Treatment Strategy
Primary radiotherapy is preferred for most T1 tumors. The preferred larynx-preserving therapy for T2 tumors depends on the disease and patient characteristics. For lesions that are nonbulky and exophytic, therapy consists of hyperfractionated or concomitant boost radiotherapy.
For T2 lesions, bulky or infiltrating:
Good pulmonary function and general condition: supraglottic laryngectomy or laser resection with or without postoperative radiotherapy.
Medically unfit or technically not suitable for supraglottic laryngectomy: if medically fit for chemotherapy, radiation with concurrent cisplatin or induction chemotherapy (docetaxel, cisplatin, and fluorouracil) followed by radiation; alternatively, hyperfractionated or concomitant boost radiotherapy.
Primary Radiotherapy
Target Volume
Initial target volume:
For boost volume: primary tumor and, when present, involved nodes with 1- to 2-cm margins.
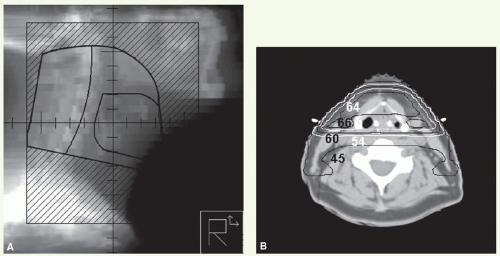
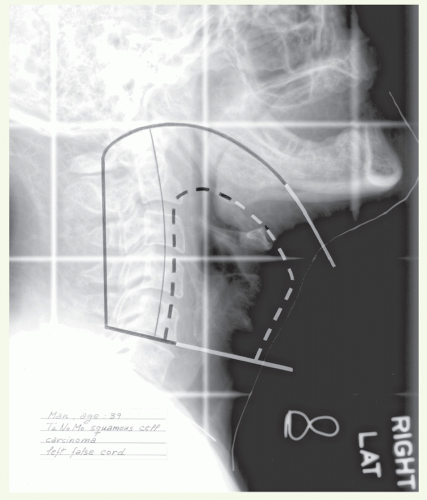
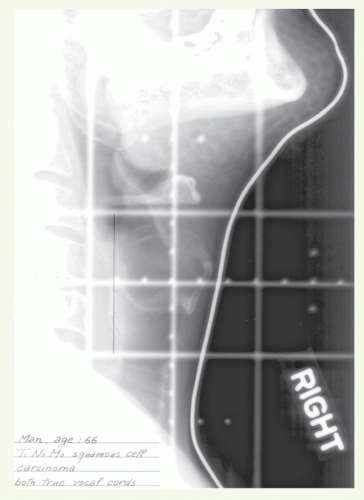
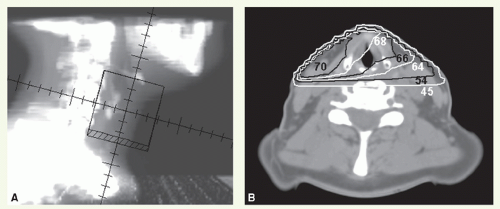
Setup and Field Arrangement for Conventional Radiotherapy Technique
The patient is immobilized in a supine position with a thermoplastic mask. Marking of shoulders and, when present, involved nodes facilitates portal design. Lateral parallel-opposed photon fields are used to treat the primary tumor and upper neck nodes.
Superior border: approximately 2 cm above the angle of mandible when N0 or approximately 1 cm above the tip of mastoid process when N+.
Anterior border: falloff anteriorly; when there is extension into the oropharynx, a generous part of the base of tongue is encompassed in the field.
Posterior border: behind the spinous processes or more posteriorly in the presence of large nodal mass.
Inferior border: depends on the disease extent—middle or bottom of cricoid cartilage for tumors of the epiglottis or false cord; upper trachea when there is subglottic extension (at least 2 cm below inferior tumor extent).
An anterior portal is used to treat the lower neck. It may be necessary to use anterior and inferior tilts for patients with a short neck. In this case, the supraclavicular fossa is included in the primary portal.
For boost volume, the lateral fields are reduced to 1- to 2-cm margins around the primary tumor and involved nodes. Nodes overlying the spinal cord can usually receive boost dose through oblique-lateral primary boost portals and those in the lower neck through an appositional electron portal or glancing photon fields.
Dose
For T1 N0 tumors: 50 Gy in 25 fractions to the initial target volume followed by 16 Gy in 8 fractions to the primary tumor. For T1 N1 tumors, an addition 4 Gy in two fractions can be delivered to the neck node with either an appositional electron beam or glancing photon beams.
For T2 N0 or T2 N1 tumors: hyperfractionated or concomitant boost regimen. Hyperfractionation delivers 55.2 Gy in 46 fractions to the initial target volume and then 21.6 Gy in 18 fractions (1.2-Gy fractions, twice daily, 6-h interval); the spinal cord dose is limited to 44.4 to 45.6 Gy or less, and uninvolved posterior cervical nodes are supplemented with 2 Gy daily to approximately 55 Gy. Concomitant boost delivers 1.8-Gy fractions to 54 Gy in 30 fractions to the initial target volume and 1.5-Gy fractions to 15 to 18 Gy given as second daily fractions during the last 2 to 2.5 weeks; the spinal cord dose is limited to 45 Gy or less.
Positive nodes receive doses appropriate for the size and the fractionation schedule used, for example, includes 66 to 70 Gy in 2-Gy fractions, 69 to 72 Gy with concomitant boost, or 74.4 to 79.2 Gy with hyperfractionation. The dose to uninvolved lower neck nodes is 50 Gy in 25 fractions (treated once a day).
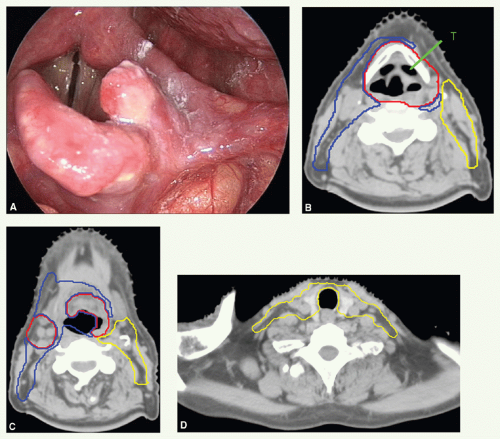
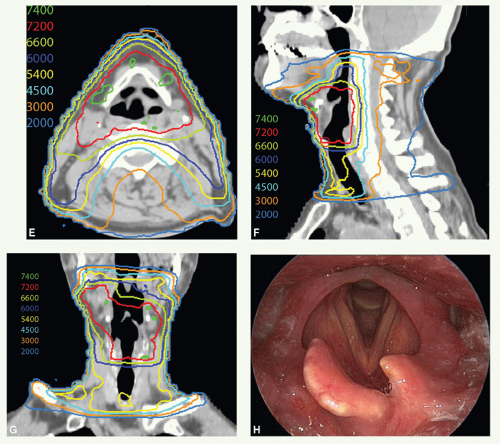
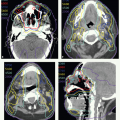
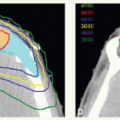
Intensity-Modulated Radiation Therapy Planning
Most patients are now treated with IMRT to spare parotid function
(see Case Study 9-3). The primary tumor is treated with a minimum of 1-cm margin, though, due to laryngeal motion, it is prudent to encompass the majority of the larynx in the high dose target volume (CTV
HD or CTV1). Involved node(s) with 1-cm margin are also encompassed in CTV
HD. The neck compartments outside CTV
HD with a 2-cm (cranial-caudal) margin are delineated as CTV
ID (CTV2). The remaining nodal levels (II, III, IV, and V) are contoured as CTV
ED (CTV3). Level Ib is included in CTV
ED on the side(s) of lymphadenopathy.
For patients with T2 tumors treated with IMRT, we have used the concomitant boost schedule, which requires two separate plans. The first plan delivers 57 Gy in 30 fractions to CTVHD and CTVID and 54 Gy to CTVED, and the second plan is for 18 Gy in 10 fractions to CTVHD. The fractionation regimen is similar to non-IMRT radiotherapy. If the preference is to deliver treatment with one plan, we prescribe 70 Gy to CTVHD, 60 to 63 Gy to CTVID, and 56 to 57 Gy to CTVED to be delivered in 35 fractions over 6 weeks, by administering 6 fractions a week for 5 weeks with a 6-hour interfraction interval on the day when 2 fractions are delivered.