Musculoskeletal System
Catherine C. Roberts
Laura W. Bancroft
Thomas L. Pope Jr.
The authors and editors acknowledge the contribution of the Chapter 2 author from the second edition: Riyadh Al-Okaii, MD
Case 2.1
HISTORY: A 39-year-old man fell
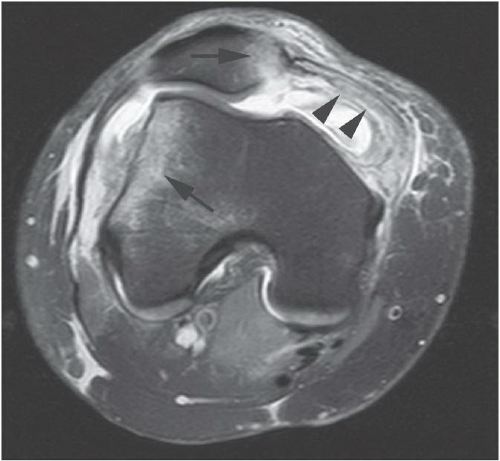
FINDINGS: Axial, T2-weighted fat-suppressed MR image (Fig. 2.1.1) shows bone contusions in the medial patella and the lateral femoral condyle (arrows) with an associated tear of the medial retinaculum (arrowheads).
DIAGNOSIS: Acute patellar dislocation-relocation (PDR)
DISCUSSION: Acute PDR is a common injury that occurs with a variety of activities and accounts for 2% to 3% of knee injuries overall, but has a higher incidence in active populations (1). It characteristically occurs with internal rotation of the femur on a fixed and externally rotated tibia or a direct blow to the medial side of the knee. In PDR, the patella dislocates laterally, and the medial patellar facet impinges on the lateral femoral condyle, producing bone contusions at both sites. Because the bone contusions result from direct impaction as they are in the transient dislocation of the knee associated with ACL tears, the contusions may also be called “kissing contusions.” Clinical evaluation of the patient with PDR is often difficult because of the large knee joint effusion and because the patella is usually relocated to its near anatomic position at the time of presentation. The patient may not realize that patellar dislocation has occurred.
Radiographs may show a lipohemarthrosis or a chip fracture adjacent to the donor site of the medial facet of the patella. MR findings associated with PDR include any or all of the following: disruption or sprain of the medial retinaculum, lateral patellar tilt or subluxation, lateral femoral condylar and medial patellar osseous contusions, osteochondral injury to the medial patella or lateral femur, intraarticular sliver-like osseus fragment, damage to Hoffa’s fat pad, and joint effusion or lipohemarthrosis (23456). MR imaging is recommended for all patients with PDR since they often have concomitant injury to the major ligaments of the knee or the menisci (7). Redislocation occurs in up to 63% of patients, and more than one-half of these untreated patients will have fair to poor outcomes. Surgical repair versus closed management is tailored to the patient’s clinical situation (8).
Aunt Minnie’s Pearls
Bone contusions of the medial patellar facet and lateral femoral condyle (i.e., “kissing contusions”) are seen with PDR.
Meniscal or ligamentous injuries are often associated findings in PDR.
Aggressive surgical repair is indicated to avoid chronic, repetitive dislocation and morbidity.
Case 2.2
HISTORY: A 61-year-old woman with shoulder pain (Figs. 2.2.1 and 2.2.2). (Fig. 2.2.3 is described under Discussion.)
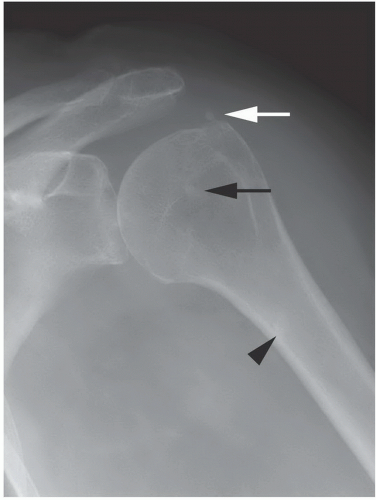
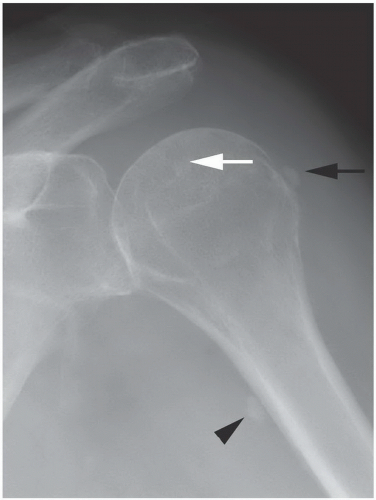
FINDINGS: AP radiographs of the left shoulder in external (Fig. 2.2.1) and internal (Fig. 2.2.2) rotation demonstrate globular foci of calcification in the expected location of the supraspinatus (white arrow), infraspinatus (black arrow), and pectoralis major (arrowheads) tendons.
DIAGNOSIS: Hydroxyapatite deposition disease (HADD)
DISCUSSION: HADD consists of crystal deposition in and around joints, without a known cause (9). Two-thirds of patients are asymptomatic (10). HADD can be the cause of acute pain and be associated with fever, increased erythrocyte sedimentation rate, and C-reactive protein. Other terms used to describe this entity include calcific tendonitis, hydroxyapatite rheumatism, calcific periarthritis, and peritendinitis calcarea.
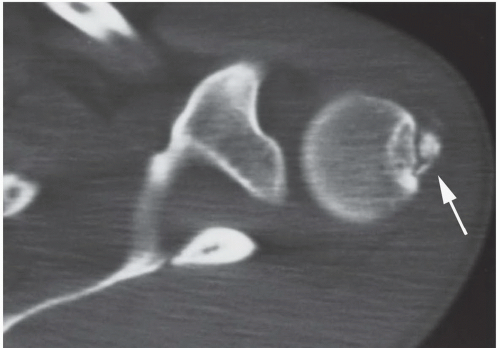
On radiographs, the calcium deposits appear cloud-like and amorphous and can involve the tendon, ligament, bursa, or joint capsule. Intraarticular crystal deposition can destroy the joint space, resulting in a condition referred to as “Milwaukee shoulder.” The shoulder is most commonly involved. On CT, accompanying erosion of the underlying bone can be seen (Fig. 2.2.3). If the interpreting radiologist is not familiar with this entity, bone erosion from HADD can be misinterpreted as reflecting an aggressive malignant process. Biopsy of these areas in equivocal cases can exclude malignancy, but the hydroxyapatite crystals are beyond the resolution of light microscopy, so a specific pathologic diagnosis of HADD will not result unless electron microscopy or electron diffraction studies are utilized. Alizarin S stain can screen for crystals but identifies other calcium crystals as well. The CT appearance has been described as commonly having a flame-shaped or comet-tail configuration of the calcifications (11,12). If calcification and erosion occur in a region not typical for HADD, additional workup to exclude malignancy is necessary.
Aunt Minnie’s Pearls
HADD is commonly referred to as calcific tendinosis and usually has an innocuous appearance on radiographs consisting of cloud-like calcification.
HADD typically is asymptomatic until migration of the calcification can be the cause of acute pain.
HADD can have an aggressive, erosive appearance on CT, especially when involving the pectoralis major origin, which can be misinterpreted as malignancy.
Case 2.3
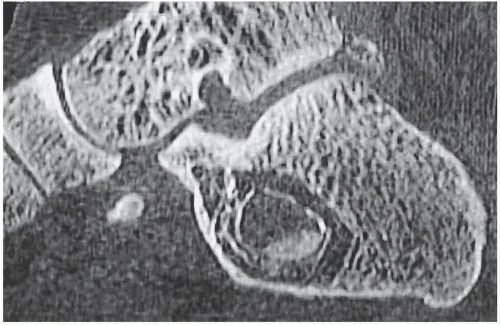
HISTORY: Three individuals with foot pain
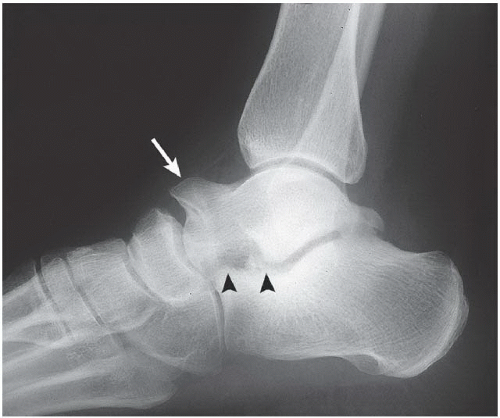
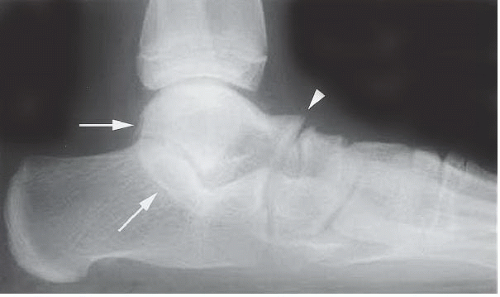
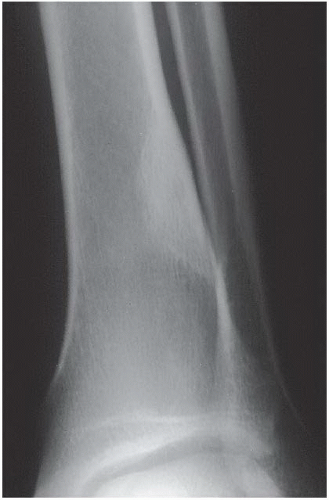
FINDINGS: A lateral radiograph of the left foot (Fig. 2.3.1) demonstrates a prominent talar beak (arrow) and bony sclerosis overlying the middle facet (arrowheads). Coronal CT through the middle facet shows talocalcaneal fusion, with bony bridging between the talus and the sustentaculum tali of the calcaneus (Fig. 2.3.2, arrow). Figures 2.3.3 to 2.3.6 are explained under Discussion.
DIAGNOSIS: Tarsal coalition
DISCUSSION: Tarsal coalition, an abnormal fusion of one or more of the tarsal bones, may be fibrous, cartilaginous, or osseous and may be posttraumatic or result from articular disease, infection, or surgery. It may be congenital, usually a consequence of autosomal dominant inheritance, and it has been linked to several syndromes. Research on defining the exact DNA point mutations is ongoing (131415). The most common tarsal coalitions are calcaneonavicular and talocalcaneal (16). Almost all talocalcaneal coalitions occur between the sustentaculum tali of the calcaneus and the middle facet of the talus. The incidence of tarsal coalition is <1% (17,18). The disorder is more common in male patients, may be bilateral in up to 50% of patients, and is most commonly discovered during the second and third decades of life (14,19). Multiple ipsilateral coalitions have been described (14). The peroneal spastic flatfoot deformity may be the initial clinical manifestation in many of these patients because of decreased subtalar motion (20).
Radiographically, calcaneonavicular coalition may be suspected because of elongation of the anterior facet of the calcaneus on radiographs (i.e., anteater sign; Fig. 2.3.3, arrow). The 45-degree medial oblique view is the best diagnostic radiographic projection to demonstrate this type of coalition (Fig. 2.3.4). CT can also be used to confirm coalition and shows sclerosis at the articulation (Fig. 2.3.5). Congenital coalition usually evolves from fibrous to osseous coalition and may not be apparent on the initial evaluation.
Talocalcaneal coalition can result in dorsal beaking of the talar head (Fig. 2.3.6, arrowhead), the so-called C-sign (Fig. 2.3.6, arrows), a ball-and-socket ankle mortise, asymmetry of the inferior talar necks, widening of the lateral talar process, nonvisualization of the subtalar joint medial facet (21), and close approximation between the talus and calcaneus. For definitive diagnosis of either type of coalition, CT is the preferred investigation in most cases (22).
Aunt Minnie’s Pearls
The most common types of tarsal coalition are talocalcaneal and calcaneonavicular.
Talocalcaneal coalition is bilateral in approximately 25% to 50% of patients.
CT is the investigation of choice for the diagnosis of tarsal coalition.
The anteater sign is seen in calcaneonavicular coalition.
A talar beak, obscured middle facet, and C-sign are seen in talocalcaneal coalition.
Case 2.4
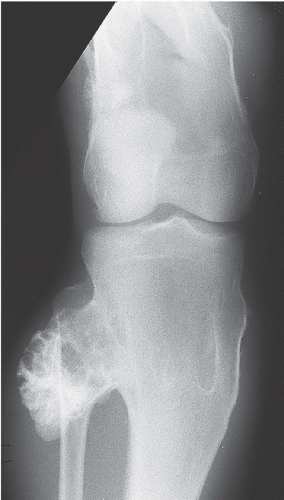
HISTORY: A 23-year-old man with pain in the right hip
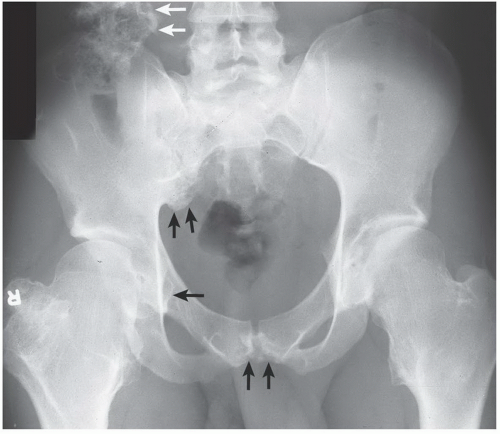
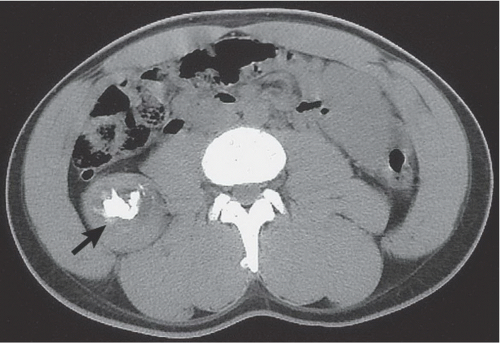
FINDINGS: An anteroposterior view of the pelvis (Fig. 2.4.1) shows flaring of the metaphyseal regions of the proximal femurs and numerous osteochondromas arising from the right iliac crest, pubic bones, and proximal right femur (arrows). An axial CT image through the upper pelvis demonstrates a large, right exostosis with an associated soft-tissue mass (Fig. 2.4.2, arrow). An anteroposterior radiograph of the knee shows multiple osteochondromas arising from the femur and the fibula (Fig. 2.4.3). Figures 2.4.4 and 2.4.5 show the classic radiographic findings in the distal femur and forearm in other patients with this same disorder.
DIAGNOSIS: Multiple hereditary exostosis (i.e., diaphyseal aclasia)
DISCUSSION: Multiple hereditary exostosis is an autosomal dominant disorder that usually manifests in the first or second decades of life. Pain may be the presenting symptom because of compression of neurovascular structures by the osteochondromas. Initial signs of the disorder may include decreased range of motion, deformities caused by bowing or shortening of the involved bones, and palpable masses adjacent to joints. The osteochondromas are generally bilateral and most commonly involve the femur, tibia, fibula, and humerus. The scapula, innominate bone, ribs, radius, and ulna may also be affected.
Complications occurring in multiple hereditary exostosis are the same as those associated with solitary exostosis: fracture, vascular injury, bursal formation, neurologic compromise, osseous deformity, and malignant transformation. The risk of malignant transformation is 5% in the patient with multiple hereditary exostoses and <1% in those with solitary exostosis. Clinical features of pain, swelling, palpable mass, and imaging findings showing growth of a previously stable exostosis, new bony erosion, or development of new or increasing calcifications are signs of potential malignant transformation. The definitive diagnosis of a developing malignancy is determined by open biopsy and pathologic examination. The most frequently associated malignant tumor is chondrosarcoma, usually developing in the femur, tibia, humerus, or innominate bone (Fig. 2.4.2, arrow) (23,24).
Aunt Minnie’s Pearls
Abnormal modeling of bone and osseous deformity are characteristic of multiple hereditary exostosis.
New pain, mass, bony erosion, or calcifications may indicate malignant transformation.
Definitive diagnosis of malignant degeneration requires open biopsy and pathologic examination.
Case 2.5
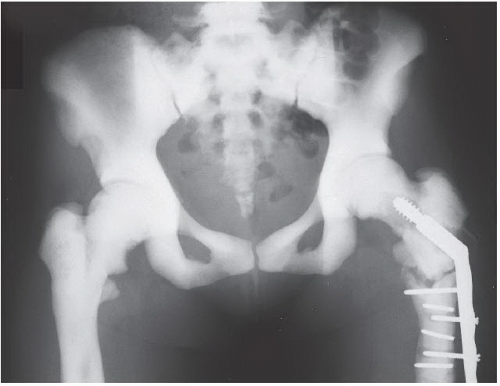
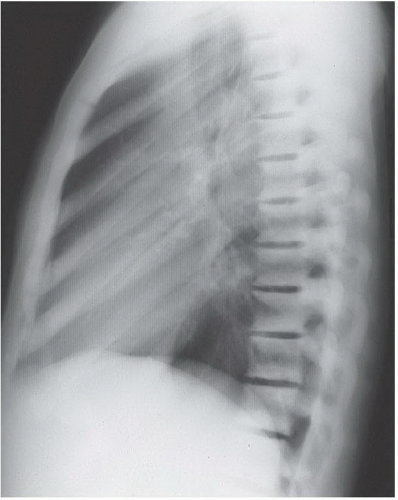
HISTORY: Three patients with the same diagnosis
FINDINGS: Anteroposterior view of the pelvis (Fig. 2.5.1) in a 22-year-old woman shows diffuse, uniform, bony sclerosis and a subtrochanteric fracture of the proximal left femur. A lateral chest radiograph of another patient (Fig. 2.5.2) shows the sandwich appearance of the vertebral bodies caused by increased sclerosis of the superior and inferior end plates. Radiographs of the knees in a younger patient (Fig. 2.5.3) show splaying of the metaphyses and alternating radiolucent bands in the distal femurs and proximal tibias and fibulas bilaterally.
DIAGNOSIS: Osteopetrosis
DISCUSSION: Osteopetrosis is a complex hereditary disorder characterized by a defect in osteoclastic resorption. Four subtypes are described with distinct clinical and radiographic features. The two most common subtypes are the precocious and delayed types. The autosomal recessive, precocious form is lethal, and the patients usually die shortly after birth or survive for only a few years. Clinically, they are characterized by hepatosplenomegaly, failure to thrive, and blindness. Patients with the autosomal dominant, delayed form are generally asymptomatic but may have mild anemia, cranial nerve deficits, pathologic fracture, or bleeding problems after tooth extraction (25).
The imaging features of osteopetrosis consist of generalized osteosclerosis and diffuse cortical thickening with narrowing of the medullary cavity. Typical radiographic features include the bone-within-bone appearance, metaphyseal undermodeling and widening (i.e., Erlenmeyer flask deformity), radiolucent
and radiodense bands near the ends of long bones, and obliteration of mastoid air cells and paranasal sinuses. Potential complications of osteopetrosis include fractures (i.e., bones are weaker than normal), crowding of normal bone marrow spaces resulting in pancytopenia and extramedullary hematopoiesis, and osteosclerosis of the basal foramina of the skull with resultant cranial nerve deficits (26).
and radiodense bands near the ends of long bones, and obliteration of mastoid air cells and paranasal sinuses. Potential complications of osteopetrosis include fractures (i.e., bones are weaker than normal), crowding of normal bone marrow spaces resulting in pancytopenia and extramedullary hematopoiesis, and osteosclerosis of the basal foramina of the skull with resultant cranial nerve deficits (26).
Aunt Minnie’s Pearls
Osteosclerosis + alternating radiolucent bands + metaphyseal widening = osteopetrosis.
The major complications are pathologic fractures, pancytopenia, and cranial nerve defects.
Case 2.6
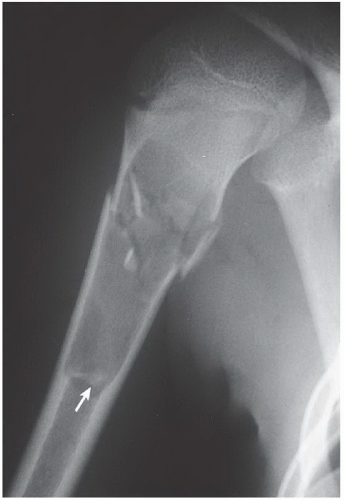
HISTORY: A 11-year-old boy with right arm pain after a fall (Figs. 2.6.1 and 2.6.2). Figure 2.6.3 shows the same lesion in the femur of a different patient.
FINDINGS: Anteroposterior and lateral views of the proximal right humerus (Figs. 2.6.1 and 2.6.2) demonstrate a well-circumscribed, geographic, lytic metaphyseal lesion with cortical thinning. The lesion has well-defined margins and no demonstrable matrix. A comminuted fracture has occurred, and fragments of the cortex have fallen to the dependent portion of the lesion (arrows). Figure 2.6.3 exhibits the same lesion in the femur of a 7-year-old boy.
DIAGNOSIS: Unicameral bone cyst
DISCUSSION: Unicameral or simple bone cysts are benign lesions of unknown origin that are often initially discovered because of pathologic fracture. The “fallen-fragment sign” is the distinguishing feature in these lesions because the fragments can reach this position only in purely cystic lesions (27). These tumors are uncommon, comprising only 5%
of all primary bone tumors. The most common sites of involvement are the proximal humerus, femur, tibia, or fibula. Most lesions are identified in the second decade, and there is a 2:1 male predominance. Lesions near the metaphysis are active, but as the patient grows, the lesion migrates to the diaphysis of the bone and becomes inactive. Treatment includes curettage and packing with bone chips or steroid injection. Lesions have been reported to resolve spontaneously (28).
of all primary bone tumors. The most common sites of involvement are the proximal humerus, femur, tibia, or fibula. Most lesions are identified in the second decade, and there is a 2:1 male predominance. Lesions near the metaphysis are active, but as the patient grows, the lesion migrates to the diaphysis of the bone and becomes inactive. Treatment includes curettage and packing with bone chips or steroid injection. Lesions have been reported to resolve spontaneously (28).
Aunt Minnie’s Pearls
Unicameral bone cysts are most common in the proximal humerus and femur.
The fallen-fragment sign confirms the cystic nature of this lesion.
Case 2.7
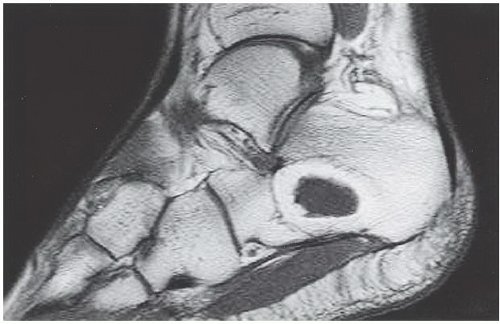
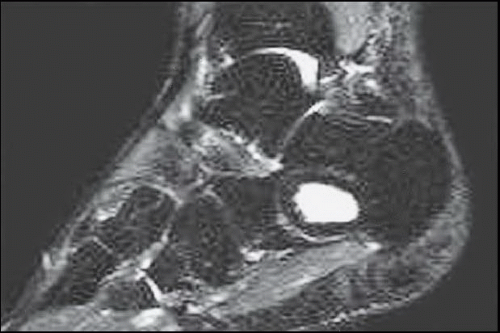
HISTORY: A 55-year-old woman (Fig. 2.7.1) and 47-year-old man (Figs. 2.7.2 to 2.7.5), both with foot pain
FINDINGS: A lateral radiograph of the left foot (Fig. 2.7.1) shows a nonaggressive, well-defined lytic lesion in the anterior aspect of the calcaneus with a thin sclerotic border and central calcification. A lateral radiograph of the foot (Fig. 2.7.2) shows a lytic lesion in the calcaneus with central calcification. Sagittal T1-weighted (Fig. 2.7.3) and short tau inversion recovery (STIR) (Fig. 2.7.4) MR images demonstrate a lesion with signal characteristics of peripheral fat and a cystic center. No soft-tissue mass is present. Figure 2.7.5 is explained under Discussion.
DIAGNOSIS: Intraosseous lipoma
DISCUSSION: Intraosseous lipomas, comprising <1% of all primary bone tumors, are most commonly diagnosed in the fourth to sixth decades of life. However, the lesions have been reported in patients up to 75 years of age. Male and female patients are equally affected. The lesion averages 4 cm in diameter and is usually found within the metaphyses of the long tubular bones of the femur, tibia, and fibula or within the calcaneus (29,30). Multiple intraosseous lipomas are rare.
The intraosseous lipoma is characterized radiographically by radiolucency; a thin, sclerotic margin; and occasionally by lobulation or intraosseous ridges. Bony expansion, when it occurs, is usually within the small tubular bones. In the calcaneus, this lesion typically resides in a relatively lucent triangle anteriorly and may, as in this case, show a central area of calcification or ossification. Lipomas arising in the proximal femur may be associated with ossification along the margin of the intertrochanteric line. Histologically, intraosseous and extraosseous lipomas are
identical (31). CT or MRI can be used as adjunct imaging tests to confirm the diagnosis of intraosseous lipoma. On MRI, the lesion has signal characteristics identical to fat, and CT demonstrates the fat within the lesion (Fig. 2.7.5). Treatment is usually unnecessary when characteristic lesions are seen in asymptomatic patients. If the patient complains of pain, a biopsy followed by bone grafting may be required.
identical (31). CT or MRI can be used as adjunct imaging tests to confirm the diagnosis of intraosseous lipoma. On MRI, the lesion has signal characteristics identical to fat, and CT demonstrates the fat within the lesion (Fig. 2.7.5). Treatment is usually unnecessary when characteristic lesions are seen in asymptomatic patients. If the patient complains of pain, a biopsy followed by bone grafting may be required.
Aunt Minnie’s Pearls
A lytic lesion with a thin, sclerotic border and central calcification (especially within the calcaneus) represents an intraosseous lipoma until proven otherwise.
The average size of intraosseous lipoma is 4 cm.
Case 2.8
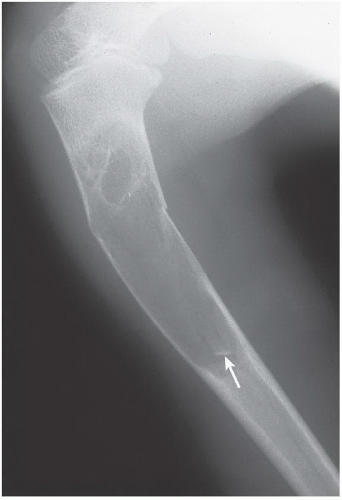
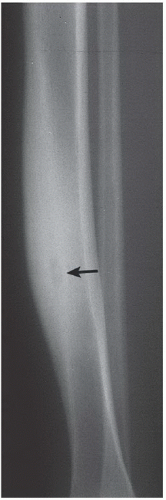
HISTORY: Adolescent child with pain in the leg (Figs. 2.8.1 and 2.8.2). Figure 2.8.3 is the same lesion in the humerus of a different patient.
FINDINGS: There is a well-defined, eccentric, radiolucent lesion with a thin, sclerotic border adjacent to the cortex of the distal tibia (Fig. 2.8.1). A repeat study 7 years later shows a well-defined sclerotic lesion in the same location (Fig. 2.8.2). Figure 2.8.3 shows an identical lesion in a different patient with a pathologic fracture, an uncommon complication of this lesion.
DIAGNOSIS: Fibrous cortical defect (FCD) or nonossifying fibroma (NOF)
DISCUSSION: FCD, the common designation for this entity, is often used synonymously with NOF. Although the lesions are identical histologically, some authorities call lesions 2 cm and larger NOF, whereas those <2 cm are called FCD. These lesions are usually discovered as an incidental finding on imaging done for other reasons and rarely cause symptoms (32).
FCD or NOF occurs in up to 40% of children older than 2 years; 95% of the lesions occur in patients younger than 20 years. Eighty percent of the lesions occur in the lower extremity, and about 25% of lesions are polyostotic. Polyostotic forms are often associated with neurofibromatosis, fibrous dysplasia, and Jaffe-Campanacci syndrome. Lesions originally arise adjacent to the physis, and as limb lengthening occurs, they migrate away from the joint. The typical FCD or NOF is radiolucent; has a thin, sclerotic margin; and shows no periosteal reaction. Rarely, it may be expansile or undergo pathologic fracture, as the lesion in Figure 2.8.3. The natural history of FCD or NOF is to involute during adolescence and to become sclerotic, as in the patient of Figures 2.8.1 and 2.8.2. When the characteristic imaging features are encountered on radiography, no further imaging or treatment is necessary. The only indication for treatment is if there has been a pathologic fracture through the lesion and fracture fixation is needed (33).
Aunt Minnie’s Pearls
Eccentric, well-defined, lucent lesion in a young asymptomatic patient is most likely an FCD or NOF.
When classic, uncomplicated radiographic findings are present, no treatment or further imaging is necessary.
Case 2.9
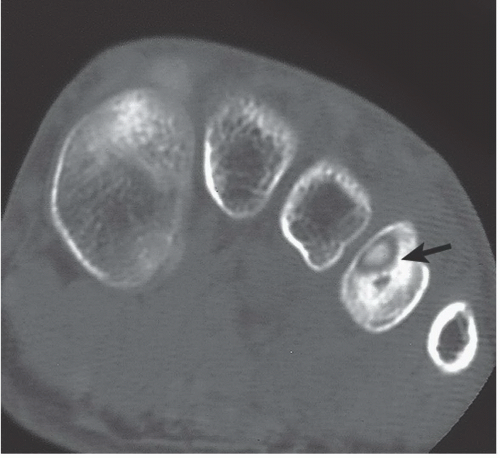
HISTORY: A 12-year-old boy with pain in the lower leg (Figs. 2.9.1 and 2.9.2) and 10-year-old boy with pain in the foot (Figs. 2.9.3 and 2.9.4). Figure 2.9.5 is the same lesion in a different patient.
FINDINGS: Anteroposterior (Fig. 2.9.1) and lateral (Fig. 2.9.2) radiographs of the lower leg in the first patient show a focal area of sclerosis in the midshaft of the tibia with a central area of radiolucency (arrow). In the second patient, an oblique view of the left foot (Fig. 2.9.3) shows sclerosis of the shaft of the fourth metatarsal with an associated central radiolucency (arrow). A corresponding axial CT image (Fig. 2.9.4) demonstrates the region of sclerosis and confirms the central radiolucency (arrow). An axial, gadolinium-enhanced, fast spoiled-gradient echo image (Fig. 2.9.5) from another patient demonstrates the intensely enhancing nidus (arrow) in the anterior aspect of the distal femur.
DIAGNOSIS: Osteoid osteoma
DISCUSSION: Osteoid osteoma is a benign osteoblastic neoplasm composed of a central core of vascular osteoid tissue and a peripheral zone of sclerotic bone. The cause is unknown. Most osteoid osteomas occur in patients between the ages of 5 and 25 years, and there is a 3:1 male predominance. With rare exceptions, pain is a hallmark of osteoid osteoma, and without this symptom, the diagnosis should be questioned. The characteristic history of pain, which is worse at night and relieved by small doses of aspirin (salicylates), can be elicited from about 50% of patients. Symptoms and signs of a systemic illness are generally absent, and results of laboratory tests are usually normal (34).
Osteoid osteoma has a predilection for the diaphysis of the long bones of the lower extremity, and about 60% of the lesions occur in the femur and tibia. Other common sites are the humerus, bones of the hands and feet, and posterior elements of the spine, where the lesions are usually located
at the base of the transverse process, pedicle, or lamina (35). Multifocal lesions are rare (36,37).
at the base of the transverse process, pedicle, or lamina (35). Multifocal lesions are rare (36,37).
The classic radiographic appearance, virtually diagnostic of osteoid osteoma, is demonstrated in these two examples: a centrally located ovoid radiolucent area (nidus), measuring <1 cm in diameter and surrounded by a zone of uniform bony sclerosis. There may also be a focus of calcification within the radiolucent nidus. Additional modalities helpful in diagnosing osteoid osteoma are bone scintigraphy, CT, and MRI. On the radionuclide bone scan, the double-density sign with intense accumulation centrally and less marked uptake in the periphery is characteristic of osteoid osteoma. Bone-seeking radiopharmaceuticals may be used for intraoperative or percutaneous therapeutic guidance (38). CT is particularly useful for evaluating lesions in the spine, pelvis, or femoral neck. Prompt arterial enhancement on dynamic MR can help differentiate osteoid osteoma from Brodie abscess and stress injuries in equivocal cases (39). Conventional therapy includes open or percutaneous excision of the entire nidus (34). Radiofrequency ablation is an excellent minimally invasive option for treatment (40).
Aunt Minnie’s Pearls
Pain that is worse at night and relieved by salicylates is characteristic of osteoid osteoma.
The nidus is the radiolucent area on radiographs and the enhancing region on MRI.
Ablation or excision of the entire nidus is usually curative; recurrence is rare.
Case 2.10
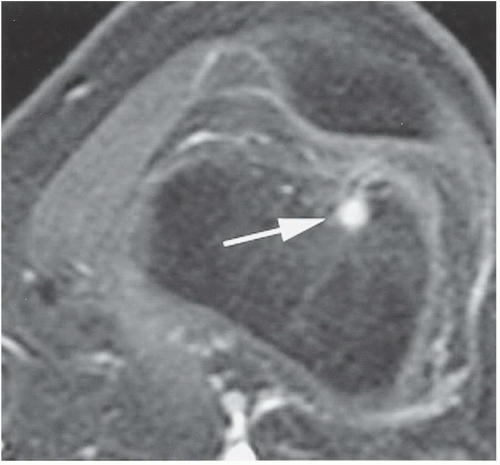
HISTORY: A 35-year-old woman with pain in the right knee
FINDINGS: Sagittal proton-density (Fig. 2.10.1) and fast spin-echo, T2-weighted fat-suppressed (Fig. 2.10.2) MR images of the right knee joint demonstrate a low-signal-intensity mass in the upper aspect of the infrapatellar fat pad (i.e., Hoffa’s fat pad) on both imaging sequences (arrows).
DIAGNOSIS: Pigmented villonodular synovitis (PVNS)
DISCUSSION: PVNS is a proliferative disorder of the synovium that usually affects adults in the third and fourth decades of life. The exact cause is unknown, but it is likely related to inflammatory or posttraumatic processes. The knee is the most commonly involved joint, followed in descending frequency by the hip, elbow, and ankle, although any joint may be affected. Generally, the disorder is monarticular but multicentric involvement may be encountered (41). The disease affects the sexes equally, with some series showing predominance of disease in either gender (424344). A history of trauma can be elicited in about 50% of cases.
Symptoms depend on whether the disease is focal or diffuse and include pain, swelling, and diminished range of motion. Aspiration of the joint may show the hemorrhagic and characteristic “chocolate” effusion.
Classic radiographic features of PVNS include soft-tissue swelling, joint effusion, preservation of articular space, absence of osteoporosis, and bony erosions or cysts. Although there are rare reports of atypical cases that contain calcium (45,46), evidence of calcification or metaplastic cartilage in essence excludes the diagnosis of PVNS. The MR features of low signal intensity on T1-weighted, T2-weighted, or gradient-echo sequences result from the hemosiderin deposition in PVNS. However, hemosiderin deposition within hemophilia, synovial hemangioma, or neuropathic osteoarthropathy, all of which are associated with a chronic hemarthrosis, may also result in low signal intensity on these MR sequences (474849). Treatment of PVNS is arthroscopic or surgical excision of the lesions with synovectomy.
Aunt Minnie’s Pearls
Lesions of PVNS, because of the hemosiderin deposits, generally have low signal intensity on T1- and T2-weighted MR images.
Hemosiderin deposits (low T1- and T2-weighted signal) may also be seen in hemophilia, synovial hemangioma, and neuropathic osteoarthropathy.
Aspiration of the hemorrhagic or “chocolate” effusion is typical of PVNS.
Case 2.11
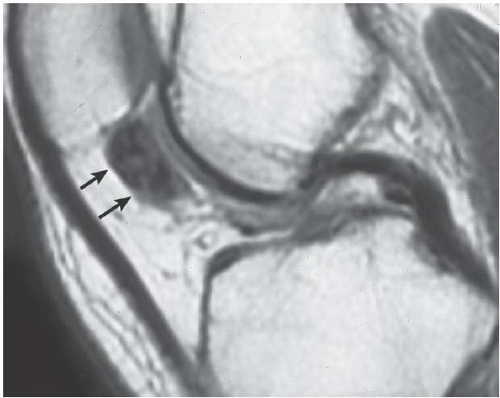
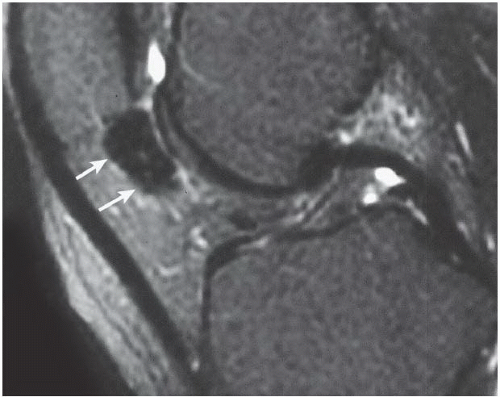
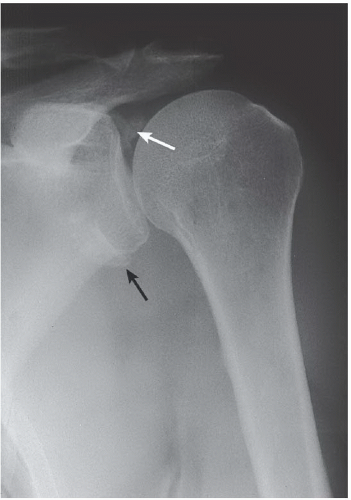
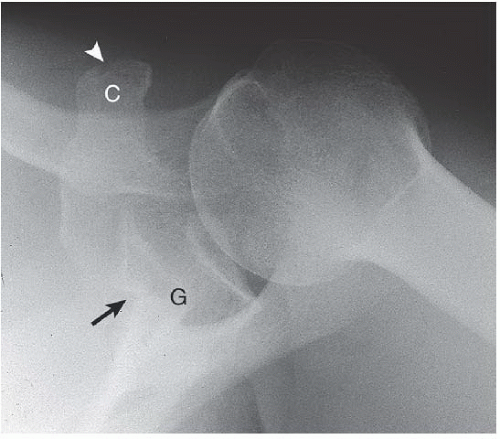
HISTORY: A 52-year-old man with a prior shoulder injury (Figs. 2.11.1 to 2.11.4)
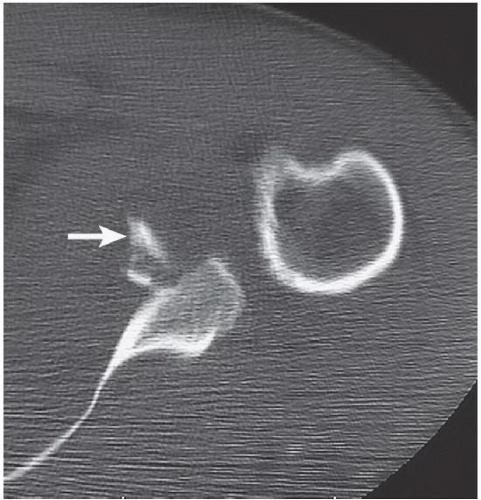
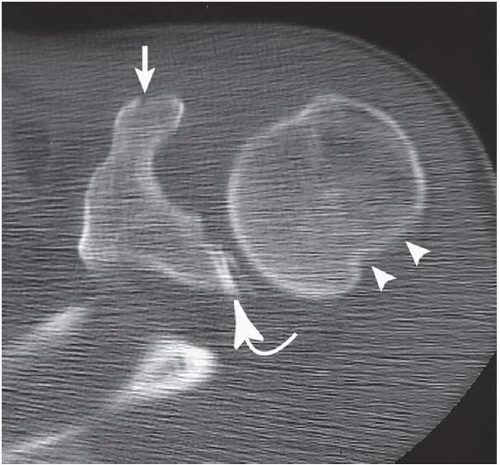
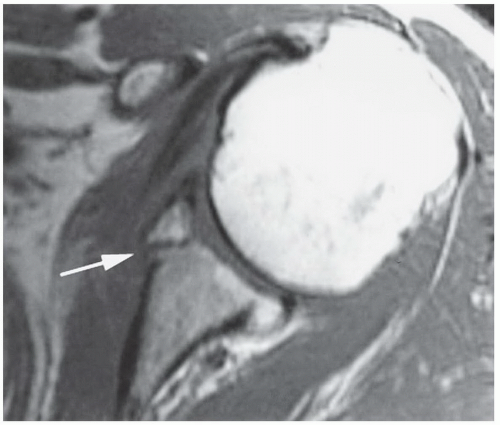
FINDINGS: Anteroposterior (Fig. 2.11.1) and axillary (Fig. 2.11.2) views of the left shoulder show small fragments of bone (arrows) adjacent to the superior and inferior aspect of the glenoid (G) and a nondisplaced coracoid (C) fracture (arrowhead). Axial CT images through the shoulder joint show a fracture of the anteroinferior aspect of the glenoid (i.e., Bankart lesion) (Fig. 2.11.3, arrow). Another CT image (Fig. 2.11.4) reveals fractures of the superior glenoid (curved arrow), coracoid process (arrow), and a compression fracture of the posterolateral aspect of the humeral head (i.e., Hill-Sachs lesion; arrowheads). Figure 2.11.5 is explained under Discussion.
DIAGNOSIS: Bony Bankart lesion of the shoulder with an associated Hill-Sachs deformity of the humeral head caused by anterior glenohumeral dislocation
DISCUSSION: The classic Bankart lesion is an avulsion of the anterior labroligamentous structures from the anterior glenoid rim. A bony Bankart consists of injury to the glenoid labrum and the anterior and inferior rim of the glenoid. Figure 2.11.5 of another patient shows the bony Bankart lesion with a fracture of the anterior and inferior aspect of the glenoid (arrow).
With anterior glenohumeral dislocation, the humeral head dislocates anteriorly and inferiorly in relation to the glenoid and may result in any or all of the following lesions: compression fracture of the superior and posterolateral aspect of the humeral head (i.e., Hill-Sachs lesion), stripping of the anterior capsule of the joint, and fractures of the cartilaginous labrum or of the osseous rim of the glenoid. Large, osseous glenoid fractures can be seen on standard anteroposterior views. Often, however, axillary shoulder views or more specialized views, such as the West Point view, are necessary to visualize more subtle bony injuries (50). Demonstration of the fibrocartilaginous Bankart lesion requires CT arthrography or MRI (515253).
Aunt Minnie’s Pearls
The Bankart lesion of the anterior inferior glenoid labrum is caused by traumatic anterior dislocation of the shoulder.
A compression fracture of the posterolateral humeral head (i.e., Hill-Sachs deformity) is often an associated finding.
MRI or CT arthrography is required to diagnose the purely fibrocartilaginous Bankart lesion.