KEY FACTS
Terminology
- •
Placenta previa (PP) : Placenta covers cervix internal os (IO)
- •
Low-lying placenta (LLP) : Placenta edge < 2 cm from IO
- •
Normal: Placenta edge 2 cm or more from IO
- •
Avoid “marginal” or “partial” PP (deemed confusing)
Imaging
- •
Placental tissue near cervix is hallmark finding
- ○
Sagittal view is best
- ○
- •
Transvaginal US (TVUS) is essential for diagnosis
- ○
Best way to evaluate lower uterine segment (LUS)
- ○
Measure distance between placental edge and IO
- ○
Marginal placental vessels count as placenta
- ○
- •
Important associations
- ○
Morbidly adherent placenta (placenta accreta spectrum)
- –
↑ risk if prior cesarean section (C-section)
- –
Greater risk if multiple prior C-sections
- –
- ○
Vasa previa: Fetal vessels cross IO
- ○
Top Differential Diagnoses
- •
Overdistended maternal bladder: Pushes front and back of uterus together; mimics long cervix and low placenta
- •
Focal myometrial contraction: Shortens uterus, “pulls” placenta low
- •
Placental abruption: Isoechoic blood clot mimics placenta
Clinical Issues
- •
LLP or PP is seen in 2% of all midgestation studies
- •
> 90% will resolve: Follow-up at 32 and maybe 36 weeks
- •
C-section for PP, LLPs might deliver vaginally
Scanning Tips
- •
Scan whole uterus before determining placenta location
- •
TVUS if any placenta seen in LUS
- •
Use color Doppler: Find cord insertion, rule out vasa previa
- •
Move baby head out of pelvis
- ○
Put bed in Trendelenburg (head lower than feet)
- ○
2nd person in room to push baby head up
- ○
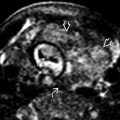
 is several centimeters over the internal cervical os
is several centimeters over the internal cervical os  . It is not surprising that this case of asymptomatic placenta previa (PP) did not resolve with advancing pregnancy.
. It is not surprising that this case of asymptomatic placenta previa (PP) did not resolve with advancing pregnancy.
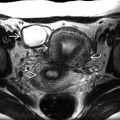
 close to, but not covering, the cervical os
close to, but not covering, the cervical os  . There is a 90% chance this will resolve with advancing pregnancy. Follow-up at 32 weeks was recommended.
. There is a 90% chance this will resolve with advancing pregnancy. Follow-up at 32 weeks was recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree