This technical review provides a comprehensive overview of spinal tumor ablation and vertebral augmentation. These percutaneous minimally invasive procedures offer significant survival and palliative pain relief benefits for patients with pathological vertebral fractures. Vertebral augmentation, which includes vertebroplasty and kyphoplasty, involves injecting cement into fractured vertebral bodies to restore height. While vertebroplasty involves the direct injection of cement into a fractured vertebral body, kyphoplasty involves using a balloon to create a low-pressure cavity to allow for cement injection to restore the vertebral body height. Over the years, this technique has evolved into a straightforward process, though it presents certain technical challenges discussed in this article.
Introduction
Bony metastases are often a consequence of advanced metastatic cancer, with the spine being the most common site of bony metastases. , Patients with spinal metastases frequently endure severe, debilitating pain due to pathological fractures or tumor-related compression, often accompanied by neurologic deficits. Given the increasing incidence of cancer, the World Health Organization estimates that 29.4 million new cancer patients will be diagnosed by 2040, indicating a potential unmet clinical need to provide efficient, cost-effective procedures for palliative short-term pain relief to mitigate the growing burden of spinal metastases. ,
Pathologic fractures have been associated with poorer survival outcomes in patients with bony metastases. Current meta-analyses have demonstrated that vertebral augmentation (VA) may also provide an overall survival benefit. The current standard of care for localized bone pain due to metastatic disease is radiation therapy. However, there is a significant flare phenomenon and delay in achieving adequate pain relief. Additionally, 20%-30% of patients do not experience pain relief and repeated radiation therapies are cumulatively toxic and unfeasible. ,
A potential answer to this ever-growing problem can be offered by skilled interventional oncologists who are trained in spinal tumor ablations combined with vertebral augmentation. Vertebral augmentation consists of either direct injection of bone cement (PMMA), known as vertebroplasty, or with the aid of a balloon, known as kyphoplasty. Since the first vertebroplasty in 1984, there has been a rapid amount of evidence generated in favor of VA to treat cancer-related pathological fractures. Currently, VA is recommended by the NCCN and the ACR for the treatment of spinal metastases.
Not only is VA an effective palliative procedure, it can also provide meaningful survival outcomes to patients suffering from compression fractures. , As a result, it is crucial to highlight the complexities and technical challenges associated with this impactful procedure.
Clinical evaluation
VA is considered in a multidisciplinary setting with medical oncology, neurosurgery, and radiation oncology. The most common indication for performing VA is pain palliation. Despite the “gold standard” of care being palliative radiation therapy, percutaneous VA and ablation help provide immediate postprocedural pain relief as an outpatient procedure. Furthermore, the decision to proceed with VA can be influenced by other factors, such as patients who had received maximal radiation dose to prevent cumulative toxicity, a lack of patient desire to undergo radiation therapy, or patients not achieving relief on conservative therapy and analgesia. Other indications include pathologic fracture stabilization, contraindications to cumulative radiation therapy, or inadequate response to analgesia.
At our center, we usually treat up to 4 levels in a single procedure, and if more levels are to be treated, then a multi-level approach can be considered. Patients presenting with acute pain may also be referred from other specialties, such as radiation oncology, as a joint effort to treat painful bony metastases. Timing of the VA can be done either before or after radiation has been administered. VA cannot be performed simultaneously with SBRT or after simulations have been performed. Ongoing systemic therapies such as chemotherapy or immunotherapy do not play any role in deciding when to perform VA.
Indications for performing VA + ablation
- •
Pain Palliation: For acute fracture or for persistent pain despite maximized radiation therapy, contraindications to radiation therapy, or inadequate response to conservative or analgesic therapy. ,
- •
Local Tumor control: For treating oligometastatic metastases. ,
- •
Prophylactic: For preventing adjacent level fractures.
Absolute contraindications
- •
Active blood stream of spinal infection.
- •
Uncorrectable bleeding.
- •
Allergy to PMMA.
- •
Bilsky score of 1C or above.
- •
Poor systemic health or poor life expectancy of less than 30 days.
Relative contraindications
- •
Posterior wall instability.
- •
Significant spinal canal stenosis due to retropulsion of fractures or epidural tumor extension.
Preprocedural evaluation
Clinical history and examination
A detailed clinical and neurological evaluation is paramount in deciding which levels to treat. The most common patient complaint is pain. A detailed history to evaluate the inciting event, acute fractures, localized pain, and causes of pain exacerbation, such as movement and weight-bearing, can be important clinical vignettes for establishing a diagnosis. Other important points include prior treatments, such as radiation, systemic therapies, medication requirements, and the patient’s functional status.
Physical examination and history can demonstrate back pain at the fracture site, where palpation over the fractured site can replicate the pain. Neurological deficits or radiculopathy can hint towards nerve root compression and relative contraindications to the procedure. We always perform a detailed neurological assessment to establish the baseline level of function or deficit. When deciding to treat multiple levels of diffuse metastatic spinal disease, the decision to treat the most symptomatic spinal levels should be undertaken. A hemogram and coagulation test (PT/INR) should be performed to assess baseline vitals and whether there are any bleeding risks in these patients. A target INR of less than 1.5 is ideal to prevent unnecessary bleeding. All antiplatelet drugs (aspirin, clopidogrel) should be held for 7 days. Injectable low molecular-weight heparin should be discontinued in high-risk patients 12 hours before the procedure.
Preprocedural imaging
Preprocedural imaging is an absolute must in all patients. Clinical examination should be correlated with imaging findings to confirm the treated levels and fully assess landmarks to decide which levels to treat. Anatomic variants, such as additional vertebral segments, transitional lumbosacral anatomy, supernumerary ribs, and congenital anomalies, can often be found, which may lead to potential wrong treatment sites. MRI is generally the preferred route of preprocedural imaging, where STIR or T2-weighted sequences can elucidate unhealed fractures with hyperintense signals ( Fig. 1 ). MRI can help differentiate between osteoporotic and pathological fractures and may help determine other asymptomatic fractures within the same patient. When MR imaging is unavailable, a nuclear scintigraph bone scan can also provide important clues to distinguish between acute fractures (which take up 99m Tc) and healed fractures (which do not take up 99m Tc), as well as predict which lesions will respond to providing pain relief. CT can also diagnose fractures, assess fracture retropulsion, and understand the underlying patient anatomy. Posterior cortical fractures may not be ideal candidates for VA as there may be an increased risk of cement leakage for these candidates. Noting the histology and type of bony lesion, whether osteolytic or osteoblastic, is important in planning the procedure. Osteoblastic lesions may prove to be more technically challenging but should be treated regardless.

Equipment and setup
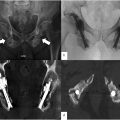
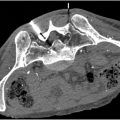
VA can be performed either under CT guidance ( Figs. 2 and 3 ) or under direct fluoroscopy ( Fig. 4 ). Both have distinct advantages and disadvantages. Fluoroscopy can be more dynamic and faster, especially with a biplane setup. CT guidance can provide a higher level of detail. Ultimately, deciding to use Fluoroscopy or CT is operator-dependent, with no significant implications on the procedural outcomes.





For spinal tumor ablation, RF is the mainstay in our practice. We use the Optablate System (Stryker Corporation, Kalamazoo, MI) ( Fig. 5 ), or the Osteocool system (Medtronic, Minneapolis, MN). The decision to forego other modalities, such as microwave ablation, cryoablation, or laser ablation, is due to the familiarity and large evidence base supporting the use of RF for spinal ablation. , Both systems utilize a bipolar RFA setup with active tip cooling and real-time impedance feedback to minimize charring and damage to the surrounding vital structures. Similarly, both companies offer vertebral augmentation kits to facilitate seamless ablation and augmentation.

Procedural steps
General vs. moderate sedation: The choice depends on the operator and required setup, and special considerations are required for local/moderate sedation to ensure comfort to the patient. General anesthesia is particularly indicated for patients with a high risk of airway complications due to pone positioning or with preprocedural narcotic requirements (which is important in cases who are nonresponsive to maximal analgesics). Other indications may entail patients with difficult access, several co-morbidities, or overall uncooperative patients. Moderate sedation can be selected for patients with 1 to 2 affected levels or for patients who are at a high risk of neurologic complications. It is beneficial to have moderate sedation for cases where conscious neuromonitoring and feedback for complex cases.
After obtaining consent for the procedure, a single dose of 1g IV Cefazolin is given 1 hour before. The patient is placed in the prone position, and the back is prepped with povidone-iodine or chlorohexidine scrub solution. A strict aseptic technique is maintained, with continuous monitoring of pulse rate, oxygen saturation, and blood pressure by both the operator and certified anesthesiology should be adhered to. After conducting the time-out, the vertebral level is identified as correlated to the preprocedural imaging. Always image the entire spine and count to the affected level to prevent any wrong site from being treated due to anatomical variations. Once the affected level is identified, liberal amounts of lidocaine (1% lidocaine or 025% bupivacaine) with a 25G needle (especially for moderate sedation) are injected into the periosteum over the pedicles of the affected level. A small scalpel is used to access the 10G or 11G diamond-tipped bone access needles. An angle of 4-12 degrees is optimal. For cases with needle drift, beveled needles can be used to realign the needle back to the initial target. Begin initially with the middle of the pedicle and navigate with both AP and lateral imaging to ensure that the needle is optimally advanced. A “down the barrel view” can be performed if using fluoroscopy ( Fig. 4 A). An orthopedic mallet can advance the bone needle anteriorly until the posterior 1/3rd of the vertebral body is reached and confirmed with repeat imaging. The majority of cases will require bilateral transpedicular approaches ( Table 1 ). For cases under moderate sedation, wrapping the mallet with a towel while hammering can reduce the audio trauma to the patient and make the process more comfortable. After access is achieved, the inner stylet of the needle is removed. At this point in time, histological sampling can be performed as well.