Abstract
Flow-diverting stents are an established endovascular treatment for internal carotid artery (ICA) dissections, but their long-term durability remains a concern, particularly in cases involving mechanical stress. A 40-year-old male with Eagle syndrome presented with a minor stroke due to left ICA dissection and underwent successful flow-diverter placement. While initial follow-up was unremarkable, subsequent imaging revealed stent fractures at 3 and 7 months, leading to complete ICA occlusion by 8 months. Despite this, the patient remained asymptomatic due to robust collateral circulation. Two-year follow-up imaging confirmed stable ICA occlusion, no new ischemic lesions, and scattered stent fragments in the subarachnoid space, which were best visualized with susceptibility-weighted MRI. This case underscores the potential for delayed stent fractures and asymptomatic ICA occlusion in Eagle syndrome, highlighting the importance of advanced imaging in long-term follow-up and the need for further research on stent durability in high-stress vascular regions.
Introduction
Eagle syndrome, caused by an elongated styloid process, can result in vascular complications such as internal carotid artery (ICA) dissection. These complications pose significant risks, including ischemic events, which may necessitate surgical or endovascular intervention [ ]. Flow-diverting stents are increasingly used to treat ICA dissections and pseudoaneurysms, offering vessel stabilization and thrombosis prevention.
However, stent fractures due to mechanical stress from the styloid process remain a rare but critical complication, with limited data on long-term outcomes. This report presents a 2-year follow-up of a patient with Eagle syndrome who developed ICA occlusion following flow-diverter fracture. It highlights imaging findings, mid-term clinical outcomes, and the implications for managing such cases.
Case report
History and prior treatment
A patient in their 40s presented with a minor stroke (NIHSS 1, mRS 1) attributed to left ICA dissection caused by an elongated styloid process measuring 5.4 cm. Initial symptoms included ptosis, visual disturbances, and transient right-hand numbness. Following heparinization, the patient was discharged on antiplatelet therapy.
Treatment and initial follow-up
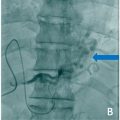
Elective endovascular treatment was performed 6 months later with a 5.5 mm dual-layer flow-diverting stent (FRED). Postprocedural imaging showed optimal stent placement and no thrombus formation. However, fractures in the stent were detected at 3 and 7 months, leading to ICA occlusion by 8 months. Despite this, collateral circulation via the Circle of Willis maintained perfusion, and the patient remained asymptomatic.
Two-year follow-up
At the 2-year follow-up, a multimodal imaging series was conducted, including non-contrast CT (NECT) of the head, contrast-enhanced MRI of the head and neck with vessel wall imaging, and contrast-enhanced flat-panel CT angiography. The following key findings were noted:
- 1.
Persistent ICA occlusion and collateral adaptation
The cervical portion of the left ICA remained occluded. Compared to preinterventional imaging, the posterior communicating artery on the left had enlarged from 1.2 mm to 2.4 mm, suggesting a compensatory adaptation to maintain cerebral perfusion after the ICA occlusion. The Circle of Willis demonstrated robust collateral circulation without evidence of hemodynamic compromise.
- 2.
Stable ischemic changes and preserved cerebral perfusion
No new ischemic lesions were detected compared to previous imaging. The small postischemic lesion in the left parietal white matter, initially observed following the minor stroke, had decreased in size on FLAIR sequences. Perfusion imaging showed no significant hemispheric asymmetry, further supporting adequate collateral supply.
- 3.
Detection of stent fragments in the subarachnoid space
Follow-up CT revealed 8 hyperdense structures distributed in the left ICA territory, with more visible in soft tissue window settings. These high-density foreign bodies, located within the subarachnoid space without signs of hemorrhage or posthemorrhagic calcifications, were suspected to be fragments of the fractured flow-diverting stent.
- 4.
MRI confirmation of fragment distribution
Susceptibility-weighted imaging (SWI) detected blooming artifacts corresponding to the high-density structures seen on CT. Additionally, multiple smaller blooming artifacts were present that had not been visible on initial MRI or postintervention CT. MR-TOF angiography and contrast-enhanced T1-weighted sequences localized these fragments in continuity with small cortical vessels, suggesting their distribution within the ICA vascular territory.
Clinical status
Despite the complete occlusion of the left ICA, the patient remains functionally independent and asymptomatic concerning cerebral perfusion. Over the past 2 years, they have reported occasional headaches and transient visual sensations affecting the right eye, for which they are receiving outpatient treatment for migraine with aura. The patient continues to manage daily activities and work without major limitations ( Figs. 1 and 2 ).