-old man with right buttock pain for 5 months precipitated by sitting. Anteroposterior radiograph ( A ) and axial proton density-weighted MR image ( B ) show osteochondroma of lesser trochanter ( arrow in A ) leading to secondary IFS narrowing and direct compression of QFM ( arrow in B ). Lobular extension of the cartilage cap is seen anteriorly ( arrowhead in B ), abutting the distal iliopsoas muscle.
Clinical presentation
Patients with IFI present with chronic pain in the groin or buttock, usually without a precipitating injury. The pain may radiate distally to the lower extremity, because of the proximity of QFM with pressure effect on the sciatic nerve ( Fig. 4 ), and can be related to other symptoms such as snapping, crepitation, or locking.
There is no specific diagnostic clinical test for IFI, but clinicians should keep this diagnosis in mind when pain is reproduced during specific maneuvers. Pain symptoms have been described in patients with IFI in response to a wide range of hip positions, including flexion, abduction, or internal rotation, as well as extension, adduction, and external rotation ( Box 2 ).