This article examines the MR imaging features of the most common autoimmune inflammatory and demyelinating myelopathies, which encompass disorders characterized by inflammation and subsequent damage to the myelin sheath within the spinal cord. The diagnosis of these conditions relies on a comprehensive approach that includes clinical assessment, neuroradiological evaluation, and laboratory investigations. MR imaging is essential in identifying key features such as signal change, lesion dimension, gadolinium enhancement pattern, and temporal evolution, overall helping to narrow down the differential diagnosis in patients with myelopathy.
Key points
- •
Typical MRI features of transverse myelitis associated with MS include short-segment lesions mainly involving the cervical segment and the lateral and posterior columns.
- •
In AQP4-IgG NMOSD, characteristic imaging findings include longitudinally extensive lesions, bright spotty lesions and rostral extension of cervical lesions into the area postrema of the brainstem.
- •
In MOGAD distinguishing features include predominant involvement of the central gray matter, involvement of the conus medullaris, and resolution of lesions.
| ADEM | acute disseminated encephalomyelitis |
| AQP4-IgG NMOSD | aquaporin-4 immunoglobulin G-positive neuromyelitis optica spectrum disorder |
| CNS | central nervous system |
| LETM | longitudinally extensive transverse myelitis |
| MOG | myelin oligodendrocyte glycoprotein |
| MOGAD | myelin oligodendrocyte glycoprotein immunoglobulin G antibody-associated disease |
| MS | multiple sclerosis |
| STIR | short tau inversion recovery |
| T1W | T1-weighted |
| T2W | T2-weighted |
Introduction
Inflammatory and demyelinating myelopathies encompass a wide range of disorders characterized by inflammation and subsequent damage to the myelin sheath within the spinal cord. These disorders include myelopathies that are presumed to be immune-mediated but lack specific antibody markers, such as multiple sclerosis (MS), as well as autoimmune conditions characterized by identifiable pathogenic autoantibodies. Examples of the latter include aquaporin-4 immunoglobulin G-positive neuromyelitis optica spectrum disorder (AQP4-IgG NMOSD) and myelin oligodendrocyte glycoprotein (MOG) IgG-associated disease. ,
The clinical presentation of these immune-mediated myelopathies is highly variable, depending on the location and extent of lesions within the spinal cord. Symptoms can range from subtle signs, such as isolated Lhermitte’s phenomenon without accompanying sensory or motor deficits, to severe manifestations like quadriplegia with significant autonomic dysfunction, substantially impacting patients’ quality of life.
Diagnosis of these conditions relies on a combination of clinical assessment, neuroradiological evaluation, and laboratory investigations. MR imaging plays a crucial role in identifying characteristic features such as signal change distribution, lesion dimensions, gadolinium enhancement patterns, and temporal evolution, thereby helping to narrow down the differential diagnosis in patients presenting with myelopathy.
This article provides an up-to-date summary of the expected MR imaging findings in the most common inflammatory demyelinating myelopathies, highlighting its pivotal role in the intricate process of differential diagnosis within this diverse spectrum of disorders.
Multiple sclerosis
MS is a progressive autoimmune disease of the central nervous system (CNS), characterized by inflammation, demyelination, and neurodegeneration. It is the most common cause of nontraumatic neurologic disability among young adults. Globally, approximately 2.8 million people live with MS, with an estimated prevalence of over 100 cases per 100,000 people in North America and Europe.
Globally, females are 2 to 3 times more likely than males to develop MS, with some countries reporting a female-to-male ratio as high as 4:1. The disease typically presents in early to middle adulthood (between 20 and 40 years), while onset before age 18 and after age 50 is less common.
MS lesions can affect any area of the CNS, although they frequently show a predilection for specific regions, including the periventricular and juxtacortical white matter, the corpus callosum, the brainstem (notably the pons) and the cerebellum, as well as the optic nerves and the spinal cord. In fact, focal or diffuse spinal cord T2 signal abnormalities like those seen in the brain are detected in over 90% of MS patients.
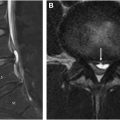
Spinal cord lesions in MS involve the cervical segment more frequently than the thoracic or lumbar segments. On sagittal images, they typically have a cigar shape, and rarely extend beyond 2 vertebral segments (short-segment myelitis). On axial images, these lesions appear wedge-shaped and usually affect the lateral and dorsal white matter columns, with or without involvement of the central gray matter ( Fig. 1 A–D). They rarely exclusively affect the anterior columns or the central cord, and seldom occupy more than half of its cross-sectional area, which may occur in the setting of acute lesions.

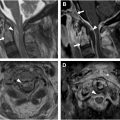
In some patients, particularly those with a progressive disease course, there may be mild diffuse T2 signal abnormality along extensive segments of the spinal cord ( Fig. 2 A). This diffuse pattern, more discernible on proton density (PD) and short tau inversion recovery (STIR) sequences, has not been incorporated into the current diagnostic criteria for MS due to concerns about its reliability and specificity.

The prevalence and characteristics of spinal cord lesions vary according to the clinical phenotype of MS. In relapsing-remitting MS, lesions are usually multiple and focal. In secondary progressive MS, lesions become more extensive and diffuse and are frequently associated with spinal cord atrophy. In primary progressive MS, spinal cord lesions are often more extensive than those seen in the brain.
Active spinal cord lesions in MS enhance less frequently than brain lesions. , When enhancement is present, it is typically short-lived (2–8 weeks, usually <4 weeks) and nodular, while ring-enhancement is less common. , Focal acute enhancing lesions in the spinal cord are often associated with new clinical symptoms and with concomitant enhancing brain lesions. Acute lesions may cause spinal cord swelling (tumefactive pattern), sometimes mimicking a spinal cord tumor ( Fig. 2 B–D).
Spinal cord MR imaging is essential at disease onset, even in patients without spinal cord symptoms, to support the diagnosis and predict the risk of disability progression. Additionally, MR imaging of the spinal cord can increase diagnostic certainty in patients with nonspecific brain MR imaging findings, as asymptomatic spinal cord lesions are relatively common in MS but rare in other white matter disorders, such as cerebrovascular disease, other autoimmune inflammatory disorders, age-related changes, or migraine-related focal white matter abnormalities.
Aquaporin-4 immunoglobulin G neuromyelitis optica spectrum disorder
AQP4-IgG NMOSD a rare chronic autoimmune inflammatory disease that severely affects the CNS, with an estimated annual incidence of 0.4 to 7.3 per million people. It predominantly affects middle-aged women, particularly those between 40 and 60 year old, with a female-to-male ratio of 9:1. This disease is rare before age 18 (<5% of total AQP4-NMOSD cases).
AQP4-IgG NMOSD is primarily characterized by severe episodes of optic neuritis, which can affect one or both eyes, and transverse myelitis. These attacks typically present as isolated syndromes but may occur simultaneously or in rapid succession.
Transverse myelitis is the most common presentation, occurring in approximately 50% of cases, typically involving the cervical or upper thoracic spinal cord, or both, while involvement of the conus is less common. Although less common, AQP4-IgG NMOSD can also involve the brainstem and brain, leading to symptoms such as nausea, hiccups, or acute neurogenic respiratory failure due to area postrema or diencephalic syndromes.
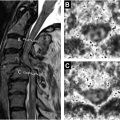
Approximately 85% of patients with AQP4-IgG NMOSD, who present with acute transverse myelitis, exhibit a single continuous hyperintense cord lesion on sagittal T2-weighted (T2W) or STIR sequences, referred to as longitudinally extensive transverse myelitis (LETM), and defined as a lesion extending cranio-caudally over 3 or more vertebrae ( Fig. 3 A, B). In contrast, LETM is extremely rare in MS and should prompt consideration of alternative etiologies. Occasionally, the coalescence of multiple short lesions in MS, along with the presence of hazy or diffuse T2-hyperintensity, can create the appearance of LETM, a phenomenon that mainly occurs in progressive MS phenotypes ( Fig. 4 A, B).


Spinal cord lesions in NMOSD are located centrally or both centrally and peripherally on axial images, generally affecting the entire or greater than 50% of the cord cross-sectional area, sometimes resulting in marked cord swelling that can mimic a neoplasm. , The predominant involvement of the central gray matter is due to this area’s high expression of the AQP4 antigen. ,
In severe cases, lesions can lead to cavitation and necrosis, often associated with T1-weighted (T1W) hypointensity of the gray matter, a condition known as pseudo-syringomyelia , (see Fig. 3 ).
Although the LETM pattern is characteristic of AQP4-IgG NMOSD, 7% to 14% of initial and 8% of subsequent myelitis attacks in AQP4-seropositive patients may present as short-segment lesions mimicking those seen in MS. These initial short-segment lesions evolve into LETM in more than 90% of cases. , , ( Fig. 5 A,B). Therefore, NMOSD should be considered in the differential diagnosis of patients presenting with short-segment lesions, and testing for AQP4-IgG status is recommended for accurate diagnosis, , even in the absence of other NMOSD features. These short-segment lesions in AQP4-IgG NMOSD, are preferentially located in the central gray matter and usually involve more than half of the cross-sectional area, indicating transversely extensive involvement. These short-segment lesions tend to be longitudinally longer than the typical spinal cord lesions seen in MS. Furthermore, LETM may evolve into multiple shorter lesions during remission or after treatment with steroids. , Therefore, the timing of spinal cord MR imaging in relation to the onset of symptoms is critical for identifying a characteristic LETM presentation.

A characteristic radiological finding in AQP4-IgG NMOSD is the so-called bright spotty lesion, defined as an area of higher T2-hyperintensity within the spinal cord lesion compared to the surrounding cerebrospinal fluid ( Fig. 6 A,B). These can be detected in approximately 50% of cases and likely reflect necrotic and microcystic changes in the spinal cord due to severe cord tissue damage. , This finding has shown a specificity of 94% and a sensitivity of 40% for AQP4-IgG NMOSD.

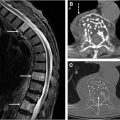
Contrast enhancement is present in most cases of acute LETM in AQP4-IgG NMOSD and can be detected for days to months following a relapse. Enhancement may appear as ring-like, elongated (lens-shaped), or patchy , ( Fig. 7 A–C). Leptomeningeal enhancement is also occasionally observed. , During remission, contrast-enhancing lesions may almost completely disappear. However, AQP4-IgG NMOSD can result in significant spinal cord atrophy, with or without associated T2W hyperintensity ( Fig. 8 A–C).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree