This review focuses on localized and whole-body MR imaging features for the more common benign peripheral nerve sheath tumors of schwannomas and neurofibromas compared with malignant peripheral nerve sheath tumors, including for sporadic tumors and tumors associated with neurofibromatosis syndromes. Additional less common tumors and tumor-like conditions associated with the peripheral nerves are reviewed for salient distinguishing features.
Key points
- •
Although there is overlap in the imaging of benign and malignant PNSTs, malignant PNSTs can be distinguished by their larger size, irregular shape, rapid growth, increased heterogeneity and exhibit restricted diffusion, characteristically with low ADC values (<1.0–1.1 × 10 −3 mm 2 /s), as well as perilesional edema and contrast enhancement.
- •
Patients with neurofibromatosis syndromes must be monitored for the development of malignancy. WB-MR imaging with WB-DWI avoids radiation exposure and is utilized to determine disease burden as well as characterization of detected tumors.
- •
There are several nonneurogenic tumors and nonneoplastic conditions that can mimic PNSTs that radiologists should be aware of.
| ADC | apparent diffusion coefficient |
| CPN | common peroneal nerve |
| CT | computed tomography |
| DWI | diffusion-weighted imaging |
| FS | fat-suppressed |
| MPNSTs | malignant peripheral nerve sheath tumors |
| MPR | multiplanar reconstruction |
| NF | neurofibromatosis |
| NF1 | neurofibromatosis type 1 |
| PNSTs | peripheral nerve sheath tumors |
| SWN | schwannomatosis |
| T1W | T1-weighted |
| T2W | T2-weighted |
Introduction
While patients with benign soft tissue masses present to their physicians about 100 times more frequently than those with malignant soft tissue masses, the imaging features of benign and malignant tumors overlap. Of the soft tissue masses that are benign, benign peripheral nerve sheath tumors (PNSTs) account for 10% to 12% of cases, and the vast majority of these are schwannomas and neurofibromas. Genetic conditions such neurofibromatosis type 1 (NF1), schwannomatosis (SWN) and neurofibromatosis type 2 (now reclassified as a form of SWN) are syndromes that predispose patients to developing benign PNSTs throughout the body. Aside from neurofibromas and schwannomas, less commonly encountered masses associated with peripheral nerves include hybrid lesions, perineuromas, ganglioneuromas, and fibrolipomatous hamartomas, as well as various nonneoplastic conditions (traumatic neuromas, Morton’s neuromas, and nerve sheath ganglions).
Malignant peripheral nerve sheath tumors (MPNSTs) are much less prevalent, with approximately half of MPNSTs occurring in patients who have NF1, for whom there is a 10% lifetime risk of developing MPNST. Otherwise, about half of MPNSTs that are encountered occur sporadically. There is overlap in the histologic features of benign PNSTs (schwannomas and neurofibromas specifically) and MPNSTs occurring sporadically, although there are some imaging characteristics that help differentiate these entities that will be discussed later. In patients with NF1, there is a specific histologic classification system that describes the progression from a benign neurofibroma through atypical and intermediate grade lesions to the formation of MPNST ; at this time, imaging correlates to this histologic progression in NF1 have not been fully established, but there are imaging features that can detect malignant degeneration with high accuracy. ,
Magnetic resonance (MR) imaging is the best noninvasive method for evaluating PNSTs. , According to Demehri and colleagues, functional MR imaging techniques, particularly diffusion-weighted imaging (DWI) with apparent diffusion coefficient (ADC) mapping, have improved the ability to assess tumor cellularity and help in distinguishing between benign and malignant masses. , , Metabolic imaging with MR imaging (proton magnetic resonance spectroscopy) has also shown utility in classifying PNSTs as benign or malignant but is not routinely used clinically. Localized MR imaging is critical for tumor characterization and defining tumor extent, while in patients with NF syndromes, whole body MR imaging has become the standard of care at many centers, for the evaluation of tumor burden throughout the body and detection of malignant degeneration. Other whole body imaging modalities, such as computed tomography (CT) and PET, are also used for evaluating tumor burden and metabolic activity at centers where whole body MR imaging is not as widely available, but PET imparts radiation that is otherwise avoided by MR imaging. Another option for whole body imaging when possible is integrated PET/MR imaging, unique in its ability to provide an anatomic, functional, and metabolic evaluation in a single session while reducing radiation exposure and has been used particularly in pediatric oncology.
In this study, the clinical presentation and imaging features of benign and malignant PNSTs will be discussed. This review will focus on localized and whole-body MR imaging features for the more common benign PNSTs of schwannomas and neurofibromas compared with MPNSTs. Additional less common PNSTs will be reviewed for salient distinguishing features.
Clinical presentation
Patients with PNSTs may present with a palpable mass and pain, as well as sensory symptoms such as numbness or tingling. The Tinel’s sign may be a useful sign of a tumor that is associated with a peripheral nerve. In addition, there may be loss of nerve function downstream, including weakness if a motor branch is involved. Not every patient with a PNST experiences pain related to the tumor, and benign PNSTs can be asymptomatic or incidental. The presence of pain related to a PNST can potentially be a sign of MPNST, but the development of pain in a benign PNST is also encountered and poorly understood.
Evaluation of an isolated peripheral nerve sheath tumor
For the diagnostic approach to evaluating PNSTs, the first important question is to decide whether a soft tissue mass is associated with a peripheral nerve, suggesting a PNST may be present. While ultrasound can be used to evaluate soft tissue masses, localized MR imaging offers a more comprehensive assessment with multisequence features for characterization and defining tumor extent. The tail sign describes the feature that suggests neurogenic origin, with the tumor in direct continuity with a nerve into and/or out of the mass. If, by imaging, a tumor appears to arise from a peripheral nerve, the next decision point is to characterize the lesion as benign or malignant, with benign tumors being much more common. As stated, schwannomas and neurofibromas are the most common sporadic benign PNSTs and distinguishing between these 2 entities can have important surgical implications: Schwannomas are eccentric tumors that grow in the epineurium and are often encapsulated for easier surgical excision. However, neurofibromas arise in the nerve fascicle and are typically centrally located, making them more difficult to resect and separate from the parent nerve, with the potential for greater morbidity. Therefore, identifying the relationship of the tumor to the nerve fascicles could provide critical information to planning surgical removal. Unfortunately, routine MR imaging features are not reliable for making the necessary distinctions, especially in small tumors or tumors that involve small nerves. High-resolution MR imaging with diffusion tractography has been reported as a valuable method for visualizing the relationship of a tumor to the parent nerve fascicles, although this technique is cumbersome and not used in routine clinical practice preoperatively. High-resolution ultrasound for superficial tumors has reportedly been used intraoperatively, but routine ultrasound is not reliable for distinguishing neurofibromas from schwannomas.
MR Imaging Features for Distinguishing Benign Neurofibromas, Schwannomas, and Malignant Peripheral Nerve Sheath Tumors
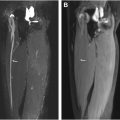
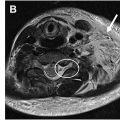
For distinguishing benign and malignant PNSTs, there are multiple primary MR imaging features that can be used, and the secondary findings related to muscle denervation should be described in the radiology report. Figs. 1 and 2 show features of a benign PNST compared with an MPNST, respectively. By conventional MR imaging (performed with T1-weighted, fluid-sensitive, and postcontrast T1-weighted sequences), important characteristics that can be ascertained include defining the size and shape of the tumor, the signal intensity with degree of heterogeneity and internal architecture, and the perilesional characteristics ( Table 1 ). First, MPNSTs are typically larger than benign PNSTs and have a more irregular lobular shape compared to benign PNSTs that are often smaller and exhibit a fusiform smooth shape. However, some benign tumors can grow to very large sizes, especially in the setting of NF syndromes and size by itself is not a reliable differentiating feature of malignancy. ,


| Primary Signs | Utility |
|---|---|
| Size | Benign PNSTs can be large, but MPNSTs are typically larger in size |
| Shape | Benign PNSTs exhibit a smooth fusiform shape while MPNSTs are typically more lobular and irregular |
| Location along the nerve | Schwannomas and MPNST are often eccentric appearing while neurofibromas appear more central, but these are not reliable differentiating features |
| Signal intensity and heterogeneity | Both benign PNSTs and MPNSTs are T2 hyperintense but MPNSTs are usually more heterogeneous on all sequences, including postcontrast T1-weighted imaging with internal cystic/necrotic regions |
| Split fat sign | Associated with PNSTs, benign or malignant, but can be associated with other tumors |
| Target sign | More frequently observed in benign PNSTs and absence of a target sign may suggest an MPNST, but some MPNSTs exhibit a target sign |
| Perilesional edema and contrast enhancement | Presence is more likely to signify MPNST |
| ADC values | Low ADC values (<1.0 × 10 −3 mm 2 /s) are concerning for MPNST and differentiate neurofibroma from MPNST in NF1. Schwannomas (especially ancient schwannomas) sometimes exhibit low ADC values |
| Presence of early arterial enhancement | Present in MPNST, absent in neurofibroma Sometimes present in cellular schwannomas |
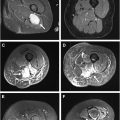
One of the most widely known features of a PNST is the target sign. This sign refers to the differential signal within a PNST that corresponds with differences in cellularity either between the Antoni A and B zones or between collagenous stroma and surrounding myxomatous tissue. , The sign refers to the presence of a central low intensity region encircled by a high-intensity rim by T2-weighted imaging and can be seen with benign neurofibromas as well as schwannomas and rarely, also in MPNSTs. The absence of a target sign, along with other features could herald the presence of an MPNST. Otherwise, the MR imaging signal of benign PNSTs reflects the internal composition, tending to be more homogeneous in signal compared to MPNSTs that exhibit internal cystic, necrotic, or hemorrhagic areas and tend to be much more heterogeneous. Following contrast administration, the enhancement of an MPNST is often heterogeneous and avid, with early arterial enhancement by dynamic contrast-enhanced MR imaging while a typical benign PNST enhances more homogeneously or, depending on the myxoid content, very little.
Perilesional characteristics are also a useful sign of malignancy. Perilesional edema and enhancement following contrast administration are features associated with MPNST. Furthermore, perilesional contrast enhancement, in general, is more likely to be associated with a high-grade sarcoma. A “split-fat” sign has been described as a feature of benign PNSTs embodied by lipid signal (high T1 signal) at the proximal and distal portions of the tumor, but is not a specific sign for PNSTs, as other tumors can exhibit this feature.
The capacity to distinguish between benign and malignant PNSTs has improved with the advent of DWI and ADC mapping, a technique that offers insight into a tumor’s cellularity. Because of the restricted diffusion associated with increased cellularity, MPNSTs frequently have lower ADC values, setting them apart from their benign counterparts, with ADC less than 1.0 × 10 to 3 mm 2 /s). ,
Despite all the features described earlier that are certainly useful for identifying an MPNST and differentiating it from a benign neurofibroma, some schwannomas (ancient schwannomas) can exhibit similar features to an MPNST with large growth, irregular and eccentric morphology, heterogeneous signal and enhancement as well as perilesional edema and enhancement with low ADC values. As such, the features described are highly sensitive for MPNST but are not necessarily specific when differentiating MPNST from a cellular or ancient schwannoma.
Benign Peripheral Nerve Sheath Tumors Other than Schwannomas and Neurofibromas
Hybrid lesions
Hybrid tumors are benign tumors of the peripheral nerve sheath that exhibit characteristics of multiple benign PNST types, including neurofibroma, schwannoma, and perineurioma. Schwannoma/perineurioma combinations, which occur infrequently, and neurofibroma/schwannoma combinations, which are commonly linked to SWN or neurofibromatosis (NF) type 1 or 2, are the most prevalent types of hybrid lesions. Rarely, neurofibroma/perineurioma combinations occur, and they are typically linked to NF1. These are benign lesions that can be excised although in rare instances, local recurrence has been reported. In hybrid PNSTs, malignant transformation has been reported in at least 2 recent case reports. MR imaging features of these lesions vary and include a fascicular sign with entering and exiting nerve signs, a target sign typical of a benign entity as well as a split fat sign when occurring in intermuscular locations; features can also include a lobulated shape and ancient change (cystic degeneration) that indicates chronicity.
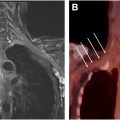
Perineuromas
The term “perineuroma” refers to a rare type of benign PNST that is made up of a localized proliferation of perineural cells in whorls surrounding nerve fibers. According to their relationship to the histologic boundaries of the nerve from which they originate, these benign tumors have historically been subclassified as either intraneural perineuriomas or extraneural (soft tissue) perineuriomas. There are also other histologic variants, such as sclerosing, plexiform, granular, and reticular perineuriomas. Clinically, intraneural perineuriomas typically manifest in young adults with motor or sensory mononeuropathy that progresses slowly, while extraneural soft tissue perineuriomas have a better prognosis and typically manifest as a painless tumor in midadulthood. Intraneural perineuromas most commonly involve the sciatic nerve and in approximately one-sixth of cases, more than one nerve is involved; they appear as lengthy fusiform nerve enlargement with a fascicular architecture and demonstrate substantial enhancement following intravenous contrast administration, as shown in Fig. 3 . Extraneural perineuromas appear as ovoid, spherical, or unencapsulated lesions with areas of heterogeneity on T2 weighted MR imaging and contrast administration.