Neck Node Metastasis from Unknown Primary
Key Points
A thorough search for a primary site is a requisite part of the staging workup and should include an examination under anesthesia, appropriate biopsies of subsites within the pharyngeal axis, and/or tonsillectomy.
Radiation is recommended in either the frontline or the adjuvant setting to obtain or maintain regional control.
In the absence of randomized trials, radiation target volumes remain controversial. Many centers recommend comprehensive treatment to bilateral neck lymphatics and putative sources of the primary site, principally the nasopharynx and oropharynx with or without the hypopharynx.
Early data of IMRT suggest favorable outcomes with regard to disease control and reduced toxicity.
TREATMENT STRATEGY
The diagnosis is usually established by a nodal biopsy or aspiration, which should be followed by an examination under anesthesia, with biopsy of suspicious potential primary sites. Tonsillectomy is usually performed in the absence of suspicious lesions. Historically, after completion of the workup, a neck dissection was performed often followed by postoperative radiation when more than one node is involved, particularly in the presence of extranodal extension. The more common practice today, as many patients present with human papillomavirus (HPV)-associated disease, is to begin with radiation, with concurrent chemotherapy in the presence of large nodal volume or CT evidence of extranodal extension, and perform a neck dissection if the nodal disease does not regress completely. Many centers currently recommend irradiation to the pharyngeal axis and the bilateral neck. Some favor omitting the larynx and hypopharynx. Intensity-modulated radiation therapy (IMRT) may allow comprehensive bilateral therapy while providing parotid sparing.
Irradiation to the ipsilateral neck alone is indicated if the histologic findings (e.g., adenocarcinoma) or nodal location (e.g., submenal, submandibular, supraclavicular) indicate a low probability of a primary along the pharyngeal axis. It may also be considered when, because of advanced age or poor medical condition, the patient is not expected to tolerate large-volume irradiation to the pharyngeal axis but residual disease is present or the probability of progression in the neck is high (e.g., presence of extracapsular nodal disease).
Close observation can be considered in patients who had neck dissection, which reveals low risk for recurrence (i.e., a single lymph node <3 cm without extracapsular extension [ECE]).
COMPREHENSIVE RADIOTHERAPY
Target Volume
Initial Target Volume
The initial target volume is composed of oropharynx, nasopharynx, and bilateral neck nodes when the clinical or histologic features suggest primary site origin from the oropharynx or nasopharynx. For example, a nonsmoker with a level II node, particularly with cystic squamous
cell carcinoma, nonkeratinizing “nasopharyngeal-like,” or undifferentiated carcinoma or carcinoma that is positive by HPV in situ hybridization or pl6 immunohistochemical assay would strongly favor an oropharyngeal primary tumor. The presence of involved upper posterior cervical (level V) nodes suggests a nasopharyngeal primary.
cell carcinoma, nonkeratinizing “nasopharyngeal-like,” or undifferentiated carcinoma or carcinoma that is positive by HPV in situ hybridization or pl6 immunohistochemical assay would strongly favor an oropharyngeal primary tumor. The presence of involved upper posterior cervical (level V) nodes suggests a nasopharyngeal primary.
In other cases, the initial target volume encompasses nasopharynx, oropharynx, hypopharynx, and bilateral neck nodes (see Case Studies 16-1 and 16-2).
The boost or high-dose volume encompasses the involved nodal bed.
Case Study 16-1
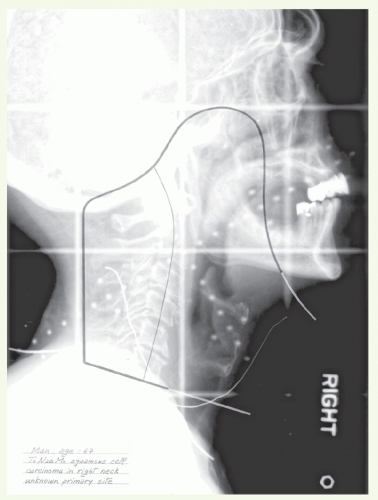
A 67-year-old man consulted his physician for mild hoarseness. He was found to have leukoplakia on both true vocal cords. Examination of the neck revealed a 2-cm mobile lymph node in the right midjugular region. A fine-needle aspiration from this node showed poorly differentiated squamous cell carcinoma. A computed tomography (CT) scan confirmed the lymphadenopathy in the right jugular chain. An examination under anesthesia showed no abnormalities except for leukoplakia on both true vocal cords. Biopsy specimens were taken from the nasopharynx, tonsils, base of tongue, and both true vocal cords. All results were negative for malignancy. The biopsy specimens of the vocal cords showed only hyperkeratosis. The patient then underwent a right modified radical neck dissection. Histologic examination showed poorly differentiated squamous cell carcinoma in two of the 13 lymph nodes, one located in the midjugular area and the other one at the midposterior cervical chain. There was ECE from the midjugular node. Stage: TO N2b MO. Subsequently, this patient received postoperative radiotherapy.
The entire pharyngeal axis and the upper and mid neck were treated bilaterally with opposed-lateral fields, as shown in Figure 16.1. The lower neck nodes were treated with an anterior appositional field. A total dose of 54 Gy was delivered, and then the right neck received an additional irradiation dose of 63 Gy with an appositional electron field.
Case Study 16-2
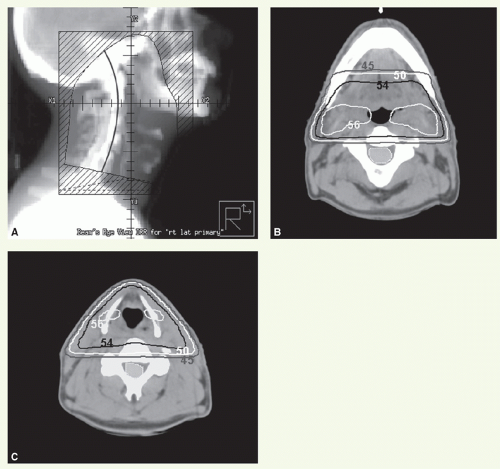
A 50-year-old man presented with bilateral cervical adenopathy (multiple left neck nodes and a 1.5-cm right neck node). He underwent an examination under anesthesia, which did not reveal any primary tumor. Biopsy specimens of both tonsils, the nasopharynx, base of tongue, vallecula, and pyriform sinuses were negative for neoplasm. The patient then underwent bilateral neck dissections. The left neck dissection revealed four of 34 nodes positive for poorly differentiated carcinoma (levels 2 and 3), whereas the right neck dissection was negative for metastases. Stage: TO pN2b MO. He received radiotherapy to both necks and the pharyngeal axis.
Figure 16.2A shows a digitally reconstructed radiograph of the opposed-lateral field is shown. Radiation was delivered with 6-MV photons in 1.8-Gy fractions to a dose of 54 Gy, with an off-spinal cord reduction to 41.4 Gy. A 3-mm tissue equivalent bolus material was placed over the scar. The posterior strips were supplemented with 9-MeV electron beams. Wedges were used to obtain a more homogenous distribution. Isodose distribution of the parallel photon beams at the level of the upper (Fig. 16.2B) and mid necks (Fig. 16.2C) is shown. The low neck was treated with a separate anterior field.
Setup and Field Arrangement
The patient is immobilized in a supine position with a thermoplastic mask. Marking of surgical scar facilitates portal design. For 3D radiotherapy, the initial target volume is irradiated with lateral-opposed photon fields.
Superior border: at mid sphenoid sinus or at the bottom of the pituitary fossa to encompass the roof of the nasopharynx.
Anterior border: include posterior third of the nasal cavities and the anterior tonsillar pillars; 1-cm fall-off for the dissected neck.
Posterior border: behind the spinous processes or more posteriorly to encompass the scar.
Inferior border: just above the arytenoids or below the cricoid cartilage, depending on whether the hypopharynx is part of the target volume.
A matching anterior appositional photon field is used to treat the cervical and supraclavicular nodes below the lateral portals. The boost dose is usually delivered through one or two lateral appositional electron fields. The electron energies are selected based on the depth required to reach the target bed. If the depth is beyond the reach of electrons, glancing photon fields can be used.
Dose
The dose to the initial target volume is 54 Gy in 30 fractions. The boost dose is an additional 6 to 10 Gy in three to five fractions in the postoperative setting. The boost dose can be delivered as a concomitant boost as second daily fractions, with a minimal interval of 6 hours, during the last week of the basic treatment course. In cases of gross nodal disease, a boost dose of 16 Gy in eight fractions (or in 10 fractions if boost dose is given as second daily fractions) is delivered.
Intensity-Modulated Radiation Therapy Planning
Most patients are now treated with IMRT to spare parotid function (see Case Study 16-3). In the event of gross nodal disease, the nodes with 1 -cm margin are outlined as high-dose clinical target volume (CTVHD or CTV1). The neck compartments outside CTVHD with a 2-cm margin are delineated as CTVID (CTV2). The remaining ipsilateral nodal levels (IB, II, III, IV, and V) on the ipsilateral side, retropharyngeal nodes,
and contralateral nodal levels II to V are contoured as CTVED (CTV3). The pharyngeal axis (including the hypopharynx and larynx when indicated) is also delineated as CTVED (see Case Study 16-4).
and contralateral nodal levels II to V are contoured as CTVED (CTV3). The pharyngeal axis (including the hypopharynx and larynx when indicated) is also delineated as CTVED (see Case Study 16-4).
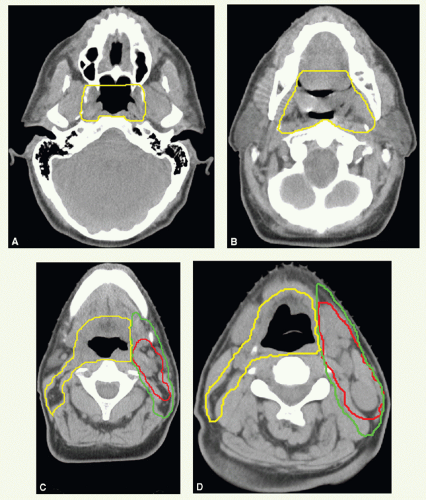
Case Study 16-3
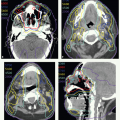
A 50-year-old man, with no history of tobacco consumption, presented with an asymptomatic left neck mass. A fine-needle aspiration of this mass revealed squamous cell carci noma. An examination under anesthesia, with biopsies of the larynx, base of tongue, pharyngeal wall, and nasopharynx, revealed normal-appearing mucosa. CT scan showed two enlarged lymph nodes in level II with additional subcentimeter nodes. Stage: TO N2b MO.
He was treated with IMRT to a dose of 66 Gy to the involved nodes with margin (CTVHD—red), 60 Gy to the remaining uninvolved ipsilateral upper neck nodes (CTVID—green), and 54 Gy to clinically uninvolved contralateral nodes and mucosa of the pharyngeal axis (CTVED—yellow) in 30 fractions. The spinal cord dose was limited to <45 Gy.