Magnetic resonance defecography (MRD) is a recommended study in the evaluation of patients with symptoms of obstructed defecation. MRD is unique in its ability to diagnose structural and functional abnormalities of the pelvic floor and provides detailed anatomic assessment to guide management. This article reviews MRD technique and limitations, normal anatomy, functional interpretation, and common pathology seen in patients with obstructed defecation and other pelvic floor disorders.
Key points
- •
MRD can aid in the diagnosis of structural and functional causes of obstructed defecation.
- •
Evacuation of rectal gel is critical to MRD accuracy.
- •
MRD can help treatment planning in patients with obstructed defecation.
| AR | anterior rectocele |
| ARA | anorectal angle |
| DPS | descending perineum syndrome |
| EAS | external anal sphincter |
| FD | fluoroscopic defecography |
| IAS | internal anal sphincter |
| LP | levator plate |
| MRD | magnetic resonance defecography |
| MRI | magnetic resonance imaging |
| OD | obstructed defecation |
| PE | physical examination |
| PCL | pubococcygeal line |
| (POP-Q) | Pelvic Organ Prolapse Quantification system |
| TW2 | T2 weighted |
Introduction
Pelvic floor disorders affect millions of Americans each year and can result in significant impairment in quality of life. These disorders are often multifactorial, and patients present with varied urinary, sexual, and defecatory complaints. Symptoms of obstructed defecation (OD) include constipation, a sense of incomplete evacuation, rectal pain, excessive straining, and the need for digital assistance (splinting) during defecation. OD has structural causes and functional causes; one or more of these causes may coexist in the same patient and require different treatment approaches. Magnetic resonance defecography (MRD) has gained popularity in the evaluation of patients with pelvic floor disorders and is now recommended in the assessment of OD. MRD is unique in its ability to diagnose structural and functional causes of OD with high soft-tissue resolution and without ionizing radiation. Additionally, MRD can identify coexistent anterior and middle compartment abnormalities that may need to be addressed during treatment planning. This article reviews MRD technique, limitations, normal anatomy, functional interpretation, and commonly seen pelvic floor pathology in patients with OD.
Imaging technique and normal anatomy
Magnetic Resonance Defecography Protocol
MRD is a noncontrast pelvic MRI that includes static sequences for structural evaluation and dynamic sequences for functional assessment of the pelvic floor. The examination takes approximately 30 minutes. Patients can be imaged in a closed-bore 1.5 T or 3.0 T magnet; upright open-bore magnets were initially preferred for their physiologic positioning but are rarely available in clinical practice. In a closed-bore magnet, patients are supine, with their knees bent over a bolster for improved comfort and to help defecation. The left lateral decubitus position can be used as an alternative. Approximately 120 to 180 cc of ultrasound gel are instilled into the rectum before scanning. The gel is expelled during the evacuation portion of the examination, and absorbent pads and diapers can be used to facilitate clean-up.
A typical MRD protocol ( table 1 ) includes axial, sagittal, and coronal T2 weighted sequences of the whole pelvis to assess anatomy. A small field-of-view oblique-axial high-resolution T2-weighted sequence along the anal canal is recommended to evaluate the anal sphincter complex. For the dynamic portion of the examination, a balanced steady-state free precession sequence is obtained in the mid-sagittal plane through the anorectal junction. The patient is imaged for approximately 30 seconds while performing Kegel (squeeze), defecation (evacuation), and Valsalva (strain) maneuvers. The defecation maneuver should be performed at least 3 times to achieve maximal gel evacuation. Although Valsalva was traditionally obtained before defecation, it is now recommended as a postevacuation maneuver to improve detection of intussusceptions and grading of anterior and middle compartment prolapse that may have been masked by the distended gel-filled rectum before defecation.
| Sequence | Plane | Static or Dynamic | Purpose |
|---|---|---|---|
| T2 turbo/fast spin echo | Axial, whole pelvis | Static | Anatomy |
| T2 turbo/fast spin echo | Coronal, whole pelvis | Static | Anatomy |
| T2 turbo/fast spin echo | Sagittal, whole pelvis | Static | Anatomy |
| Balanced steady-state free precession (BTFE/FIESTA/trueFISP) | Sagittal, midline | Dynamic Kegel | Function |
| Balanced steady-state free precession (BTFE/FIESTA/trueFISP) | Sagittal, midline | Dynamic defecation, repeat at least 3 times or until evacuation is achieved | Function |
| Balanced steady-state free precession (BTFE/FIESTA/trueFISP) | Sagittal, midline | Dynamic Valsalva, after evacuation | Function |
| Recommended: High-resolution T2 | Axial oblique through anal canal | Static | Anatomy |
| Optional: T1 Gradient Echo | Axial | Static | Anatomy |
| Optional: Balanced steady-state free precession (BTFE/FIESTA/trueFISP) | Coronal and/or axial | Dynamic Valsalva, after evacuation | Function |
Limitations of Magnetic Resonance Defecography
Evacuation of rectal gel is critical to MRD accuracy; studies of upright and supine MRD found that defecation identified significantly more anterior and middle compartment prolapse, rectoceles, enteroceles, and intussusceptions compared to Valsalva alone without defecation. However, in practice, patients may not be able to expel the rectal gel because of insufficient effort, embarrassment, supine position, or obstructed defecation. Several techniques have been proposed to address these issues. Patient education and coaching before and during the examination may help to alleviate patient anxiety or shame and improve defecatory effort. A larger volume of rectal gel may be helpful to stimulate defecation in some cases. Patients can also be removed from the magnet to evacuate in the restroom and then brought back for postdefecation Valsalva; however, this may not be practical in most clinical settings. The MRD report should include a statement on whether defecation was achieved, and this should be accounted for at examination interpretation.
The non-physiologic position of MRD is often referenced as a limitation of the exam and a potential cause for discordant results compared with fluoroscopic defecography (FD) and physical examination (PE), which are performed in the seated upright position mimicking the physiology of defecation. Although it is generally accepted that supine MRD underestimates the presence and severity of pelvic floor abnormalities compared with upright examinations, early comparative studies were confounded by variations in technique, and subsequent studies have shown that supine MRD performs similarly to upright MRD and FD in detecting clinically significant pelvic prolapse. It is important to remember that MRD is not intended to replace PE, but rather should be used as a complement to identify occult abnormalities and anatomic defects that may alter treatment planning or risk of recurrent symptoms after surgery.
MRD is subject to the limitations that affect all MRI, including cost, motion, and susceptibility artifacts, and MR-incompatible implants. MRD is also limited for patients with claustrophobia, as sedation could impede adequate performance of the pelvic floor maneuvers and generally should not be used. Lack of radiologist familiarity with MRD is also a concern; however, this is improving with more widespread acceptance and performance of MRD and educational efforts by expert groups.
Alternate Diagnostic Tools
Fluoroscopic defecography
FD can be used to evaluate patients with OD and is able to diagnose anorectal descent, rectocele, pelvic floor dyssynergia, intussusception, and some cul-de-sac hernias. , FD is more sensitive than MRD for the detection of intussusception, although MRD can better differentiate mucosal from full-thickness intussusception. The anterior and middle compartments are not assessed at FD unless contrast is also instilled into the bladder and vagina (cystocolpoproctography); however, this is more invasive and may not be as well tolerated by patients as MRD with rectal gel alone.
FD is preferred by some referrers because of its physiologic positioning and use of thicker paste, which is more similar to stool consistency than ultrasound gel. If commercially produced paste is not available, a mixture of barium with potato starch can be created as an alternative. The examination requires the use of a commode, which can be purchased or constructed.
Because it is not as widely used as MRD, fewer radiologists are comfortable with FD, which is a major limitation. Additional limitations include the use of ionizing radiation and the inability to directly visualize the pelvic floor muscles and anal sphincter for abnormalities.
Dynamic pelvic floor ultrasound
Dynamic translabial ultrasound is another imaging modality used to evaluate the pelvic floor. Ultrasound can demonstrate pelvic organ prolapse and can be used to assess the levator hiatus, levator attachments, and anal sphincter complex for defects. Ultrasound is also the preferred test to assess midurethral slings. However, dynamic translabial ultrasound is not performed with a defecation maneuver, limiting the evaluation of OD. Additional limitations include lack of training, radiologist comfort, and operator dependence.
Additional diagnostic tools
Patients with pelvic floor disorders may undergo additional clinical and imaging tests, depending on their symptoms. Pelvic organ prolapse can be evaluated and graded on physical examination using a system such as the Pelvic Organ Prolapse Quantification system (POP-Q). , Anorectal manometry and the balloon expulsion test are used to evaluate anorectal tone, sensation, and function. Colon transit studies, such as a radio-opaque marker study, are performed to assess colonic motility in patients with constipation. ,
Normal anatomy
The female pelvic floor is divided into 3 compartments. The anterior compartment contains the urethra and bladder; the middle compartment contains the vagina and uterus, and the posterior compartment contains the anus and rectum. When MRD is performed in men, the anterior and posterior compartments are evaluated. Patients with pelvic floor disorders frequently have abnormalities in more than 1 compartment.
The 3 compartments of the pelvic floor share a multilayered support structure. The first layer of support is the endopelvic fascia, which covers the pelvic floor organs and attaches them to the bony pelvis via ligaments (ie, the uterosacral ligament), some of which can be seen on MRI. The thin fascial layer itself cannot be seen on MRD, and the positioning and shape of the urethra and vagina can be used to infer a fascial tear. , The middle layer of pelvic floor support is the muscular pelvic diaphragm, which supplies active pelvic tone at rest and strain via the levator ani. The perineal membrane is the inferior layer of the pelvic floor and acts predominantly as a passive attachment site.
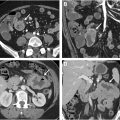
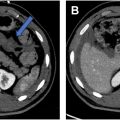
The levator ani muscle group is made up of the pubococcygeus, iliococcygeus, and puborectalis muscles ( Figs. 1 and 2 ). The pubococcygeus and puborectalis are oriented antero-posteriorly and are well-visualized in the axial plane. The iliococcygeus has a transverse orientation and is often better seen in the coronal plane, where it normally appears upwardly convex. The pubococcygeus and iliococcygeus fuse together posteriorly before inserting on the coccyx. This fused portion is called the levator plate and should be oriented horizontally on a midsagittal image. The puborectalis attaches on both sides of the pubic symphysis and slings around the anorectal junction ( Fig. 2 ). The puborectalis is a key landmark on MRD for the levator hiatus, anorectal junction, and interpretive reference lines.


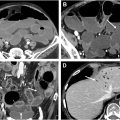
The anal sphincter complex ( Fig. 3 A, B ) includes the internal anal sphincter (IAS) and external anal sphincter (EAS). The IAS is the continuation of the circular smooth muscle layer of the rectal wall and appears intermediate in signal on T2W images. The EAS is made up of the puborectalis and additional skeletal muscle components and appears low signal on T2.