Neuroradiology: Head and Neck
Lubdha M. Shah
Richard H. Wiggins III
Case 7.1
HISTORY: A 40-year-old man with neck swelling.
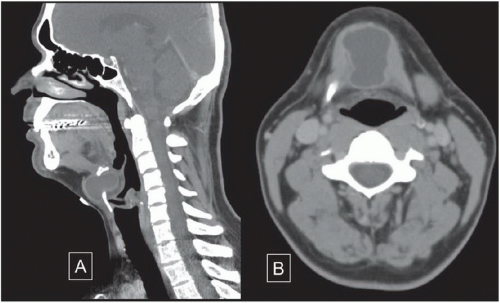
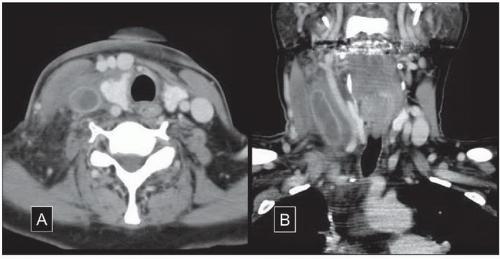
FINDINGS: Sagittal reconstruction post-contrasted CT of the cervical soft tissues demonstrates a well-circumscribed homogeneous midline cystic lesion, between the hyoid bone and the thyroid cartilage without surrounding aggressive features (Fig. 7.1.1A). Axial standard algorithm CECT image at a level between the hyoid and thyroid cartilage shows the midline well-circumscribed mass embedded within the anterior strap musculature (Fig. 7.1.1B).
DIAGNOSIS: Thyroglossal duct cyst.
DISCUSSION: In the third week of fetal life, the thyroid primordium originating at the level of the foramen cecum descends in the neck. It penetrates through the underlying mesoderm of the tongue and floor of mouth musculature, passes anterior to the hyoid bone and laryngeal cartilages, and reaches its final position anterior to the thyrohyoid membrane and strap muscles by the seventh week of gestation (1). This thyroid anlage is connected to the tongue by the thyroglossal duct (TGD), which normally involutes by eighth to tenth week of gestation. Portions of the thyroglossal duct may persist and secretions from the epithelial lining may give rise to a cystic lesion, known as a thyroglossal duct cyst (TGDC) (2). The thyroglossal duct is closely associated with the hyoid bone, which explains why most TGD cysts are located at the level of the hyoid bone (15%) or in the strap muscles immediately inferior to it (65%) (3,4).
This cystic lesion is located either midline at the level of the hyoid bone or slightly off midline within the strap muscles. It has well-circumscribed smooth margins with homogeneous low fluid-like attenuation on CT. Internal areas of high attenuation may be due to increased protein content, possibly due to prior infection. There may be peripheral rim enhancement (5). Similarly, on MRI the signal intensity is fluid-like: T1 hypointense and T2 hyperintense. A thick enhancing rim may be due to infection/inflammation.
Aunt Minnie’s Pearls
The thyroglossal duct cyst is one of the most common incidental lesions found on cervical soft tissue CT studies.
If you look closely, you will frequently see small cystic lesions near the hyoid bone, often with a small osseous defect in the midline of the bone.
If there is irregular nodularity or weird chunky calcifications associated with the cyst, be sure to consider a thyroid carcinoma.
Case 7.2
HISTORY: 37-year-old man with right jaw mass.
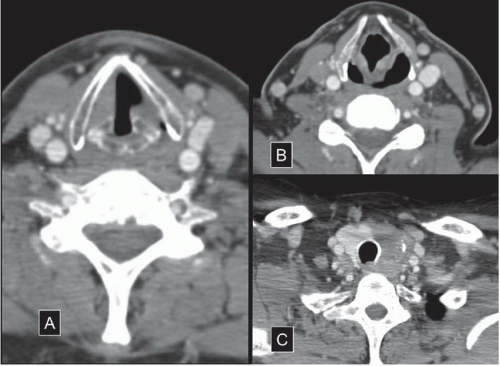
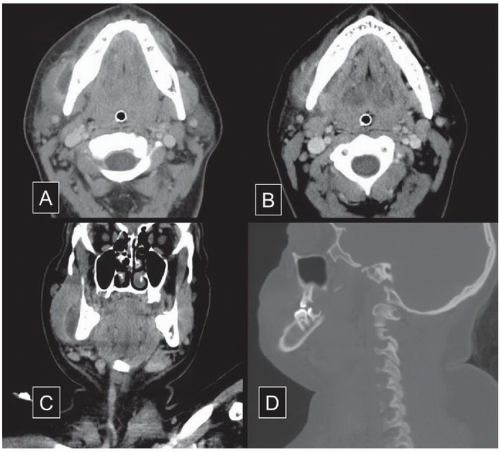
FINDINGS: Axial standard (A) and bone (B) algorithm images obtained at a level immediately below the mandible demonstrates a focal high density lesion within the left submandibular gland (SMG) (Fig. 7.2.1). The gland itself shows no inflammatory changes. A small radiodense marker on the skin surface overlying the mass demarcates the location of the patient’s pain. The coronal (C) standard algorithm image and the oblique sagittal (D) bone algorithm images show that there are several lesions extending along the expected course of the left SMG duct.
DIAGNOSIS: Submandibular gland lithiasis.
DISCUSSION: Sialolithiasis occurs in the submandibular gland 80% of the time (6) in part due to its anatomy. The submandibular gland has a wider lumen but tighter orifice. It also lies in a dependent position with uphill course of the submandibular duct (Wharton’s duct) (7). Wharton’s duct extends from the submandibular gland to the posterior edge of the mylohyoid muscle. It then curves around the muscle and enters the sublingual space on the surface of the mylohyoid muscle and drains into the sublingual papilla (8). The viscous secretions are also contributory to the formation of sialoliths. Obstruction of a duct by a calculus can result in painful swelling of the submandibular gland due to secretion and stasis of saliva. Different imaging modalities can be used to evaluate the large salivary glands including conventional sialography, ultrasonography, computed tomography (CT), digital sialography, and digital subtraction sialography. However, approximately 10% to 20% of sialoliths in the submandibular gland or duct are not radiopaque and, therefore, are not visible on radiographs (8). In addition, phlebolithiasis and hemangiomas with
calcifications or calcified lymph nodes may mimic sialoliths on radiographs. Calculi are readily detected by CT and ultrasound, which have a reported high sensitivity and specificity (9,10). Newer imaging techniques include MR sialography (8).
calcifications or calcified lymph nodes may mimic sialoliths on radiographs. Calculi are readily detected by CT and ultrasound, which have a reported high sensitivity and specificity (9,10). Newer imaging techniques include MR sialography (8).
Aunt Minnie’s Pearls
Calcifications can be found anywhere along the course of the submandibular gland duct, extending along the ipsilateral sublingual space.
If there are inflammatory changes seen to the SMG itself, you should look along the expected course of the duct for a possible calcific stone.
It is important in these cases to try to differentiate a mass lesion arising within the gland from inflammatory changes of the entire gland.
An obstructed SMG duct can lead acutely to abnormal enhancement and enlargement of the gland early, and fatty replacement and decrease gland size in chronic cases.
Case 7.3
HISTORY: 55-year-old man with persistent hoarseness.
FINDINGS: Multiple axial post-contrasted standard algorithm CT images through the cervical soft tissues (Fig. 7.3.1). An image through the level of the vocal cords demonstrates asymmetry of the vocal cords with slight widening of the thyroarytenoid groove (A). A slightly higher axial image (B) shows thickening and anteromedialization of the left aryepiglottic fold and enlargement of the pyriform sinus. A lower section through the thyroid gland (C) demonstrates an aggressive lesion of the left lobe of the thyroid with heterogeneity and extension posteriorly into the left tracheoesophageal groove.
DIAGNOSIS: Vocal cord paralysis (VCP).
DISCUSSION: VCP is caused by the dysfunction of the ipsilateral vagus nerve (cranial nerve 10) or recurrent laryngeal nerve. On CT and magnetic resonance imaging (MRI) of the neck, one should look for a constellation of findings: paramedian position of the affected vocal cord, ballooning of the ipsilateral laryngeal ventricle, anteromedial rotation of the arytenoid cartilage, medially displaced and thickened aryepiglottic fold and an enlarged ipsilateral pyriform sinus (11). There may be atrophy of the cricoarytenoid cartilage (12).
Look for a lesion or injury to the vagus nerve from the medulla to the jugular foramen and along the carotid space. It is important to follow the recurrent laryngeal nerves from the subclavian artery on the right and the aortopulmonary window on the left. Also, remember that the recurrent laryngeal nerves ascend to the larynx in the tracheoesophageal groove. CT angiogram may reveal an internal carotid artery dissection. Additional cranial neuropathies may be present depending on the location of the injury/lesion. If there is loss of the ipsilateral pharynx sensation, cranial nerve 9 may be affected. Denervation of the ipsilateral sternocleidomastoid and trapezius is suggestive of cranial nerve 11 injury. The lesion/injury in these cases may be anywhere from the brainstem to the jugular foramen. If a lesion affects cranial nerve 12 in the superior carotid space to the level of the hyoid bone, there may be tongue denervation.
Aunt Minnie’s Pearls
While the vocal cords should normally be symmetric, there can be some asymmetry of the cords with motion or vocalization during the CT scan.
The spinnaker sail sign is the primary finding of cord paralysis, and the secondary signs include those listed above. I often have to draw a picture to explain the spinnaker sail sign shape to our land-locked residents and fellows. So here is a picture of a black spinnaker sail just for you (Fig. 7.3.2) (I made it myself) to compare to the air-filled space on axial section in Figure 7.3.1 (A) on the prior page. Just imagine the sail and the mast are both black (no, seriously, that’s really what it looks like; you can go Google it for yourself).
Case 7.4
HISTORY: A 63 year-old man with left cheek nontender mass.
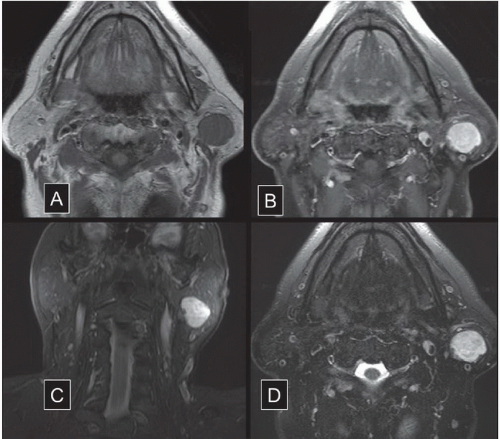
FINDINGS: Multiple MRI images through the face show a well-circumscribed lesion within the left parotid gland. This lesion has low T1 signal intensity before contrast (A) and avidly enhances following contrast administration (B) (Fig. 7.4.1). The coronal T2 FSE with FS (C) and the axial STIR (D) both show very bright T2 signal intensity of this lesion, even brighter than that of the cerebrospinal fluid (CSF) on the T2 FSE FS image. There are no surrounding inflammatory or aggressive changes, and no other lesions are seen.
DIAGNOSIS: Benign mixed tumor
DISCUSSION: Benign Mixed Tumor (aka BMT, pleomorphic adenoma) is the most common epithelial tumor of the parotid gland, comprising 60% to 70% of all salivary gland tumors (13). They can arise from the superficial or deep lobe of the parotid gland in middle-aged patients (slight female preponderance) and tend to be asymptomatic. These lesions are typically solitary, well-circumscribed and slow-growing. Larger masses may have a lobulated contour. The tumor matrix may show calcification or ossification (14), and rarely, these tumors can contain fat (15). On MRI, these lesions have a characteristic T2 hyperintense signal due to the myxoid material; it tends to be as bright as the CSF but may sometimes be heterogeneous due to small areas of fibrosis or calcification. With contrast administration, these lesions show patchy enhancement. These lesions displace adjacent structures, such as compressing muscles toward the mandibular ramus rather than invading them (16).
Aunt Minnie’s Pearls
Lesions within the parotid can be very confusing to evaluate.
The most common mass within the parotid is simply a lymph node, while the most common pathologic lesion is a BMT. These can become large as they slowly grow with benign surrounding changes.
A large benign appearing mass in the deep spaces of the cervical soft tissues that crosses the stylomandibular tunnel (the space between the mandible and the styloid process) is usually a BMT, especially if it is very bright on the T2 imaging— as bright as CSF.
Case 7.5
HISTORY: A 55-year-old woman with pancreatic cancer on chemotherapy through a right chest Chemo-Port complains of right neck edema and pain.
FINDINGS: Post-contrasted axial (A) and coronal (B) CT images through the cervical soft tissues show inflammatory changes within the right neck (Fig. 7.5.1). There are several round structures anterior to the right thyroid lobe with density similar to the main cervical vessels. There appears to be a fluid collection with surrounding enhancement lateral to the right lobe of the thyroid gland and the right common carotid artery. The coronal (B) image shows this tubular lesion to extend superiorly and inferiorly within the right neck.
DIAGNOSIS: Internal jugular vein septic thrombophlebitis.
DISCUSSION: Septic thrombophlebitis refers to venous thrombosis associated with inflammation in the setting of bacteremia (17). It may be associated with use of central venous devices and intravenous therapy. Neoplastic disease often creates a thrombogenic state, through inflammation mediators, tumor necrosis factor, platelet activation, as well as a procoagulant substances released by tumor cells. Furthermore, long indwelling lines increase risk for thrombosis, reported in 0.06% to 32% of patients, although the risk changes with type of catheter, neoplasm, chemotherapy regimes and radiation (18). The thrombus can become infected with persistent bacteremia and septic embolization may occur. Septic thrombophlebitis should be suspected in patients with persistent bacteremia after 72 hours of appropriate antimicrobial therapy, particularly in the setting of an intravascular catheter. Histologic findings consist of inflammation and suppuration within the vein wall. Thrombus with or without pus may be seen within the vein lumen, with evidence of perivascular inflammation. The diagnosis may be made based on culture data together with radiographic evidence of thrombosis. On contrast-enhanced CT, one may detect an intraluminal filling defect in venous structure with a catheter. The proximal or distal segment of vein may opacify with contrast. There is perivascular fat stranding and hazy enhancement of the surrounding tissues. Treatment with only antimicrobials is rarely effective for controlling infection. It is important to remove the focus of infection (e.g., intravenous catheter). Anticoagulation and in some cases a more aggressive approach such as resection of the affected vein (19) or thrombectomy (20) may be needed.
Aunt Minnie’s Pearls
The clinical history here gives the case away, but also reminds of us the importance of clinical information when reading head and neck studies.
Head and neck cases should never be read without clinical history, and that clinical information may completely change the way studies are interpreted.
The anterior collateral venous vasculature in this case also helps to make the diagnosis of jugular vein thrombosis, and the surrounding inflammatory changes tell you that it is thrombophlebitis.
Case 7.6
HISTORY: A 23-year-old woman with right facial swelling and pain.
FINDINGS: Axial post-contrasted CT images through the mandible (A) and at a level through the bottom of the mandible (B) show a fluid collection within the right masticator space, within the right masseter muscle, and wrapping around the bottom of the mandible (Fig. 7.6.1). The coronal (C) reconstruction image shows how the fluid collection wraps around the mandible inferiorly. The sagittal reconstruction (D) with bone window to the right of midline shows the right-sided teeth.
DIAGNOSIS: Odontogenic abscess.
DISCUSSION: An odontogenic abscess most often involves the masticator space but can extend into the adjacent submandibular space. Bone algorithm on CT may show the dental caries and/or the periodontal disease as indicated by periapical lucency with osseous erosion. There may also be periosteal elevation if there is associated osteomyelitis. Contrast-enhanced CT is helpful to delineate the peripherally enhancing abscess and associated phlegmon in the masticator space. The muscles of mastication may be edematous and swollen. Be sure to evaluate the suprazygomatic masticator space as well as the infrazygomatic masticator space for the full extent of the infection.
The acute dental abscess is usually polymicrobial comprising facultative anaerobes, such as viridans group streptococci and the Streptococcus anginosus




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree