MR imaging is a useful tool in establishing the diagnosis of inflammation and/or infection in the hip joint and adjacent tissues, and in determining the extent of disease. In conjunction with clinical factors, MR imaging findings can help to narrow the differential diagnosis in individual cases and can guide decisions regarding biopsies, aspirations, or additional imaging.
Key points
- •
Joint effusions and synovial thickening are hallmarks of infectious synovitis but are also found in non-infectious joint processes.
- •
MR imaging findings of muscle edema may signify a variety of unrelated disorders such as infection, autoimmune processes, ischemic myopathy, or reactive edema.
- •
Post-operative inflammation or infection may be seen following hip arthroplasties or cosmetic procedures such as gluteoplasty.
Introduction
Infection and/or inflammation can occur at any age and in any part of the musculoskeletal system. Infection is caused by entry of pathogens into musculoskeletal tissues resulting in abscesses, myositis, fasciitis, osteomyelitis, and septic arthritis. Inflammation, a complex defensive response to tissue injury can be caused by infection, chemical toxins, thermal injuries, trauma, and tissue ischemia. This article will focus on the role of MR imaging in the diagnosis of inflammatory and infectious conditions affecting the hip. We will present 2 broad categories of inflammation and infection, those in bone and joint, and those in soft tissues, knowing that there is often overlap between these categories. We will include a few entities that can be mistaken for infection or inflammation.
MR imaging protocols
Routine MR imaging protocols are generally sufficient for visualizing inflammatory and infectious processes around the hip. T1-weighted (T1W) sequences are essential in evaluating bone marrow and muscle atrophy, while fat-suppressed (FS) water sensitive imaging, most commonly short tau inversion recovery (STIR) or T2-weighted (T2W) FS sequences, are effective in demonstrating tissue edema and edema-like signal, joint effusions, bursal distention, and soft tissue collections. Advanced techniques such as chemical shift imaging, diffusion-weighted imaging, perfusion imaging, Dixon-based T2W imaging, and MR neurography can also be used. Administration of gadolinium, while not required for the diagnosis of osteomyelitis, is helpful in delineating synovial thickening and abscesses. Sequences including a large field of view should be included to view the entire pelvis, or at least the affected hemipelvis, as the sacroiliac joints are often the sites of inflammation or infection presenting with hip symptoms.
Osteoarticular infection and inflammation
Infectious Synovitis (Septic Arthritis) and Osteomyelitis
Septic arthritis and osteomyelitis of the hip are most commonly due to Staphylococcus aureus ; other causative organisms include Streptococcus pneumonia , Neisseria gonorrhea , Salmonella (predominantly seen in sickle cell anemia), and Pseudomonas . The synovium in joints is highly vascularized and is susceptible to hematogenous seeding, but septic arthritis can also be caused by spread from adjacent osteomyelitis or penetrating injuries. Osteomyelitis around the hip can be caused by direct extension from an infected joint or ulcer, penetrating trauma or hematogenous spread.
Bacterial septic arthritis is considered an urgent or emergent situation as the infection can rapidly destroy cartilage and lead to osteomyelitis. Aspiration of the joint yields valuable information including cell count; gram stains, and aerobic or anaerobic cultures may reveal the causative organism. However, an effusion may not be visible in cases where the joint has decompressed into adjacent soft tissues. If fluid cannot be aspirated, lavage can be performed for cultures. Along with the bacterial cultures, aspirate or lavage fluid should be sent for mycobacterium and fungal cultures.
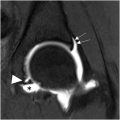
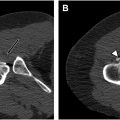
MR imaging findings in septic arthritis of the hip include joint effusion and synovial thickening , ; contrast can help to better evaluate the degree of synovial thickening and nodularity. Reactive bone marrow edema may be present, but geographic low signal on T1W images is suggestive of osteomyelitis ( Fig. 1 ). Spread of hip joint infection to the retroperitoneum occurs readily via the iliopsoas bursa, leading to inflammation ( Fig. 2 ), phlegmon, or abscess formation ( Fig. 3 ). Attention to the ipsilateral sacroiliac joint is important as septic arthritis of this joint may present with hip pain ( Fig. 4 ).




Joint infection caused by mycobacterium tuberculosis is less common and more indolent than bacterial septic arthritis but left unrecognized can eventually lead to joint destruction. The infection usually occurs via hematogenous seeding of the adjacent bone from a remote site (such as lung) with subsequent penetration into the joint. Direct hematogenous spread to synovium is less frequent. While identification of the causative organism either by culture or synovial biopsy is essential for establishing the diagnosis of tuberculous arthritis, MR imaging has been found to be helpful and distinguishing tuberculous joint and adjacent soft tissue involvement from that of pyogenic organisms. In particular, extension into the soft tissues from the joint may occur with formation of cold abscesses, which do not show prominent adjacent inflammation; the walls of these abscesses may be thin and smooth as opposed to pyogenic abscesses that tend to show thick irregular walls. , Calcifications in abscesses are highly suggestive of tuberculosis ( Fig. 5 ).

Autoimmune Inflammatory Arthritis
Autoimmune inflammatory arthritis is a broad category of arthritis with rheumatoid arthritis being most common. The group also includes juvenile idiopathic arthritis and seronegative spondyloarthropathies. Inflammatory arthritis can be seen in other rheumatic and autoimmune diseases such as systemic lupus erythematosus, systemic sclerosis, Sjogren syndrome, mixed connective tissue disorders, and others, and may also be found in association with underlying malignancies. MR imaging can be a useful tool in the diagnosis and evaluation of autoimmune inflammatory arthropathies as it is more sensitive than plain films in evaluating early synovitis. , Typical findings in more advanced rheumatoid arthritis include visualization of thick synovial pannus, bone erosions, and joint fluid ( Fig. 6 ).

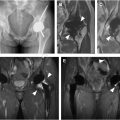
In most cases of seronegative spondyloarthropathies, sacroiliac joints are involved. The diagnosis of active sacroiliitis can be made when subchondral bone marrow edema is seen ; erosive disease is also demonstrated by MR imaging ( Fig. 7 ). Detection of enthesitis is important in seronegative spondyloarthropathies, seen as high signal on water sensitive MR imaging sequences at tendon and ligament attachments to bone ( Fig. 8 ). MR imaging diffusion-weighted imaging or assessment with contrast may be helpful in assessing treatment efficacy in ankylosing spondylitis.


Osteoarthritis and Rapidly Destructive Hip Osteoarthritis
Traditionally, osteoarthritis has been classified as a non-inflammatory arthritis since decades ago, the inflammatory markers found in osteoarthritis, such as leukocyte counts in joint fluid, were lower than those in rheumatoid arthritis, seronegative arthritis, and infectious synovitis. However, there has been increasing recognition of synovitis in osteoarthritis, and inflammation has been appreciated as a component of the development of osteoarthritis in some patients ( Fig. 9 ).

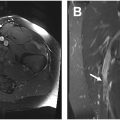
Rapidly destructive hip osteoarthritis (RDO) is a subset of osteoarthritis typically affecting older females in whom severe symptoms develop in a strikingly short period of time, often in months, with an average of 1.4 years. MR findings in RDO include joint effusions, synovitis, and bone marrow edema-like signal in the femoral head, femoral head flattening, subchondral cystic-appearing lesions, and linear subchondral foci suggestive of subchondral fractures. , Osteophytes may be too small to recognize on MR imaging but are found on histology. RDO is diagnosed only after exclusion of other entities that cause rapid hip destruction such as septic arthritis, autoimmune arthritis, and neuropathic disease.
Depositional Arthropathies
Crystalline arthropathies
Crystal-related arthropathies occur following crystal deposition in joints and periarticular soft tissues with a resultant inflammatory response. , The most common crystals involved are monosodium urate, calcium pyrophosphate dihydrate, and basic calcium phosphate including carbonated hydroxyapatite. Crystals within the hip joint may be identified in aspirated hip fluid and should be considered in the differential diagnosis of suspected septic arthritis. Extra-articular crystal deposition is thought to be one of the many factors that may contribute to greater trochanteric pain syndrome. On hip MR imaging, a low signal focus or foci may be seen with surrounding high signal around the gluteal tendons or trochanteric bursa ( Fig. 10 ).

Amyloidosis
Amyloid deposition occurs in association with dialysis, multiple myeloma, and various chronic inflammatory diseases.
Dialysis-related amyloidosis occurs in patients with end stage renal disease on long-term dialysis. This form of amyloidosis primarily involves the musculoskeletal system, causing deposition of β2-microglobulin in synovium resulting in destructive arthropathies, destructive spondyloarthropathy, and carpal tunnel syndrome. The hips are common sites of involvement. The clinical presentation may be mistaken for osteoarthritis or inflammatory arthropathies such as rheumatoid arthritis.
Amyloid deposition causes bulky deposits that line the synovium and invade bone. T1W images show low signal tissue, with variable signal on T2W images due to a component of fluid within the amyloid masses. Low signal on both T1- and T2-weighting is suggestive of amyloid ( Fig. 11 ).

Processes Mimicking Inflammatory Arthropathies
Intra-articular osteoid osteoma
Osteoid osteomas are small benign bone-forming lesions that make up approximately 3% of all primary bone tumors with a peak incidence in the second decade of life. Although an inflammatory cause has been questioned, osteoid osteomas are classified as neoplasms due to the presence of chromosomal markers.
Osteoid osteomas can arise in any bone; the femoral neck is overall the most frequent anatomic site. Approximately 10% of osteoid osteomas are intra-articular locations with the hip joint most often involved , ; these lesions can promote joint effusions and adjacent soft tissue swelling. On MR imaging, a small nidus can be seen as a low-signal focus (nidus) surrounded by bone marrow edema-like signal with a joint effusion. Post-contrast images will typically show enhancement of the marrow around the nidus, and the synovium and soft tissues ( Fig. 12 ). The small nidus may be overlooked, leading to a misdiagnosis of a primary inflammatory process, sometimes resulting in unnecessary joint aspirations and delay in treatment. Awareness of the entity, and its MR imaging appearance, is important as the diagnosis should be considered in young patients presenting with monoarticular joint complaints. Computed tomography (CT) may help in identification of a nidus.