MR neurography offers a specialized approach for detailed nerve imaging when clinical symptoms indicate involvement. Imaging peripheral nerves in the foot and ankle is demanding due to their small size and challenging anatomy. This article provides an overview of foot and ankle nerve assessment, highlighting the importance of technical expertise and anatomic knowledge for accurate diagnosis.
Key points
- •
MR neurography (MRN) is a specialized imaging technique that allows for detailed evaluation of the foot and ankle peripheral nerves, providing crucial diagnostic information to guide optimal treatment decisions.
- •
A comprehensive assessment of intra- and perineural anatomy and pathology requires high-resolution imaging with fat- and water-sensitive contrasts. Combining 2-dimensional and 3-dimensional sequences typically yields the best results.
- •
MRN is instrumental in detecting a wide range of nerve abnormalities and their underlying causes, including entrapment neuropathies (eg, tarsal tunnel syndrome), traumatic nerve injuries, diffuse neuropathies, and neoplasms.
| 2D | 2-dimensional |
| 3D | 3-dimensional |
| SPAIR | spectral saturation using an adiabatic inversion pulse |
| MRN | MR neurography |
| PTN | posterior tibial nerve |
| LPN | lateral plantar nerve |
| MPN | medial plantar nerve |
| ICN | inferior calcaneal nerve |
| SPN | superficial peroneal nerve |
| DPN | deep peroneal nerve |
| SNR | signal-to-noise ratio |
| PD-weighted | proton density-weighted |
| STIR | short tau inversion recovery |
| DW | diffusion weighting |
| DWI | diffusion-weighted imaging |
| ADC | apparent diffusion coefficient |
| DTI | diffusion tensor imaging |
| TSE | turbo spin echo |
| PNST | peripheral nerve sheath tumor |
| NS-RADS | Neuropathy Score Reporting and Data System |
| CMT | Charcot-Marie-Tooth |
Introduction
Standard MR imaging of the ankle and foot provides excellent capabilities for comprehensive assessment of bones, ligaments, tendons, cartilage, and soft tissues. , However, many acute and chronic ankle and foot conditions can stem from peripheral nerve pathology. Imaging the foot and ankle nerves presents a unique challenge due to their small size, geometrically complex and tortuous course, and close topographic relation to accompanying blood vessels and fibro-osseous structures and tunnels.
Consequently, if clinical symptoms suggest the involvement of peripheral nerves, MR neurography (MRN) offers a more specialized approach that provides excellent capabilities for detailed imaging of nerves and their pathologic conditions. Comprehensive knowledge, including technical requirements, choice of sequences, anatomy, and the spectrum of pathologic conditions, is essential for optimal image acquisition and subsequent radiologic assessment. This article recapitulates the anatomy, discusses the current standard of techniques for MRN, and provides an overview of foot and ankle nerve assessment, emphasizing MRN’s role in evaluating common nerve conditions.
Anatomy of the foot and ankle nerves
The smallest structural unit of peripheral nerves is the axon, which is wrapped in Schwann cells and surrounded by fluid and connective tissue (endoneurium). Axons are grouped into fascicles, each enclosed by a connective tissue layer (perineurium). Multiple fascicles are bundled to form the entire nerve encased in an outer connective tissue layer (epineurium).
The foot receives 5 primary peripheral nerves, each following a unique pathway and serving distinct motor and/or sensory roles: the posterior tibial, superficial peroneal, deep peroneal, sural, and saphenous nerves.
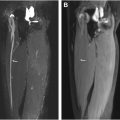
The tibial nerve arises from the sciatic nerve, descends dorsal/dorsomedial, and becomes the posterior tibial nerve (PTN) at the ankle ( Fig. 1 ). Before reaching the tarsal tunnel, it gives rise to the medial calcaneal nerve, which provides sensory innervation to the heel. Passing through the tarsal tunnel under the flexor retinaculum, the tibial nerve divides into the medial and lateral plantar nerves (MPN and LPN, respectively). The MPN supplies sensation to the medial two-thirds of the plantar foot and innervates the abductor hallucis, flexor hallucis brevis, flexor digitorum brevis, and the first lumbrical muscle. The LPN provides sensation to the lateral third of the foot sole, covering the fifth and part of the fourth digit, and motor innervation to most other intrinsic foot muscles, including the adductor hallucis, abductor digiti minimi, flexor digiti minimi brevis, lumbricals, and interossei. The inferior calcaneal nerve (ICN) arises typically from the LPN at the level of the medial malleolus or directly as the ICN, courses under the calcaneus to innervate structures near the heel, sending out small motor branches to the flexor digitorum brevis, quadratus plantae, and abductor digiti minimi.

The common peroneal nerve, the other major branch of the sciatic nerve, travels through the anterolateral compartments of the lower leg before giving rise to the superficial peroneal nerve (SPN) and the deep peroneal nerve (DPN).
The SPN descends within the peroneus longus muscle and emerges through the peroneal musculature about halfway down the anterolateral aspect of the lower leg through the crural fascia above the ankle joint. More inferiorly, it then divides into the medial and intermediate dorsal cutaneous nerves, which supply the dorsum of the foot. The DPN travels within the anterior compartment of the leg just anterior to the interosseous membrane, alongside the anterior tibial artery and vein. At the ankle, it enters the anterior tarsal tunnel and bifurcates into lateral and medial branches ( Fig. 2 ). The lateral branch innervates the extensor digitorum brevis and extensor hallucis brevis and provides sensory innervation to the ankle and sinus tarsi, while the medial branch provides sensory innervation to the first web space.

The sural nerve is a cutaneous nerve formed by contributions from the medial sural nerve (a branch of the tibial nerve) and the lateral sural nerve (from the common peroneal nerve). It descends along the posterolateral lower leg near the Achilles tendon, running alongside the lesser saphenous vein and supplying sensory innervation to the lateral ankle and foot. The saphenous nerve, originating from the femoral nerve, descends along the medial lower leg. Emerging between the sartorius and gracilis muscles and traveling close to the great saphenous vein, it provides sensation to the medial ankle and foot.
Technical considerations
MRN aims to produce images to visualize normal and abnormal nerve signals and morphology optimally. High-resolution visualization in multiple planes and contrasts is required for comprehensive evaluation of the nerves of the ankle and foot, including their small branches with sub-millimeter diameters ( Fig. 3 ). , ,

Field Strength and Coils
1.5 T and 3T MR imaging scanners can be used for MRN; however, 3T should be preferred when available. The increased signal-to-noise ratio (SNR) of 3T MR imaging permits higher image contrast and resolution and enables faster 3-dimensional (3D) imaging. , , However, artifacts due to B0 inhomogeneity and susceptibility can be more pronounced at 3T, making 1.5 T MR imaging more advantageous in the presence of metallic implants. , For maximal spatial resolution and optimal use of parallel imaging acceleration, a dedicated ankle/foot receiver coil should be used. , , ,
Pulse Sequences
Both fat- and water-sensitive contrasts are essential for comprehensively evaluating intra- and perineural anatomic and pathologic imaging characteristics. ,
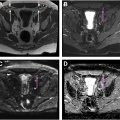
T1-weighted and proton density-weighted (PD-weighted) sequences provide excellent anatomic detail of peripheral nerves, offering optimal contrast against surrounding fat. , They also provide valuable information for the detection of intraneural fat, perineurial and epineurial thickening, effacement of the perineural fat plane due to mass lesions or focal fibrosis, characterization of mass lesions, and for depicting regional fatty infiltration and atrophy of muscles ( Fig. 4 ).

T2-weighted fat-suppressed images are essential for detecting abnormalities, typically leading to increased T2 signal in the affected part or surrounding nerve area. , , Containing endoneurial fluid, peripheral nerves have slightly longer T2 times than muscles, therefore T2-weighting with longer effective echo times (>60 ms) achieves optimal nerve-to-background contrast in fat-suppressed images, which is amplified in the presence of abnormalities. , , Water-sensitive sequences also enable sensitive detection of muscle edema in early denervation and allow further characterization of mass lesions.
Fat suppression techniques include short tau inversion recovery (STIR), spectral saturation using an adiabatic inversion pulse (SPAIR), or the Dixon technique. While STIR is a robust technique, it suffers from relatively low SNR and increased pulsation artifacts compared to SPAIR and should, therefore, be reserved for cases with expected B0 inhomogeneities and metal implants. Dixon is a usually more time-consuming alternative to SPAIR but allows for a more uniform fat suppression, which SPAIR can struggle with due to the geometry of the ankle and foot. Some authors have proposed acquiring STIR sequences after gadolinium-based contrast agents to suppress signals from adjacent vessels, achieving more nerve-specific imaging. However, intravenous contrast should generally be reserved for imaging neural or perineural mass lesions or infection, as it provides limited additional value in cases of trauma or entrapment neuropathy beyond vascular suppression. ,
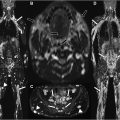
Due to their predominantly longitudinal orientation and diffusion anisotropy, adding diffusion weighting (DW) to anatomic sequences can enhance the selective conspicuity of peripheral nerves. Hybrid sequences like 3D diffusion-weighted reversed fast imaging with steady-state precession hybrid pulse sequences generate isotropic 3D images with excellent vascular suppression and improved peripheral nerve visibility ( Fig. 5 ). Although diffusion-weighted imaging (DWI) is not routinely performed, it can be used to support nerve-specific imaging. DWI facilitates apparent diffusion coefficient (ADC) measurements and offers qualitative insights into neuropathy, with neuropathic nerves often exhibiting asymmetrical hyperintensity or enlargement on high b-value images. Additionally, diffusion tensor imaging enables fractional anisotropy measurements and tractography, where changes in these metrics have been observed in various peripheral neuropathies associated with demyelination or axonal degeneration. ,

Two-dimensional turbo spin echo (TSE) sequences offer excellent in-plane resolution and a high signal yield. However, achieving adequate signal per slice generally requires a slice thickness of at least 2 to 4 mm, which limits through-plane resolution and leads to partial volume effects. This presents particular challenges in the ankle, where the anatomy involves oblique and curved courses for nearly all peripheral nerves. For comprehensive imaging, multiple acquisitions in various planes and, where indicated, oblique orientations are often needed. This approach can be time-consuming and increases the chance of errors at acquisition. With ongoing advancements, isotropic high-resolution 3D TSE MR imaging can be achieved within acquisition times of approximately 5 min per sequence. Vendor-specific implementations include SPACE (sampling perfection with application-optimized contrasts using different flip angle evolution, Siemens Healthineers, Erlangen, Germany), CUBE (GE Healthcare, Waukesha, WI), and VISTA (volumetric isotropic T2-weighted acquisition, Philips, Best, The Netherlands). Resulting in high-resolution image data with isotropic voxel sizes as small as (0.5 mm) 3 provides limitless possibilities for linear and curved reconstructions after acquisition, without interslice gaps and partial volume effects ( Fig. 6 ). Curved planar reconstructions and maximum intensity projections (MIP) enable longitudinal visualization of nerves, which is particularly beneficial for topographic analysis and presurgical planning. ,

However, despite these advantages, 3D sequences have not fully replaced 2D sequences in MRN due to comparatively lower in-plane resolution and longer acquisition times. A combination of 2D and 3D sequences usually yields optimal results by leveraging the strengths of both techniques.
Recommended sequence combinations for comprehensive MRN in the foot and ankle include axial T1-or PD-weighted sequences, axial T2 SPAIR or T2 Dixon, coronal or sagittal PD-weighted sequences, 3D SPAIR TSE, and 3D DW PSIF. , For smaller nerves in the hindfoot, nerve-perpendicular and oblique axial images across the axis of the calcaneus are useful for optimal evaluation of medial plantar, lateral plantar, and calcaneal nerves. The slice thickness for 2D imaging is ideally kept small at 2.5 to 3.5 mm with a 0% to 10% gap, and axial images should have an in-plane resolution of at least 0.4 mm. 3D imaging should aim for isotropic voxel sizes under 1 mm 3 . ,
Deep Learning-based Image Reconstruction
Recent advances in deep learning (DL)-based image reconstruction hold considerable promise for MRN. Advanced denoising and super-resolution techniques have significantly enhanced the image quality in standard musculoskeletal MR imaging while reducing scan times. Given the small structure of nerves and the demand for image details in their evaluation, such DL techniques may be well-suited for MRN. First, studies with commercially available DL techniques have shown substantial improvements in peripheral nerve evaluation in 2D and 3D MRN, greatly enhancing nerve visibility compared to standard reconstruction methods. ,
General considerations for MR neuropathy interpretation and grading
A structured approach is beneficial to assess the full range of nerve lesions, and correlating clinical symptoms, examination findings, and electrodiagnostic results significantly enhances diagnostic accuracy and reduces the risk of false positives and negatives. , , , , Comprehensive MRN evaluation should include the entire neuromuscular unit, assessing both the nerve and the innervated muscle and considering alternative diagnoses that may explain the clinical symptoms.
Normal And Abnormal Appearance of Peripheral Nerves
Normal peripheral nerves should generally exhibit isointense signals relative to skeletal muscle on T1-and PD-weighted images and usually demonstrate a slightly hypertense signal on T2-weighted images ( Fig. 7 ). ,