Monitoring and Reporting of Complications
Jeffrey P. Kanne
LEARNING OBJECTIVES
1. Define sentinel event and near miss
2. List causes of errors in medical imaging interpretation
3. Describe types of medical error reporting systems
In 2000, the Institute of Medicine (IOM) published its 1999 report, “To Err Is Human: Building a Safer Health System,” drawing attention to medical errors.1 Complications and injuries associated with the delivery of health care continue to face scrutiny from various stakeholders, including patient advocacy groups, government agencies, accrediting and certifying organizations, insurance companies, employers, and patients. Not only do complications from medical treatment result in patient harm, but they also result in increased costs to the health-care enterprise. The IOM estimated that 98,000 patients died each year as a result of medical errors.
Adverse events are those that are associated with patient harm as a result of the administration of health care. A preventable adverse event is one that is the result of a medical error, which is defined as a behavior that falls below the standard of care.2 Adverse events occur in approximately 3% of hospitalizations, and around 10% of adverse events lead to patient deaths.1,3
A core mission of quality improvement in health care is to identify medical errors and their causes for improving patient safety by reducing the number of errors. Risk management in health care has shifted from a reactive process to one of prevention.4
TYPES OF ERRORS
Sentinel Events
The Joint Commission (TJC) defines a sentinel event as a patient safety event that reaches the patient and results in death, permanent harm, or severe temporary harm requiring intervention to sustain life (Table 6.1). Other events considered sentinel include suicide of any patient receiving care, treatment, or services in a staffed around-the-clock care setting or within 72 hours of discharge, including from the organization’s emergency department (ED); unanticipated death of a full-term infant; discharge of an infant to the wrong family; and abduction of any patient receiving care, treatment, or services. Although accredited organizations are not required to report sentinel events to TJC, they are strongly urged to do so.
Table 6.1 SENTINEL EVENTS. | ||||||
|---|---|---|---|---|---|---|
|
Near Misses
Near misses are safety events that do not reach a patient or result in minimal harm (Table 6.2). A more positive term is “good catch,” reflecting that the error was detected and corrected before reaching the patient. Unfortunately, near misses tend to receive less attention than sentinel events despite the fact that a number of opportunities for improvement can be garnered from studying processes and practices that result in near misses.
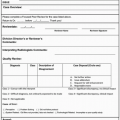
Table 6.2 EXAMPLE OF NEAR MISSES IN RADIOLOGY DEPARTMENT. | |
|---|---|
|
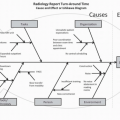
CAUSES OF ERRORS
Medical errors can be caused by single or multiple contributing factors that include limited or lack of knowledge, insufficient experience, fatigue, carelessness, and faulty judgment.5
In radiology, errors can lead to delay in diagnosis and treatment, failure to recognize treatment-related complications, performing a study that is contraindicated or not indicated, or failure to adequately supervise and monitor an examination.6 Errors in diagnostic radiology are common and are often multifactorial (Table 6.3). Environmental factors such a room lighting, available clinical information, index of suspicion, comparison studies, old radiology reports,7 and psychophysiologic characteristics of human visual perception8 all play into the complex process of medical imaging interpretation.9
For image interpretation, three types of errors have been described.10 Scanning error is the failure to fixate on the area of the abnormality. Various factors can contribute to scanning error, including lack of search pattern, eye fatigue, and interruptions. Recognition error is failure to recognize the abnormality. Factors that can contribute to scanning error include eye fatigue, room ambience, lack of experience, and technical limitations (artifact, noise, etc.). Decision-making error, the most common, is the incorrect interpretation of abnormal finding as normal or a normal finding as abnormal. Another important type of observational error in diagnostic radiology is satisfaction of search, which occurs when an abnormality is overlooked because another one is found. Satisfaction of search can be associated with scanning error, recognition error, or decision-making error.
ERROR REPORTING SYSTEMS
Error reporting systems can be defined as mandatory or voluntary. Some organizations may contract with third-party vendors while other organizations develop their own error reporting systems.
Mandatory Reporting Systems
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree