Magnetic resonance neurography (MRN) of the brachial plexus (BP) has witnessed significant technical advancements in recent years, with improved spatial and contrast resolution enabling greater demonstration of nerve detail and corresponding pathology. In this article, we provide an update on the technical considerations for MRN of the BP, including surface coils and advanced imaging sequences, and review the standard technical approach to investigating common BP pathology using MRN. Suggested imaging protocol modifications are discussed depending on common clinical scenarios of typical MRN BP referrals, and quintessential imaging findings of these pathologies are highlighted.
Key points
- •
Recommended brachial plexus magnetic resonance neurography protocols utilizes flexible surface coils conforming to the neck and shoulder, obtaining high signal-to-noise ratio and spatial resolution.
- •
Heavily T2-weighted sequences with fat suppression provide the greatest nerve-to-background contrast resolution, with images acquired both longitudinal and orthogonal to the BP.
- •
The baseline MRN BP protocol is adapted based on the clinical question and targeted nerve(s).
- •
Specialized sequences added to the standard protocol include 3-dimensional myelographic sequences, vascular suppression techniques, multispectral imaging for around metal, and bone sequences with CT-like detail.
| ABER | abduction/external rotation |
| BFFE | balanced fast field echo |
| BP | brachial plexus |
| DESS | double echo steady-state |
| DSN | dorsal scapular nerve |
| DTI | diffusion tensor imaging |
| FIESTA | fast imaging employing steady-state acquisition |
| FISP | fast imaging with steady-state procession |
| FOV | field of view |
| FSE | fast spin echo |
| GRE | gradient recalled echo |
| HGC | hourglass-like constriction |
| IV | intravenous |
| IR | inversion recovery |
| LTN | long thoracic nerve |
| MENSA | multi-echo in steady-state acquisition |
| MRA | magnetic resonance angiography |
| MRN | magnetic resonance neurography |
| MSI | multispectral imaging sequence |
| PD | proton density |
| PDw | proton density weighted |
| PSIF | time-reversed FISP |
| PTS | Parsonage-Turner syndrome |
| SAN | spinal accessory nerve |
| SNR | signal-to-noise ratio |
| SPGR | spoiled gradient recalled acquisition |
| SSN | suprascapular nerve |
| STIR | short-tau inversion recovery |
| TE | echo time |
| TOS | thoracic outlet syndrome |
| TI | inversion time |
| TR | repetition time |
| TIGRE | T1-weighted gradient echo with radiofrequency fat saturation |
| TRIVE | T1-weighted high-resolution isotropic volume examination |
| T 1 w | T1-weighted |
| T 2 w | T2-weighted |
| VIBE | volumetric interpolated breath-hold |
| ZTE | zero echo-time |
| 3D | 3-dimensional |
Introduction: technical considerations
High-quality, magnetic resonance neurography (MRN) of the brachial plexus (BP) hinges on maximizing the nerve-to-background contrast ratio. , Our institutional BP MRN protocol utilizes unilateral imaging with the combinations of flexible surface coils that conform as closely as possible to the contours of the neck and shoulder for the best possible spatial resolution. Heavily T2-weighted, fat-suppressed sequences provide the greatest nerve contrast resolution, with imaging planes oriented longitudinal and perpendicular to the main plexus segments.
The standard MRN BP protocol may be modified in advance by the overseeing radiologist depending on the clinical question. BP cases may also be reviewed by the radiologist in real-time, adjusting imaging parameters or repeating sequences if image quality is suboptimal. Evaluating the BP with high-resolution MRN may initially be challenging for radiologists, especially when interpreting nonstandard, oblique sagittal planes. The increase in published literature on MRN BP nerve anatomy and the development of online nerve imaging atlases have made this training more accessible in recent years. , ,
Obtaining diagnostic-quality MRN of the BP also relies on technologists with experience in coil setup and prescription planes. For unilateral imaging, the BP should ideally be positioned close to the magnetic field isocenter to reduce B 0 inhomogeneity for adequate fat suppression. Additionally, the technician’s experience with patient positioning and optimal breathing patterns can help minimize motion degradation.
Coils
Unilateral BP coverage using a combination of high-density, flexible receiver coils maximizes signal-to-noise ratio (SNR) and spatial resolution, with parallel imaging applied to reduce scanning time. Dedicated research coils currently being tested for cervical MRN may be extended to the BP in the future, improving anatomic conformity. High impedance coils and stretchable coils containing liquid metal technology are in early stages of investigation and may provide additional conformity.
3-Dimensional Sequences
A 3-dimensional (3D), heavily T2-weighted, thin-slab, fast-spin-echo sequence with short-tau inversion recovery (STIR) can be used to evaluate the longitudinal morphology of individual nerves, and when acquired isotropically, can be readily reformatted into multiple arbitrary planes. , This sequence also facilitates characterization of active muscle denervation edema. , Advances in 3D imaging across most vendors include the combined use of deep learning and parallel imaging reconstruction to reduce the historically long acquisition times. ,
Magnetic Resonance Angiography/Contrast
Intravenous (IV) contrast medium is frequently requested by referring clinicians. Most BP cases, however, typically do not require IV gadolinium-based contrast medium, with nerve pathology readily reflected by high signal on T2-weighted, fat-suppressed sequences. Gadolinium contrast medium, however, can be used in combination with a 3D-STIR sequence to shorten blood’s T1 and T2 signal, thereby increasing nerve contrast resolution. Vascular suppression is important for visualizing smaller branches of the BP (eg, suprascapular nerve [SSN], long thoracic nerve [LTN], and axillary nerve) that may be confounded by similarly sized blood vessels. IV gadolinium contrast medium is typically used for MR angiography (MRA) in patients with suspected thoracic outlet syndrome (TOS), in the setting of neoplasm to characterize a primary or secondary malignancy involving the BP, or occasionally to further characterize inflammatory polyneuropathies. , ,
Tailoring brachial plexus magnetic resonance neurography for specific clinical scenarios
The recommended protocol for most BP MRN examinations includes a combination of coronal and oblique sagittal, heavily T2-weighted sequences ( Table 1 ), updated from Davidson and colleagues, 2022 . Applying a universal protocol, however, is not recommended. Instead, a baseline protocol should be tailored to the type and location of suspected pathology. In the following sections, we provide a case-based imaging approach to common clinical scenarios.
| Standard BP Sequences | TOS/Tumor | Bone (including TOS) | Neck (Avulsion Assessment) | ||||
|---|---|---|---|---|---|---|---|
| Sequence | 2D PDw-FSE | 3D T 2 w-FSE | 2D T 2 w-FSE | 2D PDw-FSE | 3D ZTE | 3D SPGR/VIBE | MENSA/DESS/PSIF/FIESTA/True FISP |
| Nominal scan time (min:s) | 2:00 | 4:30 | 4:30 | 2:00 | 5:00 | 4:00 | 5:30 |
| Orientation | Axial | Double oblique-coronal | Coronal and oblique-sagittal | Sagittal or oblique sagittal | Axial or coronal | Axial or coronal | Axial |
| FOV (cm) | 28.0 | 32.0×16.0 | 16.0 | 16.0 | 28.0 | 25.6 | 16.0 |
| TR/TE (ms) | 4200/35 | 3300/60 | 4300/85 | 4200/35 | 255/0 | Min/In-phase | Min/Min |
| TI (ms) | — | 250 | — | — | — | — | — |
| GRE Flip Angle ( o ) | — | — | — | — | 1 | 4 | Variable |
| Matrix size (frequency x phase) | 512 × 352 | 320 × 160 | 320 × 224 | 384 × 320 | 256 × 256 | 256 × 256 | 320 × 320 |
| Slice thickness (mm) | 3 | 1 | 2.5 | 3 | 1.1 | 1 | 2.0 |
| Fat suppression | None | IR | Dixon or chemical saturation | None | None | None | None (FIESTA/True FISP) or water excitation (MENSA/DESS/PSIF) |
| Optional | — | Flow suppression crusher pulses Use of IV gadolinium contrast for vascular suppression | Respiratory gating | Neutral and ABER arm positions | — | With fat suppression and higher flip angle for steady-state MRA | — |
Traumatic Plexus Injuries
The goal of MRN following BP trauma is to localize and grade the severity of an injury. The decision of when to image following injury must balance the timing of any planned interventions with the likelihood of soft tissue edema obscuring nerve segments and motion artifact related to patient discomfort in the acute setting. For suspected iatrogenic injuries, early imaging is recommended to determine whether surgical intervention is needed.
A 17-year-old high-school football player sustains a compression load to the hyperextended neck during a tackle. He immediately experiences right shoulder weakness in forward flexion and mild weakness in shoulder and external rotation. Team doctors suspect he has sustained a “stinger injury” and order a BP MRN examination.
In this scenario, the standard, unilateral MRN BP protocol can be used. As football and rugby athletes are typically broad-chested and wide-shouldered, standard coils may be inadequate to cover the shoulder and neck regions and positioning the plexus at the magnet’s isocenter may be impossible. Another imaging challenge in this patient cohort is a paucity of subcutaneous and deep intermuscular fat that otherwise outline the nerve’s course. Larger-sized coils may be needed, along with technical adjustments to increase SNR while maintaining reasonable spatial resolution.
Images are reviewed in real-time for early denervation edema patterns. Depending on the pattern of muscle involvement, the protocol can then be tailored to the involved nerve or nerve territory. It should be noted that if the lower portions of the proximal plexus are affected (C7-T1), denervation would manifest in the arm and forearm muscles (outside of the imaged field-of-view of the shoulder girdle). Simultaneous assessment of concomitant injuries is also important, particularly clavicular and rib fractures, sternoclavicular or acromioclavicular joint injuries, and shoulder dislocations.
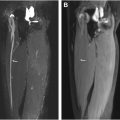
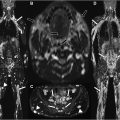
In this case, the patient sustained an acute neuropraxia involving the C5 nerve root, characteristic of a “stinger” or “burner” injury ( Fig. 1 ). A “stinger” injury reflects an acute, transient traumatic BP irritation, most frequently involving the C5 or C6 nerve roots, and typically resolves within minutes to hours but can last longer. It commonly occurs during high-contact sports like American football, rugby, and wrestling. The axillary nerve is also commonly injured in contact sports, as it courses inferior to the glenohumeral joint and is vulnerable to traction neuropraxia following anterior glenohumeral dislocations ( Fig. 2 ).


A 33-year-old male is brought to the Emergency Department with right arm weakness after being thrown from his electric scooter in a high-velocity collision. Initial trauma computed tomography (CT) identifies a cervical spinal fracture. He maintains finger movement but reports numbness and weakness in the right upper extremity. Clinical examination demonstrates 0/5 strength in shoulder abduction, external rotation, elbow flexion, and elbow extension. Clinical suspicion is for BP nerve root injury, and MRN is requested to assist in diagnosis and surgical planning.
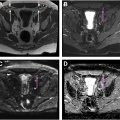
In this high-velocity, acute traumatic setting, extensive soft tissue edema and hematoma can limit evaluation of the postganglionic BP on MRN. Other limitations to image quality include patient pain and support lines or tubes that limit patient and coil positioning and make routine breathing instructions difficult to follow. At our institutions, these cases are preferentially performed within daytime hours during which full technical and medical/nursing support is available. In the acute period, other injuries in the region should be prioritized, including vascular repair, fracture fixation, and urgent spinal intervention. In the United States, peripheral nerve surgeons typically do not perform emergency plexus surgery, instead waiting several weeks for the nerve deficit to evolve and inform surgical planning. Therefore, MRN may also be delayed by 1 to 2 weeks to allow swelling to subside and improve the diagnostic imaging yield without impacting management. In this case, imaging was performed 3 months postinjury ( Fig. 3 ). Most of the soft tissue edema had resolved, allowing the nerve root injury and extent of nerve stump retraction to be assessed.

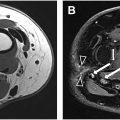
In a high-velocity, traumatic BP scenario, standard MRN pulse sequences are initially obtained. If oblique sagittal Dixon sequences are motion-degraded despite the use of respiratory gating, an oblique sagittal STIR may be considered as it is more robust to respiratory motion artifact. Additionally, high-resolution oblique sagittal proton density (PD) sequences can also be extremely helpful in determining the presence or loss of fascicular architecture, with the latter suggesting neurotemesis injury, a high grade injury requiring surgical intervention.
Cervical “MR myelography” for preganglionic injury evaluation can be challenging due to motion artifact. Heavily T2-weighted, balanced, steady-state gradient echo sequences (eg, fast imaging employing steady-state acquisition [FIESTA], T2 true fast imaging with steady-state procession [true FISP], or balanced fast field echo [BFFE]), can be used for MR myelography but are prone to motion from breathing and swallowing and are subject to banding artifacts in the lower cervical and upper thoracic regions. Another type of gradient echo sequence, 3D double echo steady-state (DESS), has been shown to provide high contrast resolution between fluid and nerve rootlets with high spatial resolution. In DESS, cerebrospinal fluid will appear dark due to its inherent high susceptibility to motion, giving a reverse myelogram quality to the images. , Additionally, diffusion tensor imaging (DTI) can characterize longitudinal tissue microstructures with potential use as a proxy for nerve health. DTI of the BP is still the subject of research, , but studies that have assessed its role in evaluating proximal root avulsions from traumatic BP injuries show promising results.
For clinically suspected or known fractures, a bone-like quality sequence (eg, zero echo-time [ZTE]) or a radio-frequency-spoiled gradient echo sequence (eg, volumetric interpolated breath-hold examination, T1-weighted high-resolution isotropic volume examination [TRIVE], or T1-weighted gradient echo with radiofrequency [RF] fat saturation [TIGRE]) can be used to assess osseous pathology. If acquired isotropically, these sequences can be reconstructed into 3D imaging planes, allowing for assessment of the relationship of the fracture to the injured nerve segments and possibly obviating the need for CT.
When assessing traumatic proximal nerve root injuries, an important differentiation is determining whether the injury is preganglionic versus postganglionic. The dorsal root ganglion can be challenging to identify in the cervical spine due to its small size but is typically positioned in the far lateral foramen. , Epidural hematoma with pseudomeningocele can be indicative of preganglionic nerve rootlet avulsion. , If a postganglionic nerve injury is detected, the nerve gap should be noted as well as the viable nerve stump caudal to the foramen for nerve grafting or transfer planning.
Imaging Pearls for traumatic BP injuries
How early to image? – Soft tissue edema can obscure BP anatomy if imaging is performed acutely. However, imaging early may facilitate earlier intervention by defining the extent of the injury. Imaging for high-velocity traumatic BP injuries is optimally performed at least 2 to 4 weeks postinjury to allow soft tissue edema to subside.
Additional Sequences in Trauma BP Cases
- •
Factures: Consider ZTE or other 3D gradient echo sequences
- •
Proximal nerve root injury: Heavily T2-weighted balanced steady-state gradient echo sequences or 3D DESS imaged through the neural foramina
- •
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree