Evaluating pediatric nerve disorders is complex due to the small size of nerves and the intricacies of nerve anatomy. This article addresses key nerve pathologies in the pediatric population, focusing on both peripheral nerve and brachial plexus disorders. It discusses how MR imaging can classify and grade peripheral nerve injuries, assess the severity of nerve damage, and guide management decisions. Additionally, the article explores pediatric brachial plexus pathologies, highlighting MR neurography’s (MRN’s) ability to identify structural causes of thoracic outlet syndrome and classify brachial plexus birth injuries. As techniques continue to evolve, MRN’s ability to provide detailed visualization of structural nerve changes and associated muscle effects with enhanced diagnostic accuracy, will further inform treatment strategies for these complex pediatric conditions.
Key points
- •
Evaluating pediatric nerve disorders is challenging due to nerve size and complexity. MR neurography (MRN) is an evolving, non-invasive tool aiding diagnosis and management.
- •
MRN provides detailed visualization of structural nerve changes and associated muscle effects, essential for evaluating pediatric peripheral nerve and brachial plexus pathologies.
- •
Intravenous contrast in MRN is debated but may help in disrupted blood-nerve barriers, peripheral nerve tumors, neuromas, and post-operative cases.
- •
MRN is useful in diagnosing thoracic outlet syndrome by effectively identifying structural causes such as cervical ribs, bone anomalies, and nerve compression.
- •
MRN plays a key role in classifying the grade of peripheral nerve and brachial plexus birth injuries and helps guide management.
Introduction
Pediatric nerve disorders, encompassing a wide range of pathologies, pose unique challenges for diagnosis and management. Accurate imaging is critical for evaluating these conditions, as early intervention can significantly improve outcomes, particularly in the pediatric population, where development and recovery potential are of paramount importance. MR neurography (MRN) has developed into a highly effective noninvasive tool for assessing pediatric nerve pathologies, offering detailed visualization of structural nerve changes and associated downstream muscle effects. This article examines the role of MR imaging in the evaluation of pathologies affecting the peripheral nerves and brachial plexus in pediatric patients.
Clinical evaluation of nerve pathology
The initial evaluation of nerve pathology starts with a comprehensive history and physical examination. Electrodiagnostic studies, such as electromyography (EMG) and nerve conduction tests, provide valuable functional insights into nerve impairment. However, these studies require the insertion of a needle electrode, which may necessitate the use of anesthesia in young children. Imaging offers significant advantages as a noninvasive alternative, enabling direct visualization of nerve injuries, assessment of indirect effects on surrounding structures, and identification of lesions compressing the nerves. Imaging can also assist in detecting patterns of disease spread along the course of nerves. Even when a diagnosis is known, imaging may be required preoperatively to localize lesions or abnormalities and assist with surgical planning.
MRN and high-resolution ultrasound are key imaging modalities for assessing nerve pathology. While some experts recommend ultrasound as the initial imaging modality due to its higher sensitivity and similar specificity compared with MR imaging, each technique offers distinct strengths and limitations. MR imaging provides a global view of multiple nerves and surrounding structures, which is particularly advantageous for detecting subtle changes related to muscle denervation and neural edema, as well as for assessing the extent of nerve injuries. With MR imaging, evaluation of the surrounding structures for other causes of symptomatology is also possible, such as sports-related injuries. In contrast, ultrasound is often more accessible, quicker, and cost-effective but is limited in visualizing deeper structures and is highly operator-dependent. , Together, these modalities offer complementary insights for evaluating nerve pathology.
Nerve imaging is inherently challenging due to the small size and winding paths of nerves. In pediatric patients, MR imaging presents additional challenges, mainly due to the prolonged scan times that often necessitate sedation or general anesthesia to prevent motion artifacts. Certain nonpharmacological strategies, such as using mock scanners, preparatory videos, or child-friendly distractions, can help reduce the need for sedation during imaging, particularly in younger children.
MR neurography protocol
MRN is a specialized technique used to enhance visualization of nerves and their pathology. While MRN performed on a 3.0-T MR scanner is preferred over a 1.5-T MR scanner due to its higher signal-to-noise ratio, it is typically not essential. Although MRN protocols vary by institution, they generally include axial 2-dimensional (2D) T1-weighted (T1W), axial 2D T2-weighted (T2W) with fat suppression, and 3-dimensional (3D) T2W with fat suppression sequences with accompanying reformatted images in multiple planes. High-resolution T1W images, typically acquired in the axial plane are essential for anatomic evaluation including perineural fat and muscle bulk. Fluid sensitive sequences, including T2W fat-suppressed (FS) sequences or short-tau inversion recovery (STIR), are essential to detect neural edema and/or pathology. , T2 FS images are less affected by blood flow artifacts, whereas STIR images provide the most homogeneous fat suppression. A 3D T2W sequence with fat suppression is also frequently obtained, allowing for the creation of multiplanar reformatted images in multiple planes and maximum intensity projections (MIPs) to fully interrogate the nerve in question. Diffusion tensor imaging is an optional sequence that can be used to create 3D tractography of nerve fiber tracts, but postprocessing is required. This sequence can add functional information and may help detect acute traumatic nerve injuries that are otherwise difficult to assess macroscopically and can assist in monitoring nerve regeneration. ,
The role of intravenous contrast in MRN is variable, with no clear guidelines established in the literature. While some studies suggest that contrast does not significantly impact diagnostic interpretation, others indicate that it may be beneficial in MRN of the brachial plexus. Under normal conditions, peripheral nerves do not enhance with contrast if the blood-nerve barrier is intact. However, contrast may be useful when the blood-nerve barrier is disrupted, as in cases of neoplasms, infections, inflammatory diseases, or postradiation injury. As such, although its added diagnostic value remains debated, contrast may be helpful in evaluating peripheral nerve tumors, neuromas, atypical or diffuse polyneuropathy, and postoperative fluid collections. The lack of established criteria for using intravenous contrast in MRN highlights the need for consensus and evidence-based practice guidelines to determine standards for use of contrast.
Peripheral nerves
Anatomy
Peripheral nerves are organized into distinct layers in cross-section that provide both structural integrity and unique imaging characteristics. Individual nerve fibers, or axons, are surrounded by a thin endoneurium. These axons are grouped into bundles known as fascicles, protected by a thicker perineurium. The outermost layer, the epineurium, encases multiple fascicles, providing structural support and protecting the nerve as it travels through the body , ( Fig. 1 ).

MR Imaging Features
On T1W sequences, normal nerves display an intermediate to low-signal intensity, appearing isointense with surrounding muscle tissue. , The isointense fascicles within the nerve are distinguishable against the more hyperintense fatty connective tissue. The nerve is outlined by a hyperintense halo of epineural fat, enhancing its visibility on imaging. On T2W fat suppressed sequences, normal nerves are closer in signal to the surrounding tissues due to their intermediate signal. With neural edema, the fascicles become more hyperintense and visible. Normal nerves do not enhance after contrast administration due to the blood-nerve barrier.
Several key pathologic features can be detected on MR imaging, including nerve flattening in compression-prone areas, deviation from a normal nerve path, segmental areas of nerve enlargement, T2 hyperintensity, loss of fascicular architecture, and contrast enhancement on T1W sequences after gadolinium injection. Additionally, MR imaging can reveal indirect signs of nerve damage through changes in muscle. In the acute stage, T2 hyperintensity from muscle edema indicates denervation. In the chronic stage, muscle atrophy appears T1 hyperintense due to fatty infiltration. ,
Peripheral Nerve Injury
Peripheral nerve injuries often occur due to trauma, with the most common causes in pediatric patients being lacerations, falls, and motor vehicle accidents. While children have a significantly higher potential for recovery than adults, prompt diagnosis and treatment are essential to optimize nerve recovery and minimize long-term deficits. Evaluation of nerve injuries requires a combination of clinical assessment, electrodiagnostic studies, and imaging. MR imaging can be a powerful tool to help assess severity and classify the injury to direct management. ,
The most commonly used grading systems for peripheral nerve injury are the Seddon and Sunderland classifications. The Seddon classification, created in 1943, divides nerve injuries into neurapraxia, axonotmesis, and neurotmesis. In 1951, Sunderland expanded on this classification to categorize nerve injuries into 5° (I–V). Neurapraxia is the mildest form and corresponds to Sunderland grade I. It describes damage to the myelin sheath with intact axons and supporting sheaths. Axonotmesis is divided into the Sunderland grades II, III, and IV. In axonotmesis, the myelin sheath and axon are damaged. There remains a continuous nerve but with varying degrees of damage to the tissue sheaths. In Sunderland grade II, all 3 sheaths are intact, in Sunderland grade III the endoneurium is damaged, and in Sunderland grade IV the endoneurium and perineurium are damaged. In Sunderland grade IV, the intraneural scarring results in the formation of a neuroma; with the epineurium still intact, this forms a neuroma-in-continuity which is detectable on MRN and ultrasound. Lastly, neurotmesis corresponds to Sunderland V, in which all 3 sheaths are damaged and there is discontinuity of the nerve.
These classifications can be used to divide nerve injury into low grade (Sunderland I–III) and high grade (Sunderland IV–V) to help direct management. Low-grade injuries are generally managed nonoperatively while high-grade injuries require surgery for nerve regrowth. A Sunderland grade I injury typically recovers fully within 12 weeks while a Sunderland grade II injury may require several months for nerve regeneration. Sunderland grade III injuries has variable regrowth but should be differentiated from Sunderland grades IV and V which must undergo surgery to allow for regrowth.
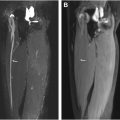
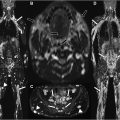
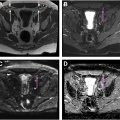
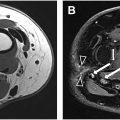
Although these classifications are clear in theory, distinguishing between them in practice can sometimes be challenging. Findings on MRN can be correlated to assist in classification and guide surgical decisions. Low-grade nerve injuries (Sunderland I–III) typically appear on MR imaging as T2 hyperintense nerves with variable enlargement ( Figs. 2 and 3 ). Sunderland grade IV injuries can be identified by bulbous enlargement with a loss of fascicular architecture while maintaining continuity and often with perineural fibrosis, all features that help distinguish these injuries from lower grade III injuries ( Fig. 4 ). Sunderland grade V represents a complete nerve transection, often with a proximal stump neuroma and a clear discontinuity in the nerve ( Fig. 5 ). A summary of these findings is presented in Table 1 .




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree