Nasopharynx
Key Points
Nasopharyngeal carcinoma (NPC) is uncommon in the United States, but is endemic in many areas in Asia, particularly southeastern China.
In endemic regions, NPC is strongly associated with Epstein-Barr virus (EBV).
Radiation is the mainstay of treatment. The addition of chemotherapy has been demonstrated to improve disease control rates in locally advanced NPC.
Because NPC is located in a horseshoe-shaped region in the proximity of critical normal structures, IMRT is increasingly used for its treatment to improve conformality of dose distribution to the tumor and to reduce dose to the brain stem, optic nerve and chiasm, temporal lobes, parotid glands, etc.
Increasing body of data indicate that IMRT improves geographic coverage of larger NPC resulting in high disease control rate while reducing toxicity, particularly xerostomia.
With the improvement of the local-regional control rate, distant metastasis has become the leading pattern of relapse in NPC.
TREATMENT STRATEGY
The current standard treatment for stage I nasopharyngeal carcinoma (NPC) is radiotherapy, though consideration for concurrent chemoradiation can be given for patients with bulky T1 disease. It is important to note that larger T1 tumors in the current American Joint Committee on Cancer (AJCC) staging system were staged as T2 or even T3 in prior editions and thus included in trials evaluating the role of chemotherapy for patients with locally advanced NPC.
The standard treatment for stage II to IV NPC is combination of radiation and chemotherapy. Outside protocol study setting, the recommended chemotherapeutic regimen in the United States was established through an intergroup Phase III trial. This regimen consists of 100 mg/m2 of cisplatin given during weeks 1, 4, and 7 of radiation, followed 3 to 4 weeks later by three courses of adjuvant therapy comprising 80 mg/m2 of cisplatin given on day 1 and 1,000 mg/m2/d of fluorouracil on days 1 to 4, repeated every 4 weeks.
Neck dissection is indicated in a very small number of patients who have a residual neck mass 6 to 10 weeks after completion of radiotherapy.
DETAILS OF RADIOTHERAPY
Target Volume
Initial Target Volume
The initial portals encompass the primary tumor and contiguous routes of spread, and the retropharyngeal and cervical nodes. For T1 lesions, the following structures are to be treated: nasopharynx, floor of sphenoid sinus, clivus, pterygoid fossa, parapharyngeal space, retropharyngeal nodes, and bilateral cervical nodes, including level V (spinal accessory) nodes. The extent of nasal cavity and/or oropharynx coverage depends on the contiguous spread of the primary tumor.
For T2 lesions, adjust the target volume to encompass the disease extension in the parapharyngeal space. For T3 to
T4 tumors, adjust the target volume to encompass the disease extension to the clivus, cranial fossa, infratemporal fossa, or hypopharynx. It is important to have generous coverage of the base of skull and known intracranial extension up to the tolerance dose of normal tissues. Intensity- modulated radiation therapy (IMRT) allows better coverage of the primary tumor or retropharyngeal nodes while maintaining normal tissues below unacceptable dose levels.
T4 tumors, adjust the target volume to encompass the disease extension to the clivus, cranial fossa, infratemporal fossa, or hypopharynx. It is important to have generous coverage of the base of skull and known intracranial extension up to the tolerance dose of normal tissues. Intensity- modulated radiation therapy (IMRT) allows better coverage of the primary tumor or retropharyngeal nodes while maintaining normal tissues below unacceptable dose levels.
Boost Volume
The boost portals cover gross disease sites with 0.5- to 1-cm margins, depending on the type of adjacent normal tissues. In case of tumor extension through the clivus, the margin on the brain stem can be only a few millimeters to avoid delivery of >60 Gy to this critical structure.
Dose
With the conventional technique, 50 Gy is given in 25 fractions to regions at risk for harboring subclinical disease, followed by a boost dose of 16 to 20 Gy in 8 to 10 fractions to the primary tumor and involved node(s), depending on the size.
Case Study 7-1
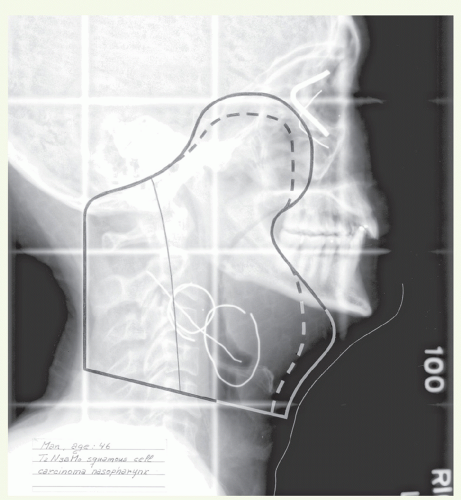
A 46-year-old man presented with a 3-week history of sinusitis, nasal congestion, and a left neck mass. An excisional biopsy of this neck mass showed squamous cell carcinoma. He was referred to our institution for workup and treatment. Physical examination revealed an erythematous mass in the nasopharynx centered on the right posterolateral wall and extending across the midline. The left posterior oropharyngeal wall was swollen consistent with enlarged retropharyngeal nodes. The nasal cavities were unremarkable. Neck examination showed a wellhealed scar in the left subdigastric region with underlying residual adenopathy. A 3.5 × 2.5 cm node and a 2-cm node were palpated in the right subdigastric area. A CT scan confirmed the physical findings and showed that the base of skull was uninvolved. A biopsy from the nasopharyngeal lesion showed poorly differentiated squamous cell carcinoma. Stage: T1, N2, M0. This patient received primary radiotherapy according to the concomitant boost schedule.
The primary tumor and upper neck nodes were treated with lateral-opposed photon fields (Fig. 7.1). The lateral orbital canthi and external auditory canals were marked along with the upper neck scar and palpable neck nodes. The mid and lower neck nodes were treated through an anterior appositional photon field with a midline block to shield the larynx and spinal cord. The dose to the primary tumor and involved neck nodes was taken to 72 Gy in 42 fractions over 6 weeks. Areas of subclinical disease received 54 Gy in 30 fractions over 6 weeks. Because the nodal biopsy site on the palpable left and the nodes on the right side were partly in the electron fields supplementing the posterior cervical areas, these fields were also taken to a total dose of 72 Gy. To deliver an adequate dose to the involved nodal areas, 12-MeV electrons were used and the dose was specified at the 90% isodose line.
With IMRT, 66 to 70 Gy is given to CTVHD and 60 Gy to CTVID in 33 fractions. The fraction size varies from 1.8 Gy to the CTVID to 2.12 Gy to the CTVHD.
Setup and Field Arrangement for Conventional Radiotherapy Technique
The patient is immobilized in a supine position. Marking of lateral canthi, external auditory canals, and palpable nodes may facilitate portal design. With conventional technique, the primary tumor and upper neck nodes are irradiated with lateral-opposed photon fields (see Case Studies 7-1 and 7-2).
Anterior border: Posterior one third to one half of the nasal cavities, depending on the size of the lesion (or 2 cm beyond tumor extension). Usually, most of the oral cavity can be shielded by shaping the field with a notch below the soft palate.
Superior border: At the floor of the pituitary fossa and just above the clivus for T1 to T2 lesions. An initial margin of 2 cm is taken beyond tumor extension into the clivus or intracranially for T3 to T4 disease.
Posterior border: Just behind the spinous processes, or more posteriorly when large spinal accessory nodes are present.
Inferior border: The inferior border is placed just above the arytenoids. When more advanced neck disease is present, it is preferred to junction therapy through the nodes above the larynx.
After off-cord reduction treatment, continue with the posterior border placed over the posterior one third of the vertebral bodies to ensure adequate coverage of the posterior pharyngeal wall and retropharyngeal nodes. It may be necessary to use oblique lateral fields in the presence of retrostyloid parapharyngeal extension of primary disease
or large retropharyngeal node(s). Patients with bilateral retrostyloid parapharyngeal extension present a particularly difficult technical problem in covering the extent of the disease without overdosing the medulla and upper cervical spinal cord without the use of conformal techniques.
Case Study 7-2
A 52-year-old woman presented with pressure-like sensation in her left ear. Further workup revealed a polypoid mass centered and confined to the roof of the 2asopharynx. A biopsy was positive for World Health Organization (WHO) type 3 NPC. There was no adenopathy. Staging workup included MRI, which confirmed that the lesion was confined to the nasopharynx. Stage: T1, N0, M0.
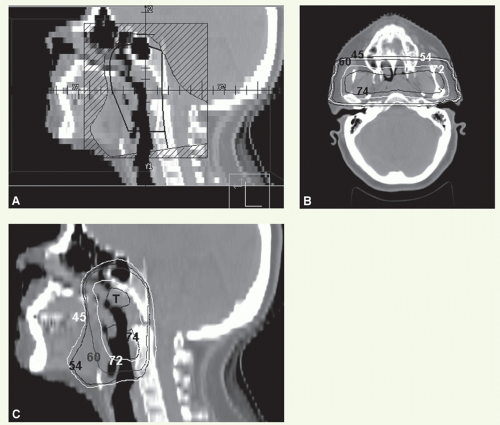
This patient received primary radiotherapy according to the concomitant boost schedule. The primary tumor and upper neck nodes were treated with lateral-opposed photon fields using 6 MV photons.
Figure 7.2A shows a digitally reconstructed sagittal view through the nasopharyngeal mass shown overlaid by a representation of the lateral primary, off-spinal cord, and boost portals. The initial fields were reduced off the spinal cord at 41.4 Gy. The off-spinal cord fields continued to 54 Gy. The posterior cervical strips were treated with 9-MeV electrons to 54 Gy. The boost was delivered as second daily fractions with 18-MV photons to 18 Gy in 12 fractions, bringing the total dose to the tumor to 72 Gy. Isodose distributions of the lateral photon fields through the nasopharynx are shown in both axial (Fig. 7.2B) and sagittal (Fig. 7.2C) views. The mid and lower neck nodes were treated through an anterior appositional photon field with a midline block to shield the larynx and spinal cord. Areas of subclinical disease received 54 Gy in 30 fractions over 6 weeks.
An anterior appositional portal is used for the mid neck and lower neck. If there is nodal disease in the posterior midcervical chain, a posterior field is added to supplement the dose to this area (see “General Principles”).
For the boost volume, lateral fields are reduced to include the primary tumor and involved upper neck nodes.
Superior border: adjusted to exclude the optic nerves, chiasm, and tracts after a dose of 54 Gy.
Anterior border: 1 to 1.5 cm beyond gross disease.
Posterior border: over the posterior one third of the vertebral bodies. Proper margins for the boost volumes are taken to encompass all clinically or radiologically apparent disease extension. These margins may be extremely tight posteriorly for tumors invading through the skull base or brain to avoid brain stem injury.
Inferior border: depends on the nodal status. If N0, the inferior border is at the level of the midtonsillar fossa (more inferior if the oropharynx is involved). If upper neck nodes are involved, the border is above the arytenoids.
As with the initial off-cord reduction, it may be necessary to use oblique lateral fields to cover retropharyngeal or parapharyngeal disease.
Electron fields or glancing photon fields are used to boost the nodes in the mid and lower neck. In cases where both the posterior strip and the mid neck need to be boosted, a single L-shaped electron field is typically used.
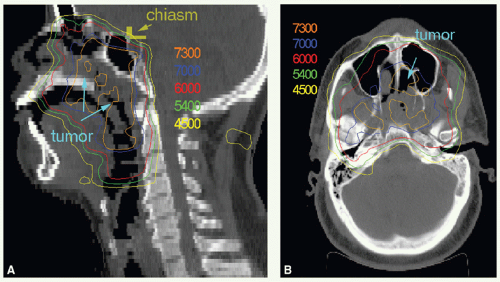
Case Study 7-3
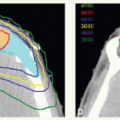
A 44-year-old man presented with nasal obstruction. He was found to have a rather bulky nasopharyngeal tumor extending into the nasal cavity and left parapharyngeal space without clinical lymphadenopathy (stage T2, N0). A biopsy revealed NPC, WHO type 2. He received concurrent IMRT and cisplatin followed by adjuvant chemotherapy. Isodose distributions on a sagittal (Fig. 7.3A) and axial (Fig. 7.3B) image are shown. A dose of 70 Gy was delivered to the CTVHD (GTV plus margin) and 60 Gy to the CTVID (a wider margin around CTVHD, including the clivus and neck nodes), all given in 33 fractions. The lower neck was treated with a matching anterior portal to 50 Gy in 25 fractions. Examination at the completion of external beam therapy revealed questionable residual disease. Therefore, two high-dose-rate brachytherapy applications, each delivering 5 Gy, were administered. He remains without evidence of disease more than 2 years after completion of therapy.
Intensity-Modulated Radiation Therapy
IMRT is gaining popularity for the treatment of NPC, but careful target volume delineation is crucial with this technique, which requires acquisition of thin-cut planning computed tomography (CT) scans for outlining the gross target volume (GTV), clinical target volumes (CTVs), and planning target volumes (PTVs), for dosimetric planning (see Case Studies 7-3, 7-4, 7-5, 7-6, 7-7, 7-8 and 7-9). Because magnetic resonance imaging (MRI) is generally better for delineating the disease extent, particularly at the skull base region, it is crucial to incorporate diagnostic MRI findings into the planning process, preferably by fusion.
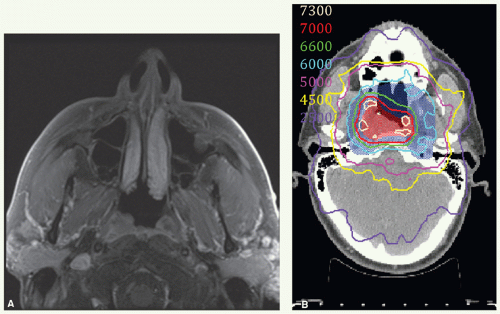
Case Study 7-4
A 58-year-old man presented with a right upper neck mass. Examination revealed a 3-cm upper jugular node and a lesion in the right fossa of Rosenmüller.
An axial MRI image demonstrates a small tumor on the right torus tubarius ablating the fossa of Rosenmüller (Fig. 7.4A). Biopsy of the primary tumor showed an undifferentiated carcinoma, WHO type 3. He was staged T1, N1, M0 and treated with IMRT and three cycles of high-dose cisplatin.
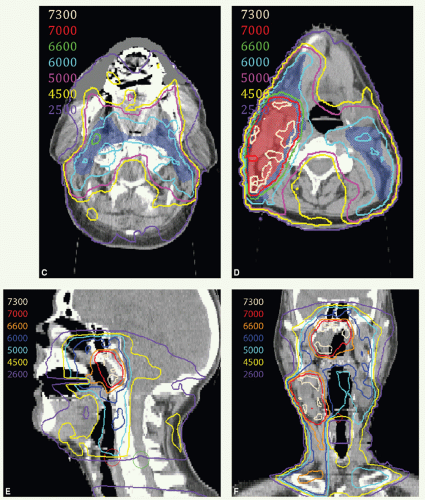
Gross tumor in the nasopharynx and neck with margin were identified as CTVHD (70 Gy). Additional margin was added to cover the inferior sphenoid sinus, clivus, posterior ethmoid and maxillary sinuses, posterior nasal cavity, and medial masticator space and defined as CTVID (60 Gy). In addition, the upper neck and retropharyngeal nodes outside the CTVHD were included in CTVID. Isocenter was placed above the thyroid notch, and the low neck was treated with a matching anterior beam. A larynx block was used for the first 40 Gy, and then a full midline block was added for the remaining 10 Gy. The right lower neck received an additional 10 Gy, to a total of 60 Gy, with glancing photon fields. Figures 7.4B, C-F show isodose distributions of the treatment plan. Axial isodose distributions are demonstrated through the nasopharynx (Fig. 7.4B), retropharyngeal region at C1 (Fig. 7.4C), and upper neck (Fig. 7.4D). CTVHD (70 Gy) is shown in red colorwash and CTVID (60 Gy) in blue colorwash. Sagittal (Fig. 7.4E) and coronal (Fig. 7.4F) distributions are shown through midline and gross disease, respectively. He also received adjuvant chemotherapy with cisplatin and fluouracil. He remains without disease and with good function 3 years later.
Case Study 7-5
A 53-year-old woman presented with a left upper neck mass, otalgia, and sore throat. Fine-needle aspiration was nondiagnostic, so an incisional nodal biopsy was performed, which revealed poorly differentiated squamous cell carcinoma. Examination revealed fullness in the left neck and a lesion in the left side of the nasopharynx, obliterating the fossa of Rosenmüller and eustachian tube.
An axial PET-CT scan demonstrated the tumor in the left nasopharynx (Fig. 7.5A) and, at more inferior section (Fig. 7.5B), left -sided adenopathy in the upper neck. Imaging also demonstrated the primary tumor extending into the retropharyngeal space, bilateral retropharyngeal adenopathy, and a small right level II node. She was staged T2, N2, M0 and treated with IMRT and three cycles of high-dose cisplatin.
CTVHD (70 Gy, red) and CTVID (60 Gy, blue) were delineated (Fig. 7.5C-F




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree