Management of Vascular Complications
John Chung
Lindsay Machan
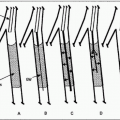
Pseudoaneurysms
The most common vascular access site complication requiring intervention is pseudoaneurysm formation. Surgical repair has surprisingly high complication rates, from 19% to 32% (4), including inadequate wound healing, femoral neuralgias, and lymphatic leaks; thus, ultrasound-guided procedures have revolutionized their treatment (5).
Indication
1. Identification of an arterial access site pseudoaneurysm. Conservative, observational management has largely been abandoned.
Contraindications
Absolute
1. Hemodynamically unstable patient
2. Active hemorrhage (retroperitoneal or percutaneous); expanding hematoma
3. Impending skin necrosis due to size of hematoma/pseudoaneurysm
4. Acute distal limb ischemia due to compression effects of hematoma/pseudoaneurysm
5. Active infection at the site of percutaneous access
Relative
1. Width of pseudoaneurysm neck >8 mm
2. Lack of any discernible pseudoaneurysm neck
3. Pseudoaneurysm sac diameter <10 mm (increased risk of arterial thrombosis)
Preprocedure Preparation
1. Detailed imaging, most commonly with ultrasound, or alternatively computed tomographic angiography (CTA) or magnetic resonance angiography (MRA). The extent and morphology of the pseudoaneurysm should be identified, including the number of lobes the pseudoaneurysm has as well as the width and length of its neck. If performing ultrasound, the Doppler waveform pattern of the outflow artery should also be assessed.
Table 4.1 Common Complications Following Percutaneous Arterial Access | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
2. Recent laboratory data should be obtained, including complete blood count (CBC), platelets, and international normalized ratio (INR).
3. Doppler or palpation assessment of ipsilateral foot arteries (dorsalis pedis, tibialis posterior) immediately prior to percutaneous therapy
Procedure
Ultrasound-Guided Compression
1. The first described ultrasound-guided management of iatrogenic pseudoaneurysms (5). It remains the preferred treatment option for pseudoaneurysms <1 cm and is still an acceptable therapy when thrombin is not available.
2. Inject copious amounts of local anesthetic. Consider intravenous sedation. Due to extensive bruising, these patients are often exquisitely tender.
3. A linear array (4 to 7 MHz) ultrasound transducer is placed on the affected groin with direct visualization of the pseudoaneurysm neck and body (or lobe closest to the neck in a multilobed, complex pseudoaneurysm) as well as the artery from which the pseudoaneurysm arises.
4. With real-time color Doppler sonographic guidance, pressure is applied on the pseudoaneurysm via the probe to eliminate flow through the pseudoaneurysm while maintaining flow through the parent artery.
5. Pressure is slowly alleviated at 10-minute intervals to assess for any persistent flow through the pseudoaneurysm.
6. At the first instance persistent flow is identified, step 4 is repeated until the pseudoaneurysm internal flow remains obliterated when transducer pressure is fully released.
7. Limitations of this technique include the relatively long time required, patient discomfort with possible need for sedation, and higher failure rates relative to other ultrasound-guided treatment methods.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree