MR imaging is a valuable imaging tool in the assessment of spinal arthritides, allowing the radiologist to formulate a rational differential diagnosis and construct a meaningful radiologic report. Of this, spondyloarthritis has garnered the most attention over the years given its debilitating symptoms and disabling effect. MR imaging depicts both inflammatory and structural lesions in the spine and SI joints and a systematic anatomic approach in appraising these lesions can aid in proper diagnosis. Combined with careful correlation with clinical findings and biomarkers, MR imaging is an instrumental tool in the diagnosis and treatment planning of spinal arthritides, particularly spondyloarthritis.
Key points
- •
MR imaging plays a pivotal role in the evaluation of spinal arthritides, enabling formulation of an appropriate and rational differential diagnosis.
- •
Amongst the various arthritides, axial spondyloarthritis is the most incapacitating type, necessitating careful imaging assessment.
- •
MR imaging detects both inflammatory and structural lesions in the spine and sacroiliac joints, and MR imaging reports should contain a detailed description of these lesions.
- •
These lesions are best assessed using a systematic anatomic approach, carefully taking into account definitions and criteria set forth by the Assessment of Spondyloarthritis International Society.
| AS | ankylosing spondylitis |
| ASAS | Assessment of Spondyloarthritis International Society |
| axSpA | axial spondyloarthritis |
| BME | bone marrow edema |
| CR | conventional radiography |
| CRP | C-reactive protein |
| CT | computed tomography |
| DISH | diffuse idiopathic skeletal hyperostosis |
| ESR | erythrocyte sedimentation rate |
| ESSR | European Society of Skeletal Radiology |
| OA | oteoarthritis |
| pSpA | peripheral spondyloarthritis |
| PsSpA | psoriatic arthritis |
| RA | rheumatoid arthritis |
| r-axSpA | radiographic axSpA |
| SASSS | Stoke ankylosing spondylitis spine score |
| SI | signal intensity |
| SI joint/s | sacroiliac joint/s |
| SpA | spondyloarthritis |
| STIR | short tau inversion recovery |
| T1-W | T1-weighted |
| T2-W | T2-weighted |
| TIRM | turbo inversion recovery magnitude |
Introduction
MR imaging plays a major role in research and clinical management of patients with spinal or axial arthritides including spondyloarthropathy or spondyloarthritis (SpA), osteoarthritis (OA) and rheumatoid arthritis (RA). Its ability to differentiate between these conditions stems from its capacity to identify unique imaging features specific to each disease. OA predominantly affects the intervertebral discs, facet joints, and other axial skeletal structures, with hallmark findings like cartilage degeneration, subchondral bone remodeling, and osteophyte formation. Axial spondyloarthritis (axSpA) on the other hand, commonly targets vertebral corners, endplates, costovertebral joints, and facet joints, with characteristic MR imaging findings such as bone marrow edema, vertebral corner inflammation, and sacroiliitis. In contrast, RA frequently involves the cervical spine, particularly the atlanto-axial region, where MR imaging can reveal pannus formation, synovitis, and erosion. Although these conditions have distinct imaging patterns, overlap can occur, such as inflammation in facet joints observed in both OA and SpA. The superior sensitivity of MR imaging to early inflammatory changes and structural abnormalities enables accurate differentiation between these disorders, facilitating tailored treatment strategies and improved patient outcomes. Amongst these, axSpA is usually the most incapacitating type, and will be the main focus of this article.
SpA is a group of inflammatory diseases previously referred to as seronegative or “human leukocyte antigen-B27 (HLA-B27)-associated” spondyloarthropathies, encompassing conditions such as psoriatic arthritis, ankylosing spondylitis (AS), enteropathic spondyloarthritis associated with inflammatory bowel disease, and reactive arthritis. In 2009, the Assessment of SpondyloArthritis International Society (ASAS) redefined the concept of spondyloarthritis, categorizing it into 2 main subtypes: axSpA, which predominantly affects the spine and sacroiliac (SI) joints, and peripheral SpA (pSpA), which involves peripheral joints. This updated classification provides a more precise understanding of the disease and its clinical manifestations. The same group more recently clarified that ‘radiographic’ axSpA (r-axSpA) is the AS equivalent of the ASAS axSpA criteria, with patients fulfilling the imaging arm based on radiographic sacroiliitis. For simplicity, the term axial spondyloarthritis ( axSpA ) will be used to refer to the historical term ankylosing spondylitis throughout this radiologic review for consistency.
Imaging considerations
Conventional radiography (CR) is widely accepted for assessing chronic structural changes in axSpA. The 1984 modified New York criteria, which rely on radiographic findings, are often referenced for diagnosis. However, these findings become apparent only after substantial structural damage has already occurred when treatment options, which are primarily focused on slowing down disease progression, may be less effectual. In general, CR remains the initial imaging tool of choice in the evaluation of arthritides and spondyloarthropathies. However, the American College of Rheumatology/Spondyloarthritis Research and Treatment Network/Spondylitis Association of America (ACR/SPARTAN/SAA) guidelines advise against routine spine radiographs at scheduled intervals for monitoring disease progression as this practice involves unnecessary radiation exposure and is unlikely to alter treatment decisions in most cases. This recommendation emphasizes the importance of balancing the diagnostic utility of imaging with the need to minimize unnecessary procedures.
Structural lesions to be evaluated in the spine include vertebral corner erosions, enthesophytes, vertebral squaring, sclerosis and erosions of the vertebral endplate, disc calcifications, syndesmophytes, bony bridging, and/or intervertebral ankylosis. Syndesmophytes, new bone formation, and ankylosis of the vertebral column are considered pathognomonic findings; on the other hand, syndesmophytes are among the strongest predictors of radiographic progression in axSpA, reflecting the structural component of the disease, though disease activity and other modifiable factors also play crucial roles. Scoring systems include the Stoke AS spine score (SASSS), the modified SASSS, the radiographic AS spinal score, the Bath AS radiology index, and the psoriatic arthritis spondylitis radiology index. Structural lesions in the SI joints are erosions, pseudo-widening, sclerosis, bony bridging, and/or ankylosis. Of these, erosions in the iliac side of the joint are the earliest radiographic findings.
Computed tomography (CT) detects the same structural lesions more optimally than CR and MR imaging , , but is less used than MR imaging because of a much higher radiation exposure. Owing to recent technological advances, it is now possible to perform CT of the spine with relatively low-radiation dose without overlapping of osseous structures, a typical pitfall in CR. In the SI joints, CT is performed by acquiring multiplanar oblique coronal and oblique axial scans oriented parallel and perpendicular to the long axis of sacrum. While it is the gold standard in the detection of early erosions, it is preferred that both inflammatory (acute or active) and structural (chronic) lesions are evaluated by a single imaging modality rather than 2 separate imaging modalities, putting MR imaging at an advantage over CT. Synthetic CT is a novel technique that generates “CT-like images” from MR imaging scans based on T1-weighted (T1-W) and T2-weighted (T2-W) sequences, and Dixon or zero echo time/ultra-short echo time, susceptibility-weighted imaging, and gradient recalled echo sequences using a deep learning-based image synthesis method. Jans and colleagues found synthetic CT to have greater diagnostic accuracy than T1-W sequences in the detection of erosion, sclerosis, and ankylosis using conventional CT as the reference standard.
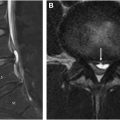
MR imaging
The primary benefit of MR imaging over CR and CT is the detection of bone marrow edema (BME) or osteitis, a key manifestation of early axSpA. , BME is characterized by high signal intensity (SI) on short tau inversion recovery (STIR) or equivalent water-sensitive sequences, and by hypointense SI on T1-W images. In the diagnostic criteria proposed by the ASAS ( Fig. 1 ), BME is the only MR imaging finding that may result in a ‘positive MR imaging’ for sacroiliitis. , MR imaging is the only imaging technique that can optimally detect both inflammatory and structural lesions of axSpA in the spine and SI joints; most recommended MR scanning protocols, for example, that of the European Society of Skeletal Radiology (ESSR) ( Table 1 ), highlight these 2 anatomic areas.

| Area | MR Imaging Sequences |
|---|---|
| SI joints | Coronal oblique T1-W Coronal oblique (STIR/TIRM), PD fat-suppressed (FS), T1-W FS or gradient-echo sequence Axial PD FS or STIR/TIRM Obligatory: minimum coronal oblique T1-W, coronal oblique STIR/TIRM and a cartilage sequence and visualization in 2 perpendicular planes |
| Spine, axSpA | Sagittal T1-W Sagittal STIR/TIRM Axial T2-W FS (if optimal assessment of BME at the posterior joints is needed) |
| Spine, RA | Sagittal T1-W Sagittal STIR/TIRM Axial T2-W FS of the atlantoaxial and atlanto-occipital and, when needed, subaxial regions Coronal T1-W in cases with atlantoaxial and/or atlanto-occipital changes suspect for lateral or rotatory subluxation Postcontrast sagittal and axial T1FS are often needed for clear delineation of active inflammation. Additional coronal sequence in cases with atlantoaxial and/or atlanto-occipital changes. |
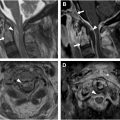
In other forms of spinal arthritides, MR imaging allows for grading of disc degeneration and facet OA and evaluation of the spinal cord, central canal, and neural foramen. Enthesitis that extends to the surrounding soft tissues , and infectious sacroiliitis that involves the iliopsoas are also best assessed by MR imaging. Because MR imaging allows for concomitant assessment of bone and soft tissue lesions, it is the best modality for appraisal of arthritides and spondyloarthropathies, which is best performed using an anatomic approach ( Fig. 2 ).

Overall, radiographs are generally inadequate for detecting early structural changes in axSpA. With advancements in pharmacologic treatments, MR imaging has become an essential tool for the early identification of inflammatory changes, allowing for detection of lesions shortly after symptom onset. This significantly enhances diagnostic confidence for rheumatologists, influencing treatment decisions. In addition to the early detection of inflammatory changes, the T1-W sequence is also considered superior to CR for identifying structural lesions in patients with axSpA. When radiographs are inconclusive and MR imaging is unavailable, CT provides an effective alternative for evaluating structural abnormalities. These advancements in imaging techniques are crucial for improving patient outcomes through timely and accurate diagnosis and tailored therapeutic strategies.
Clinical considerations and biomarkers
Though the central role of the radiologist in evaluating spinal arthritis revolves around detection of lesions, it remains of utmost prudence for the radiologist to refer to the patient’s clinical examination and chart during radiologic interpretation and reporting. Apart from MR imaging lesions, a clinical history of inflammatory back pain, enthesitis (heel), uveitis, dactylitis, and family history of spondyloarthropathy may help the radiologist favor axSpA over other differentials when imaging findings are equivocal or borderline. HLA-B27 remains a core biomarker for axSpA but is less reliable in early axSpA. C-reactive protein (CRP) levels fluctuate in many inflammatory conditions but are helpful parameters of disease activity in axSpA and have been shown to correlate with the ankylosing spondylitis disease activity score. Erythrocyte sedimentation rate (ESR) seems to be a less reliable marker of disease activity than CRP, although elevated ESR has been found to be independently associated with radiographic spinal progression. Beyond disease detection, inflammatory biomarkers are useful tools for monitoring disease activity, treatment response and outcomes, which, along with imaging findings, can aid in formulating a rational differential and sound therapeutic regimens.
Axial spondyloarthropathies
Anatomic Considerations
The SI joint is lined by irregular articular surfaces and reinforced by robust supporting ligaments that restrict vertical shear forces. It has limited mobility and primarily serves to transmit load from the axial skeleton to the lower limbs. There are 2 main parts in the articulation: the ventral joint or cartilaginous part; and the dorsal joint or the fibrous/ligamentous part. The upper and middle thirds of the ventral joint act as a weight-bearing area, and is thereby susceptible to mechanical or degenerative conditions. The lower third or the main body of the ventral joint is the primary region of interest in the context of axSpA. This part is predominantly cartilaginous/ fibrocartilaginous, giving the joint the overall characteristics of an enthesis and making it susceptible to spondyloarthritis and other inflammatory conditions. There is more fibrocartilage in the iliac side, making this side a more common target than the sacral side for axSpA. The dorsal joint is mainly fibrous and essentially acts as a syndesmosis since the articulating surfaces are connected by an interosseous ligament.
SpA in the spine can occur either in vertebral body or nonvertebral body locations. Vertebral body lesions are further divided into: corner or essentially the entheses of the spinal ligaments; noncorner such as in vertebral body endplate; and lateral like the costovertebral joint. Nonvertebral body lesions or posterior element lesions are found in the facet joint; or elements with ligamentous or muscular attachments (transverse or spinous processes that may include the lamina; pedicle, facet processes, and pars interarticularis are excluded). ,
Axial Spondyloarthritis of the Spine
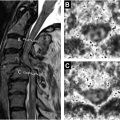
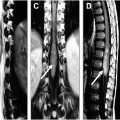
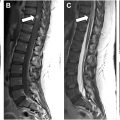
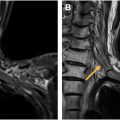
Spondylitis refers to inflammatory lesion of the vertebral body and is depicted as high SI in the anterior (Romanus lesion) ( Fig. 3 ) or posterior vertebral corners. , In axSpA, these lesions are usually well-defined and focal; whereas extensive and diffuse involvement frequently indicates other forms of SpA such as psoriatic arthritis. , These corner lesions may also be seen in degenerative or malignant spinal disease, although multiple lesions in younger patients are highly diagnostic of axSpA, irrespective of any other clinical or laboratory parameter. Involvement of more than 3 corners in the absence of osteophytes or Schmorl nodes is 81% specific for axSpA, which increases to 97% in patients younger than 40 years. Spondylitis of the cervical spine sparing the thoracic or lumbar spine or SI joints is also suggestive of other forms of SpA. , Spondylodiscitis or inflammatory Andersson lesion manifests with high SI at the cortical plates adjacent to intervertebral disks but not involving the corners ( Fig. 4 ). Costovertebral arthritis only applies to the thoracic spine and may be associated with BME extending to the pedicles ( Fig. 5 ), posterior aspects of the vertebral bodies, or adjacent ribs and soft tissues. Facet joint arthritis presents with BME in at least 1 facet of a facet joint and may be accompanied by erosions or facet joint effusion. Posterior element inflammatory lesion includes enthesitis of spinal ligaments (supraspinal, interspinal, and flaval) and costotransverse joint inflammation.



Chronic or structural lesions of the spine include erosion, focal fat, intradiscal T1-W signal, syndesmophyte, and ankylosis. A spinal erosion is similar to erosions elsewhere, appearing as a full-thickness loss of the dark appearance of cortical bone and loss of normal high SI of adjacent bone marrow on T1-W images. Focal fat on vertebral corners (fatty Romanus lesion) is frequently seen in the thoracic spine. More than 5 fatty Romanus lesions support a diagnosis of axSpA. Syndesmophyte, intradiscal T1-W signal, and ankylosis are examples of new bone formation in the disco-vertebral unit of the spine ( Fig. 6 ). Intradiscal T1-W signal is considered present when there is high SI on T1-W within the intervertebral disc on 2 consecutive slices; that measures half of the disc height and a quarter of the vertebra width on at least 1 slice. It has been hypothesized to represent early discal calcification, potentially a specific sign for axSpA. Syndesmophytes are thin, vertically oriented new bone formations on the peripheral aspects of discs, most often in a symmetric and bilateral distribution in the setting of axSpA. Conversely, thick, irregular bone formations at the vertebral corners are considered pseudosyndesmophytes and favor other forms of SpA, most commonly psoriatic arthritis. , , Syndesmophytes can either be bridging or nonbridging. Bridging syndesmophytes are considered the best predictors of radiographic progression; the appearance of just 1 syndesmophyte within 2 years indicates progression of structural changes in axSpA. In contrast to bridging syndesmophytes, the value of nonbridging syndesmophytes in the diagnosis of axSpA is currently unestablished. Ankylosis is high SI on T1-W that continues from 1 vertebra to the adjacent vertebra, either partially or completely. It may involve the anterior and posterior corners; vertebral endplate not involving either the anterior or posterior corner, essentially transdiscal ankylosis; and intervertebral synovial joints like the costovertebral, costotransverse, and facet joints. , Transdiscal ankylosis is more extensive than syndesmophytes ( Fig. 7 ). It is a specific marker of axSpA and indicates late disease or more extensive disease in younger patients. Literature on the MR imaging features of the intervertebral synovial joints are lacking likely because assessment requires coronal or axial slices, which are not typically obtained in standard axSpA MR imaging protocols. A few studies suggest that they are involved in the early stage of the disease. Apart from purely inflammatory and purely structural lesions, inflammatory changes superimposed upon structural lesions can be seen, or acute-on-chronic lesions. ,