GROSS ANATOMY
Overview
- •
Liver: Largest gland and largest internal organ (average weight: 1,500 g)
- ○
Functions
- –
Processes all nutrients (except fats) absorbed from gastrointestinal (GI) tract; conveyed via portal vein
- –
Stores glycogen, secretes bile
- –
- ○
Relations
- –
Anterior and superior surfaces smooth and convex
- –
Posterior and inferior surfaces indented by colon, stomach, right kidney, duodenum, inferior vena cava (IVC), and gallbladder
- –
- ○
Covered by peritoneum except along gallbladder fossa, porta hepatis, and bare area
- –
Bare area : Nonperitoneal posterior superior surface where liver abuts diaphragm
- –
Porta hepatis : Portal vein, hepatic artery, and bile duct located within hepatoduodenal ligament
- –
- ○
Falciform ligament
- –
Extends from liver to anterior abdominal wall
- –
Separates right and left subphrenic peritoneal recesses (between liver and diaphragm)
- –
Marks plane separating medial and lateral segments of left hepatic lobe
- –
Carries round ligament (ligamentum teres), fibrous remnant of umbilical vein
- –
- ○
Ligamentum venosum
- –
Remnant of ductus venosus
- –
Separates caudate from left hepatic lobe
- –
- ○
- •
Vascular anatomy (unique dual afferent blood supply)
- ○
Portal vein
- –
Carries nutrients from gut and hepatotrophic hormones from pancreas to liver along with oxygen
- □
Contains 40% more oxygen than systemic venous blood
- □
- –
75-80% of blood supply to liver
- –
- ○
Hepatic artery
- –
Supplies 20-25% of blood
- –
Liver less dependent than biliary tree on hepatic arterial blood supply
- –
Usually arises from celiac artery
- –
Variations common, including arteries arising from superior mesenteric artery
- –
- ○
Hepatic veins
- –
Usually 3 (right, middle, and left)
- –
Many variations and accessory veins
- –
Collect blood from liver and return it to IVC
- –
Confluence of hepatic veins just below diaphragm and entrance of IVC into right atrium
- –
- ○
Portal triad
- –
At all levels of size and subdivision, branches of hepatic artery, portal vein, and bile ducts travel together
- –
Blood flows into hepatic sinusoids from interlobular branches of hepatic artery and portal vein → hepatocytes, which detoxify blood and produce bile
- □
Blood collects into central veins → hepatic veins
- □
Bile collects into ducts → stored in gallbladder and excreted into duodenum
- □
- –
- ○
- •
Segmental anatomy
- ○
8 hepatic segments
- –
Each receives secondary or tertiary branch of hepatic artery and portal vein
- –
Each drained by its own bile duct (intrahepatic) and hepatic vein branch
- –
- ○
Caudate lobe = segment 1
- –
Has independent portal triads and hepatic venous drainage to IVC
- –
- ○
Left lobe
- –
Lateral superior = segment 2
- –
Lateral inferior = segment 3
- –
Medial superior = segment 4a
- –
Medial inferior = segment 4b
- –
- ○
Right lobe
- –
Anterior inferior = segment 5
- –
Posterior inferior = segment 6
- –
Posterior superior = segment 7
- –
Anterior superior = segment 8
- –
- ○
IMAGING ANATOMY
Internal Contents
- •
Capsule
- ○
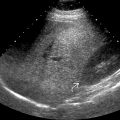
Reflective Glisson capsule making borders of liver well defined
- ○
- •
Left lobe
- ○
Contains segments 2, 3, 4a, and 4b
- ○
Longitudinal scan
- –
Triangular in shape
- –
Rounded upper surface
- –
Sharp inferior border
- –
- ○
Transverse scan
- –
Wedge-shaped tapering to left
- –
- ○
Liver parenchyma echoes are midgray with uniform, sponge-like pattern interrupted by vessels
- ○
- •
Right lobe
- ○
Contains segments 5, 6, 7, and 8
- ○
Liver parenchymal echoes similar to left lobe
- ○
Sections of right lobe show same basic shape, though right lobe usually larger than left
- ○
- •
Caudate lobe
- ○
Longitudinal scan
- –
Almond-shaped structure posterior to left lobe
- –
- ○
Transverse scan
- –
Seen as extension of right lobe
- –
- ○
- •
Portal veins
- ○
Have thicker reflective walls than hepatic veins; portal veins have fibromuscular walls
- ○
Wall reflectivity also depends on angle of interrogation; portal veins cut at more oblique angle, may have less apparent wall
- ○
Can be traced back toward porta hepatis
- ○
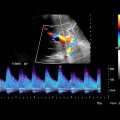
Normal portal flow is hepatopetal on color Doppler; absent or reversal of flow may be seen in portal hypertension
- ○
Normal velocity: 13-55 cm/s
- ○
Normal diameter: < 13 mm
- ○
Portal waveform has undulating appearance due to variations with cardiac activity and respiration
- ○
Branches run in transverse plane
- ○
Hepatic portal vein anatomy is variable
- ○
- •
Hepatic veins
- ○
Appear as echolucent tubular structures within liver parenchyma with no reflective wall: Large sinusoids with thin or absent wall
- ○
Branches enlarge and can be traced toward IVC
- ○
Flow pattern has triphasic waveform
- –
Resulting from transmission of right atrial pulsations into veins
- □
A wave: Atrial contraction
- □
S wave: Systole (tricuspid valve moves toward apex)
- □
D wave: Diastole
- □
- –
- ○
Right hepatic vein
- –
Runs in coronal plane between anterior and posterior segments of right hepatic lobe
- –
- ○
Middle hepatic vein
- –
Lies in sagittal or parasagittal plane between right and left hepatic lobe
- –
- ○
Left hepatic vein
- –
Runs between medial and lateral segments of left hepatic lobe
- –
Frequently duplicated
- –
- ○
1 of 3 major branches of hepatic veins may be absent
- –
Absent right hepatic vein: ~ 6%
- –
Less commonly middle and left hepatic vein
- –
- ○
- •
Hepatic artery
- ○
Flow pattern has low-resistance characteristics with large amount of continuous forward flow throughout diastole
- –
Normal velocity of proper hepatic artery: 40-80 cm/s
- –
Resistive index ranges 0.5-0.8, increases after meal
- –
- ○
Common hepatic artery usually arises from celiac axis
- ○
Classic configuration: 72%
- –
Celiac axis → common hepatic artery → gastroduodenal artery and proper hepatic artery → latter gives rise to right and left hepatic artery
- –
- ○
Variations from classic configuration
- –
Common hepatic artery arising from superior mesenteric artery (replaced hepatic artery): 4%
- –
Right hepatic artery arising from superior mesenteric artery (replaced right hepatic artery): 11%
- –
Left hepatic artery arising from left gastric artery (replaced left hepatic artery): 10%
- –
- ○
- •
Bile ducts
- ○
Normal peripheral intrahepatic bile ducts too small to be demonstrated
- ○
Normal right and left hepatic ducts measuring few millimeters usually visible
- ○
Normal common duct
- –
Most visible in its proximal portion just caudal to porta hepatis: < 5 mm
- –
Distal common duct should typically measure < 6-7 mm
- –
In elderly, generalized loss of tissue elasticity with advancing age leads to increase in bile duct diameter: < 8 mm (somewhat controversial)
- –
- ○
ANATOMY IMAGING ISSUES
Questions
- •
Designating and remembering hepatic segments
- ○
Portal triads are intrasegmental, hepatic veins are intersegmental
- ○
Separating right from left lobe
- –
Plane extending vertically through gallbladder fossa and middle hepatic vein
- –
- ○
Separating right anterior from posterior segments
- –
Vertical plane through right hepatic vein
- –
- ○
Separating left lateral from medial segments
- –
Plane of falciform ligament
- –
- ○
Separating superior from inferior segments
- –
Plane of main right and left portal veins
- –
- ○
Segments numbered in clockwise order, as if looking at anterior surface of liver
- ○
Imaging Recommendations
- •
Transducer
- ○
2.5- to 6.0-MHz curvilinear or vector transducer generally most suitable
- ○
Higher frequency linear transducer (i.e., 7-12 MHz) useful for evaluation of liver capsule and superficial portions of liver
- ○
- •
Left lobe
- ○
Subcostal window with full inspiration generally most suitable
- ○
- •
Right lobe
- ○
Subcostal window
- –
Cranial and rightward angulation useful for visualization of right lobe below dome of hemidiaphragm
- –
Can sometimes be obscured by bowel gas
- –
- ○
Intercostal window
- –
Usually gives better resolution for parenchyma without influence from bowel gas
- –
Right lobe just below hemidiaphragm may not be visible due to obscuration from lung bases
- –
Important to tilt transducer parallel to intercostal space to minimize shadowing from ribs
- –
- ○
Imaging Pitfalls
- •
Because of variations of vascular and biliary branching within liver (common), frequently impossible to designate precise boundaries between hepatic segments on imaging studies
CLINICAL IMPLICATIONS
Clinical Importance
- •
Liver ultrasound often 1st-line imaging modality in evaluation for elevated liver enzymes
- ○
Diffuse liver disease, such as hepatic steatosis, cirrhosis, hepatomegaly, hepatitis, and biliary ductal dilatation, well visualized on ultrasound
- ○
Documentation of patency of portal vein, hepatic vein waveforms, and hepatic arterial velocities helpful in evaluation for etiologies of elevated liver function tests
- ○
- •
Liver metastases common
- ○
Primary carcinomas of colon, pancreas, and stomach commonly metastasize to liver
- –
Portal venous drainage usually results in liver being initial site of metastatic spread from these tumors
- –
- ○
Metastases from other non-GI primaries (breast, lung, etc.) commonly spread to liver hematogenously
- ○
- •
Primary hepatocellular carcinoma
- ○
Common worldwide
- –
Risk factors include cirrhosis of any etiology and chronic viral hepatitis B in certain populations
- –
Chronic hepatitis C with stage 3 fibrosis and nonalcoholic steatohepatitis may also have increased risk of hepatocellular carcinoma
- –
Ultrasound commonly used for screening and surveillance in patients at risk for development of hepatocellular carcinoma typically at 6-month intervals
- –
- ○
HEPATIC VISCERAL SURFACE