The brachial plexus is a network of nerves responsible for the motor and sensory innervation of the upper extremity and upper chest. Pathologies affecting this structure can lead to significant morbidity, ranging from pain and sensory deficits to profound motor impairment. MR imaging is the modality of choice for imaging the brachial plexus. This review provides an overview of brachial plexus imaging, emphasizing practical aspects, anatomic landmarks, and imaging protocols, as well as a wide range of pathologies ranging from traumatic injury to inflammatory, idiopathic, hypertrophic, and neoplastic conditions.
Key points
- •
MRI is the preferred modality for brachial plexus evaluation due to high resolution, multiplanar imaging, and superior soft tissue contrast.
- •
Brachial plexus trauma causes pre- or postganglionic injury. Classification by severity or location helps identify patients who may benefit from conservative treatment or surgical intervention.
- •
Schwannomas and neurofibromas are the most common primary brachial plexus tumors, but secondary neoplasms, spreading via direct extension or metastasis, are more frequently encountered.
- •
Viral and vector-borne bacterial infections of the BP are often classified as Parsonage-Turner syndrome, typically presenting with a characteristic history and prodrome.
- •
Radiation-induced plexopathy, the most common non-traumatic plexopathy, often occurs after radiation therapy for apical lung, breast, or head and neck cancers.
| 2 D | 2 dimensional |
| 3D | 3 dimensional |
| BP | brachial plexus |
| CIDP | chronic inflammatory demyelinating polyneuropathy |
| CMT | Charcot-Marie-Tooth disease |
| COVID-19 | coronavirus disease 2019 |
| CT | computed tomography |
| DTI | diffusion tensor imaging |
| EMG | electromyography |
| MPNST | malignant PNST |
| NCS | nerve conduction studies |
| NF | neurofibromatosis |
| PNSTs | peripheral nerve sheath tumors |
| SSFP | steady-state free precession |
| STIR | short-tau inversion recovery |
| T1WI | T1-weighted images |
| T2WI | T2-weighted images |
| TBPI | traumatic brachial plexus injury |
Introduction
The brachial plexus (BP) is a network of nerves responsible for the motor and sensory innervation of the upper extremity and upper chest. Pathologies affecting this structure can lead to significant morbidity, ranging from pain and sensory deficits to profound motor impairment. A thorough understanding of the anatomy, pathology, and imaging techniques is essential for accurate diagnosis and management. MR imaging is the modality of choice for imaging the BP.
Normal anatomy
The BP typically arises from the ventral rami of the C5, C6, C7, C8, and T1 spinal nerves as they exit the neural foramina. , The BP consists of 5 ventral rami of spinal nerves, 3 trunks, 6 divisions, 3 cords, and 5 terminal branches ( Figs. 1 and 2 ). These segments are often remembered using the mnemonic “Radiology Technologists Drink Cold Beverages” or the variation “Some Technologists Don’t Carry Beepers,” which uses the correct terminology for spinal nerves instead of “roots.” ,


Normal anatomic variants are present in up to 50% of the population, with the most common being the course of C5 to C6 anterior to the scalene muscle. , Other variations, such as a prefixed (C4–C8) or postfixed (C6–T2) plexus, should also be recognized to avoid misinterpretation. These clinically significant variations may influence predisposition to certain pathologies and impact surgical planning.
Anatomically, as well as on imaging, the BP can be divided into 3 key sections: supraclavicular, retroclavicular, and infraclavicular. Important anatomic and imaging landmarks define these sections as described in Table 1 .
| Sections | Segments | Anatomical Landmarks |
|---|---|---|
| Supraclavicular | Spinal nerves (roots) | The ventral rami of the spinal nerves pass through the interscalene triangle after exiting the neural foramen . This triangle is formed by the anterior and middle scalene muscles and is bounded inferiorly by the first rib |
| Trunks |
| |
| Retroclavicular | Divisions |
|
| Infraclavicular | Cords |
|
| Terminal branches |
|
Diagnostic tools
Various diagnostic tools can be used to assess BP abnormalities, both invasive and noninvasive. Initial examination may include a radiograph to provide an overview of the spine, shoulder, and chest, allowing the detection of abnormalities such as a cervical rib, elongated C7 transverse process, or tumors like Pancoast.
Ultrasound allows for dynamic assessment of the different segments of the BP during various neck and shoulder movements, and can be used as a guide for treatment options. Computed tomography (CT) is useful for evaluating osseous structures, particularly in cases of trauma or neoplastic bone involvement. CT angiography can be tailored for assessing thoracic outlet syndrome, while CT myelography can aid in evaluating preganglionic injuries in trauma. , ,
However, MR imaging is the preferred imaging modality for BP evaluation due to its high resolution, multiplanar capabilities, and superior visualization of soft tissues, nerves, and muscles. It enables detailed assessment of abnormalities from the spinal cord and intradural rootlets to the spinal nerves and terminal branches. , On MR imaging, the different segments of the BP are isointense to muscle on T1-weighted images (T1WI) and isointense to slightly hyperintense compared to muscle on T2-weighted images (T2WI; see Fig. 2 ). It is always important to compare the BP to the contralateral side, as they should be symmetric.
Advanced techniques, including MR neurography and diffusion tensor imaging (DTI), provide improved visualization of nerve integrity and microstructure. , , DTI, in particular, enables 3 dimensional (3D) reconstruction of nerve fibers by analyzing water diffusion in multiple directions. Additionally, artificial intelligence is showing promise in automating segmentation and improving diagnostic accuracy. ,
Electrophysiologic testing, including nerve conduction studies (NCS) and electromyography (EMG), is used to confirm the diagnosis, localize the lesion level, and assess the severity of axon loss.
MR imaging technique and protocol
MR imaging of the BP provides high spatial resolution of small anatomic structures in the head and neck region. Imaging protocols for the BP should be customized according to the clinical suspicion to optimize diagnostic accuracy. It can be performed on both 1.5 Tesla (1.5 T) and 3T scanners, with a combination of 2 dimensional (2D) and 3D sequences. , While 2D sequences offer superior in-plane resolution and faster acquisition times, 3D isotropic sequences allow for multiplanar reconstructions and detailed visualization of nerve pathways. The use of flexible surface coils or custom coil arrays ensures optimal coverage of the BP. , However, dedicated high-resolution multichannel phased array surface coils are preferred. Imaging protocol for BP MR imaging can vary between institutions due to differences in equipment, software capabilities, and specific clinical requirements ( Table 2 ).
| Primary Sequences | FOV (∼mm) | Slice Thickness (mm) a | TR | TE | Flip Angle |
|---|---|---|---|---|---|
| Coronal T2W high resolution, with multiplanar oblique reformats | Shoulder to shoulder Oblique axial , sagittal and coronal on the affected side | 1 | 3800 | 191 | 120 |
| Coronal STIR FSE | Shoulder to shoulder | 1–2 | 3800 | 195 | 120 |
| Coronal T1WI TSE 2D | Shoulder to shoulder | 3–4 | 643 | 13 | 160 |
| Sagittal oblique T1WI TSE | Affected side (220–280) | 3–4 | 730 | 12 | 130 |
| If contrast required, multiplanar T1WI fat-suppressed sequences are obtained after contrast administration. Of note, coronal should cover shoulder to shoulder, and oblique reformats the affected side | |||||
For imaging planning, axial oblique and coronal oblique images are preferred, with coronal and sagittal planes optimally oriented orthogonally to the neurovascular bundle. , This also helps reduce motion artifacts, as the heart and lungs are avoided.
T1W non–fat-suppressed sequences are valuable for visualizing nerves within perineural fat. T2W fat-suppressed sequences help detect nerve abnormalities, muscular edema, and soft tissue changes and are useful to distinguish tumors and other pathologic processes. Short-tau inversion recovery (STIR) is a reliable method for fat suppression across scanners but has drawbacks like low signal-to-noise ratio, pulsation artifacts, and enhanced nerve signal. Spectral adiabatic inversion recovery offers a viable alternative when available. Intravenous contrast material should not be routinely used and should be reserved for specific cases, such as neoplastic conditions or infectious plexitis. If administered, T1W fat-suppressed sequences should be obtained.
Brachial plexus pathology
The BP can be affected by a variety of pathologic conditions, which can be broadly divided into 2 major categories: traumatic and nontraumatic brachial plexopathies. MR imaging plays a critical role in evaluating these pathologies, providing detailed visualization of structural changes and facilitating both diagnosis and treatment planning.
Traumatic Brachial Plexus Injury
Adult traumatic brachial plexus injury (TBPI) results in functional deficits and debilitating pain and may have mental health implications and significant economic impact. The annual incidence of TBPI worldwide ranges from 0.17 to 1.6 per 100,000. , These injuries most frequently occur in young adult male individuals who are involved in traffic accidents. , Classifying TBPI helps identify patients who may benefit from conservative or surgical treatment.
Lesion Severity
TBPI is traditionally categorized using the Seddon and Sunderland classifications ( Table 3 ). , According to the Seddon classification, the mildest nerve injury type is neurapraxia. This condition involves a temporary block in the conduction of nerve impulses, which typically resolves on its own. On the other hand, axonotmesis refers to damage to the axon and the supporting connective tissue framework, although these structures remain partially or fully intact. The likelihood of spontaneous recovery in cases of axonotmesis depends on the extent of the damage (see Table 3 ). Neurotmesis is the most severe type of nerve injury, characterized by a complete disruption of the nerve and its connective tissue components. This type of injury usually requires surgical intervention. Sunderland further developed Seddon’s classification of nerve injuries by dividing them into 5 categories based on the number of compromised connective tissue layers (see Table 3 ).
| Anatomical Structure | Injury | Classification of Injury Seddon Sunderland | Management | |
|---|---|---|---|---|
| Axon | Focal segmental demyelination | Neuropraxia (“praxis” means “nonaction”) | Grade I | Conservative |
| Axon + connective tissue (lesion in continuity) | Axon damaged with intact endoneurium | Axonotmesis (“tmesis” means “cutting”) | Grade II | Conservative |
| Axon + endoneurium damaged with intact perineurium | Axonotmesis | Grade III | Conservative | |
| Axon + endoneurium + perineurium damaged with intact epineurium | Axonotmesis | Grade IV | Nerve reconstruction | |
| Axon + connective tissue + anatomic nerve division | Complete nerve transection | Neurotmesis | Grade V | Nerve reconstruction |
Lesion Location
Based on the dorsal root ganglion, the BP can be categorized into preganglionic and postganglionic segments. A preganglionic injury occurs when nerve rootlets are avulsed from the spinal cord or when there is a rupture in the preganglionic root zone. This severe type of injury typically affects the lower C8 to T1 nerve roots. Spontaneous nerve recovery is not possible in cases of preganglionic injuries, which necessitate surgical intervention.
Postganglionic injuries are further divided into supraclavicular and infraclavicular injuries. Supraclavicular injuries involving the roots, trunks, or divisions are typically associated with high-energy trauma. Compared to infraclavicular injuries, supraclavicular injuries are generally more severe, are more likely to require surgical nerve repair, and are associated with a worse prognosis. In contrast, infraclavicular injuries, affecting the cords and terminal branches, typically do not require surgery. They most commonly involve the C5 to C7 nerve roots and are often associated with other injuries, such as anterior shoulder dislocation or vascular dissection. ,
Mechanism of Injury
TBPI is often linked to high-energy blunt trauma resulting from falls from heights, motor vehicle accidents, and sports injuries. In certain populations, low-energy or gunshot wounds are significant injury mechanisms.
Imaging Assessment
MR imaging is the imaging method of choice for evaluating the BP as it facilitates surgical planning and patient prognostication. The imaging findings depend on the location of injury and time elapsed after injury onset. CT myelography serves as an alternative imaging method when MR imaging is not available or when MR imaging findings are unclear and is specifically limited to assessing preganglionic TBPI.
Preganglionic injury
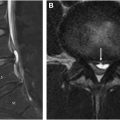
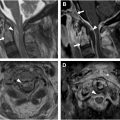
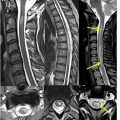
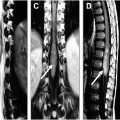
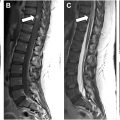
MR imaging may reveal discontinuity of the ventral or dorsal nerve rootlets from the spinal cord ( Fig. 3 ), indicating root avulsion, localized cord edema, and the presence of subarachnoid hemorrhage. , , Secondary imaging findings include the presence of a pseudomeningocele, a cerebrospinal fluid-filled nerve root sleeve with a cystic appearance, thickening of the dura matter (known as the black line sign), edema in the ipsilateral paraspinal muscles suggestive of denervation myopathy, and lateral displacement of the cord toward the side of injury due to scarring (see Fig. 3 ; Fig. 4 ). , MR imaging is most accurate for the detection of preganglionic injury when performed 3 to 4 weeks after the injury. This timing allows for the resolution of edema and hemorrhage and for the development of secondary imaging findings, such as pseudomeningocele. Of note, up to 23% of root avulsions do not have an associated pseudomeningocele.



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree