Abstract
Objective
Ultrasound stimulation of internal organs and peripheral nerves has demonstrated promising potential in regulating blood glucose metabolism. This study aims to assess the effectiveness of low-intensity pulsed ultrasound stimulation (LIPUS) on intestine in improving insulin resistance with type 2 diabetes mellitus (T2DM).
Methods
C57BL/6J mice, both normal and T2DM, were randomly divided into three groups: Control, T2D-sham, and T2D-LIPUS. The T2D-LIPUS group received LIPUS stimulation in the intestine. The parameters were as follows: 1 MHz frequency, 1.0 kHz pulse repetition frequency (PRF), 20% duty cycle, 100 mW/cm² intensity spatial average temporal average (I SATA ), for 20 minutes per session, five days per week, over four weeks.
Results
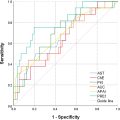
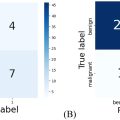
Blood glucose analysis indicated that mice in the T2D-LIPUS group displayed significantly lower area under the curve (AUC) of glucose tolerance tests (GTT) and insulin tolerance tests (ITT) ( p < 0.001), HOMA-IR ( p < 0.001), and fasting serum insulin levels ( p < 0.01) compared to the T2D-sham group. LIPUS treatment effectively lowered serum levels of IL-1β ( p < 0.001) and TNF-α ( p < 0.01) along with mRNA expression levels of IL-1β ( p < 0.01) and IL-18 ( p < 0.001) in the intestines of T2DM mice. Additionally, Western blot analysis revealed a reduction in the protein levels of NLRP3, caspase-1, and GSDMD-N in the intestinal tissues of mice treated with LIPUS.
Conclusion
These findings suggest that LIPUS can reduce inflammation and cellular apoptosis, while improving insulin resistance by inhibiting the NLRP3/Caspase-1/GSDMD signaling pathway. This research introduces a novel, non-pharmacological approach for managing T2DM.
Introduction
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disease characterized by high blood glucose, insulin resistance, and impaired β-cell function [ ]. It is closely associated with genetic predisposition, suboptimal dietary habits, and lifestyle factors [ ]. Complications arising from persistent hyperglycemia, such as microvascular issues including diabetic nephropathy [ , ], retinopathy [ ], and neuropathy [ ], as well as macrovascular conditions like coronary artery disease, heart attack, stroke, and diabetic foot ulcers [ ], are significant contributors to diabetes-related mortality. The increasing prevalence of diabetes has thus become a pressing global public health concern [ ]. However, fully understanding the complex pathophysiological mechanisms underlying T2DM remains a challenge, which in turn complicates efforts toward its effective treatment.
The intestine plays a critical role in blood glucose metabolism and is essential in maintaining glucose homeostasis. In response to nutrient intake, enteroendocrine cells release incretin hormones, which subsequently stimulate insulin secretion from the pancreas [ ]. During glucose tolerance tests, it has been observed that a substantial portion (up to 70%) of insulin release, which controls blood glucose levels, is attributed to gut-derived hormone stimulation. These hormones include Glucose-Dependent Insulinotropic Peptide (GIP) and Glucagon-Like Peptide-1 (GLP-1), produced by enteroendocrine K-cells and L-cells, respectively [ ]. However, individuals with T2DM often show impaired or reduced incretin function. Consequently, various new anti-diabetic drugs have been designed specifically to target incretin regulation [ ]. Beyond pharmacological approaches, bariatric surgery has proven effective in improving diabetes outcomes [ ]. This effect is achieved through mechanisms such as restricting food intake, accelerating chyme transit to the distal small intestine, and stimulating the release of gastrointestinal hormones—all processes closely tied to intestinal function. Additionally, substantial research has established a strong link between gut microbiota and blood glucose regulation [ ]. Despite their potential, glucose-lowering drugs often pose drawbacks such as toxicity and risk of dependency, which may limit their long-term efficacy in diabetes management. Similarly, although surgical and gut microbiota-targeted interventions are promising, they also have limitations in treatment outcomes. With the diabetic population rising at a rapid rate, there is an urgent need for innovative therapeutic approaches.
Low-intensity pulsed ultrasound (LIPUS) is a specific type of focused ultrasound that offers distinct advantages across various applications, including promoting the healing of bone fractures, reducing inflammation in soft tissue regeneration, and influencing nerve activity [ ]. The effectiveness of ultrasonic therapy in managing diabetes has been supported by numerous studies. In vitro research has shown that pancreatic beta cells increase insulin secretion following exposure to continuous, non-focused ultrasound at a frequency of 0.8 MHz for 5 minutes with an ISPTA of 1 W/cm 2 [ ]. Additionally, in vivo studies in a mouse model demonstrated a significant rise in blood insulin levels when the pancreas was subjected to the same intensity and duration of ultrasound at 1 MHz [ ]. Saab et al. further investigated these effects using a 2D model of the abdominal region in adolescents, exploring the impact of ultrasound on the pancreas and surrounding tissues. Their experiments with various combinations of angle, ultrasound intensity, and duration revealed that applying ultrasound (f = 1 MHz, I = 5 W/cm 2 ) directly from the anterior abdomen produced optimal pressure on the pancreas, yielding therapeutic effects for T2DM [ ]. Peripheral nerve modulation techniques for diabetes have also shown potential in reducing insulin resistance. In lipopolysaccharide-induced diabetic rats, pulsed focused ultrasound (pFUS) stimulation of the hepatic portal, pancreas, and intestine regions was found to improve glucose tolerance and utilization to varying degrees. Further studies have indicated that cytokine production in the pancreas can be influenced by the intensity of sound waves [ ].
Using ultrasound to regulate glucose levels by stimulating internal organs and adjacent nerves has shown potential in diabetes management. The intestine, a key organ in glucose metabolism, remains relatively unexplored in terms of symptom improvement through ultrasound stimulation. Therefore, we selected the intestine as the target for stimulation to evaluate the efficacy and mechanisms of ultrasound therapy in managing T2DM. Specifically, LIPUS was applied to the abdominal intestinal area of mice with STZ-induced T2DM. Therapeutic outcomes were assessed using glucose tolerance tests (GTT), insulin tolerance tests (ITT), serum analysis, and hematoxylin-eosin (H&E) staining. Additionally, this study examined the underlying mechanisms of ultrasound therapy in diabetes management through qRT-PCR and Western blot analysis.
Materials and methods
Animal model and experimental procedures
The Animal Ethics Committee of Fudan University approved the experimental protocol, which adhered to the guidelines of the National Institutes of Health’s Guide for the Care and Use of Laboratory Animals (Protocol number: IDM2021020). Forty male mice, aged five weeks and weighing between 20g And 30g, were used in this study, supplied by GemPharmatech Co., Ltd. (Nanjing, China). The mice were housed five per cage in controlled conditions, with a 12-hour light-dark cycle and unrestricted access to food and water. The environmental parameters were set at a temperature of 23 ± 1°C and a relative humidity of 60% ± 5%. A two-week acclimation period was provided before the start of experimental procedures. For clarity, the experimental timeline is depicted in Figure 1 a. The mice were divided into two groups and fed either a standard diet (n = 10) or a high-fat diet (HFD, n = 30) ad libitum, with 60% of calories derived from fat (D12492). After 4 weeks on the HFD, the mice received intraperitoneal injections of streptozotocin (STZ, Sigma, St. Louis, MO, USA), dissolved in 0.1 mol/L citrate buffer (pH 4.5), at a dose of 40 mg/kg per day for three consecutive days. On the ninth day after completing STZ injections, the mice were fasted for eight hours, and fasting blood glucose levels were measured. Mice with fasting blood glucose levels ≥8.3 mmol/L were classified as having T2DM for the study. The experimental groups included the control group (Control, normal mice, n = 8) fed a standard diet, the sham operation group (T2D-sham, type 2 diabetic mice, n = 8), and the LIPUS treatment group (T2D-LIPUS, type 2 diabetic mice, n = 8), with all diabetic mice in the latter two groups fed HFD. The T2D-LIPUS group received continuous ultrasound treatment for 4 weeks. The Control and T2D-sham groups underwent the same positioning, experimental setup, and procedures as the LIPUS group, with the only difference being that the LIPUS device was deactivated during experiments, thus emitting no ultrasound waves.

At the end of the treatment period, the mice were euthanized for tissue collection. Blood samples were taken from the retro-orbital plexus, and the liver and epididymal fat were excised and weighed. Tissue samples from the small intestine and pancreas were used for qRT-PCR and Western blot analysis. Additionally, a portion of pancreas tissue from each group was selected for morphological examination.
LIPUS treatment
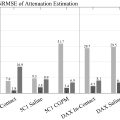
The LIPUS device, an ultrasound treatment tool, was developed in-house by the Department of Biomedical Engineering, Fudan University (Shanghai, China) ( Fig. 1 b). The device operated at 1 MHz, with a pulse repetition frequency (PRF) of 1.0 kHz, a duty cycle of 20%, and an intensity spatial average temporal average (I SATA ) of 100 mW/cm 2 .
Before LIPUS treatment, ultrasonic propagation sound field was measured by hydrophone (NH0200, Precision acoustics, UK) ( Fig. S1 ) and the acoustic power of the transducer was measured by an acoustic power meter (UPM-DT-1000 PA, Ohmic Instruments, MO, USA). I SATA of the treatment ultrasound was calculated by dividing the emission area of the planar probe. To ensure consistent treatment intensity, the probe was calibrated at the end of each week during LIPUS treatment.
During treatment, mice were placed in a horizontal supine position and kept under continuous isoflurane inhalation anesthesia. The treatment site was located over the abdominal area (above the intestine) ( Fig. 1 c). An ultrasound coupling gel was applied between the skin and a planar circular transducer (Suzhou Sound Source Transducer Co., Ltd., Suzhou, China), with a diameter of 20 mm. Mice in the T2D-LIPUS group received daily ultrasound treatment for 20 minutes, five days per week, over four weeks. Mice in the control and T2D-sham groups underwent the same procedure, except that the ultrasound device remained inactive.
Glucose and insulin tolerance test
Following a 16-hour fast, mice underwent the glucose tolerance test (GTT) with an intraperitoneal injection of glucose at a dose of 1.0 g/kg body weight. For the insulin tolerance test (ITT), mice were fasted for six hours before receiving an intraperitoneal injection of insulin at 0.5 U/kg body weight. Blood samples were taken from the tail vein at 0, 30, 60, 90, and 120 minutes before and after treatment, and blood glucose levels were measured using a glucometer (OneTouch Ultra, Johnson & Johnson, USA).
Serum biochemistry analysis
Mouse blood samples were collected and centrifuged at 4°C and 3500 rpm for 15 minutes to obtain serum. Serum insulin levels were analyzed by ELISA (90080 Ultra Sensitive, Donas Grove, IL, USA). Serum levels of tumor necrosis factor-α (TNF-α) and interleukin-1β (IL-1β) were measured by ELISA (MEC1003 and MEC1010, Derry Road East, Ontario, Canada). Serum triglycerides (TG) and total cholesterol (T-cho) were assessed as per the manufacturer’s instructions (A110-1-1, A111-1-1, Nanjing Jiancheng Bioengineering Institute, Nanjing, China).
H&E staining
Following treatment, pancreatic samples from the three groups of mice were collected, fixed in 4% paraformaldehyde, and embedded in paraffin. Thin sections of pancreas tissue were stained with hematoxylin and eosin (H&E) and examined under a microscope.
Quantitative real-time PCR
The procedure involved lysing the intestinal tissue homogenate to release its contents, extracting total RNA with Trizol reagent, and then synthesizing complementary DNA through reverse transcription. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) served as the internal reference for the SYBR qPCR Mix using the QuantStudio 5 Real-Time PCR System from Thermo Fisher Scientific. Quantitative RT-PCR was performed in triplicate, and relative quantification was determined using the 2 −ΔΔCT method. Primer sequences are listed in Table 1 .
| Forward primer (5′ -> 3′) | Reverse primer (5′ -> 3′) | |
|---|---|---|
| IL-1β | TAC ATC AGC ACC TCA CAA GC | AGA AAC AGT CCA GCC CAT ACT |
| IL-18 | AAT GGA GAC CTG GAA TCA GAC | TTG TCA ACG AAG AGA ACT TGG |
| NLRP3 | GAC TGC GAG AGA TTC TAC AGC | CCT CCT CTT CCA GCA AAT AGT |
| GSDMD | CTG TAT GCT GAG GTG AAG GCT | GGG CTG GTC CTG TAA AAT CTT |
Western blot
For the Western blot assay, total proteins were extracted from cells using RIPA buffer. The samples from intestinal tissue were loaded onto 8% SurePAGE gels and separated by SDS-PAGE, then transferred electrophoretically to PVDF membranes. The PVDF membrane was blocked with a 5% skimmed milk solution for 2 hours, followed by an overnight incubation with a primary antibody. After three washes with TBST, the membrane was incubated for 2 hours at room temperature with a secondary antibody from Zen Bioscience. The membrane was then washed with TBST for 10 minutes, repeated three times. ECL luminescent solution was applied to the membrane, which was subsequently exposed in a chemiluminescence instrument. Antibodies and their respective dilutions are detailed in Table 2 .
| Manufacturer’s brand | Dilution ratio | |
|---|---|---|
| Anti-beta Actin antibody | BioTNT, A20120A0702 | 1:1000 |
| Anti-NLRP3 antibody [EPR20425] | Abcam, ab210491 | 1:1000 |
| Caspase 1/p20/p10 Polyclonal antibody | Proteintech, 22915-1-AP | 1:1000 |
| Anti-GSDMD antibody [EPR20859] | Abcam, ab219800 | 1:1000 |
| Peroxidase AffiniPure Goat Anti-Rabbit IgG (H+L) | Jackson, 111-035-003 | 1:20000 |
Statistical analysis
All data were presented as Mean ± Standard Error of the Mean (SEM), and statistical analyses were performed using GraphPad Prism software (Version 8.2.1, San Diego, USA). Statistical differences among groups were assessed using one-way or two-way analysis of variance (ANOVA). The effectiveness of ultrasound stimulation in alleviating symptoms of type 2 diabetes was further evaluated with Scheffe’s method as a post hoc test. A p value < 0.05 was considered statistically significant in this study. Significance levels in the text are indicated as *P, **P, and ***P for p values less than 0.05, 0.01, and 0.001, respectively.
Results
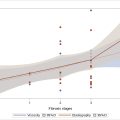
LIPUS had little impact on body weight or food intake
No significant differences in food intake were observed between the T2D-sham and T2D-LIPUS groups during the experiment. However, the control group, consisting of normal mice on a standard diet, exhibited a lower overall energy intake compared to the other two groups of mice ( Fig. 2 a). Throughout the study, the T2D-sham group maintained a higher body weight compared to both the Control and T2D-LIPUS groups. However, there were minimal changes in body weight within the Control, T2D-sham, and T2D-LIPUS groups over the feeding period ( Fig. 2 b). Further comparison of liver and epididymal fat weights revealed no significant differences in liver weight across the groups. However, the epididymal fat weight in the T2D-sham and T2D-LIPUS groups was higher than in the Control group, with the T2D-LIPUS group showing a slight reduction in epididymal fat weight compared to the T2D-sham group ( Fig. 2 c). Serum TG and TC levels were elevated in the T2D-sham group relative to the Control and T2D-LIPUS groups ( Fig. 2 d). In contrast, the T2D-LIPUS group showed a reduction in serum TG and TC levels compared to the T2D-sham group. These findings suggest that LIPUS stimulation of the intestine has limited effect on body weight and dietary intake.