Neuroradiology: Spine Imaging
Daniel B. Nissman
Matthew S. Chin
The authors and editors acknowledge the contribution of the Chapter 11 author from the second edition: Mauricio Castillo, MD and the Chapter 6C author from the third edition: Donna R. Roberts
Case 8.1
HISTORY: A 16-year-old male presents with intermittent lower back pain. Scoliosis on physical examination
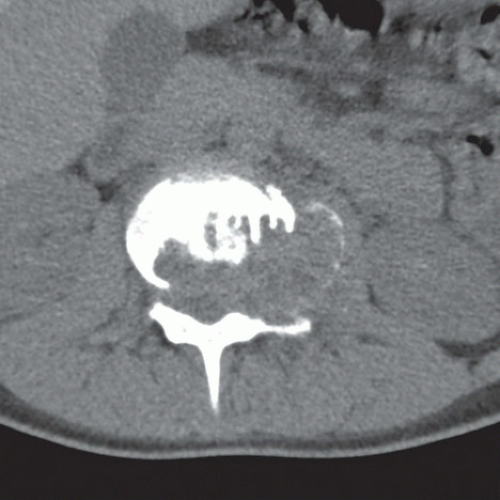
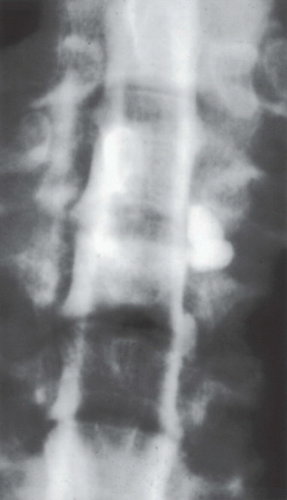
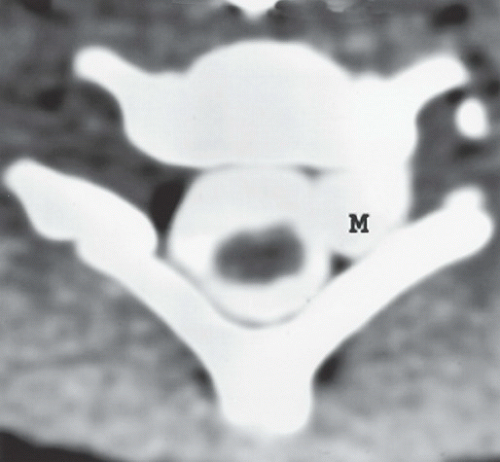
FINDINGS: Frontal radiograph (Fig. 8.1.1) shows an expanded left L2 transverse process with soft-tissue calcification adjacent to it. Subsequent axial CT image (Fig. 8.1.2) demonstrates a lytic lesion in the L2 vertebral body with a sclerotic rim, extending into the posterior elements. On T1-weighted, T2-weighted, and contrast-enhanced magnetic resonance imaging (MRI) sagittal images (Figs. 8.1.38.1.4 to 8.1.5), the heterogeneously enhancing, expansile, L2 vertebral body lesion is causing partial vertebral body collapse and spinal canal stenosis.
DIAGNOSIS: Spinal osteoblastoma
DISCUSSION: Osteoblastomas are rare, benign primary neoplasms of spine and long bones, accounting for 1% of primary bone tumors (1,2). Forty percent occur in the spine, usually the posterior
elements, with an additional 17% diagnosed in the sacrum. Secondary aneurysmal bone cysts are seen between 6% and 10% of osteoblastoma cases (1,3).
elements, with an additional 17% diagnosed in the sacrum. Secondary aneurysmal bone cysts are seen between 6% and 10% of osteoblastoma cases (1,3).
Spinal osteoblastomas are usually diagnosed in young adults (mean age: 20) and have a male predominance (2:1). Symptoms at presentation include back pain or neurological problems. Painful scoliosis may also result from these lesions.
Similar to osteoid osteomas, these lesions comprise osteoid and primitive woven bone, yet differ given their ability to grow >2 cm (average size: 3.2 cm) (1). Unlike osteoid osteomas, they may display rapid resorption of bony cortex, with extension into the surrounding soft tissues. Malignant osteoblastomas have also been reported—with characteristics similar to osteosarcomas (osteoblastoma-like osteosarcoma) (4,5). These malignant-type osteoblastomas demonstrate greater recurrence at prior excision sites as well as disease metastatic to the lungs (6).
Radiographic appearances of osteoblastomas vary (7). The most common pattern is a lytic lesion with multiple small calcifications and a thin sclerotic rim. These lesions may also appear completely lucent with minimal central calcifications. Pseudomalignant features may be present in 25% of the cases, including cortical thinning, expansion of the bone, and the presence of a soft-tissue mass (8). Given the nonspecific radiographic findings, further imaging studies are usually warranted.
CT scans allow characterization of the lesion’s nidus, matrix mineralization, and extent of involvement. With MRI, osteoblastomas have hypointense T1-weighted and hypo-to-hyper-intense T2-weighted signal, relative to bone marrow, based on the amount of ossified matrix material (7). Although limited in its visualization of subtle calcifications, MR allows better visualization of any soft-tissue edema or masses. Percutaneous biopsy will often be performed prior to definitive treatment.
Surgery (curettage or wide excision) is the primary treatment modality. Wide excision is chosen for cases with biopsy or radiographic features of the more aggressive variant. High recurrence rates (up to 24%) have been reported with curettage— significantly less with en bloc resections (1,6). As a result, a wider excision than simple curettage of the lesion may be chosen even in those without more aggressive features. Radiation therapy is controversial, especially given reports of radiation-induced sarcomas, yet utilized in fast growing or recurrent disease (9,10). Few case studies proposed a potential benefit of chemotherapy in aggressive lesions (11,12). Associated aneurysmal bone cysts are usually treated with excision and/or embolization.
Aunt Minnie’s Pearls
Although rare, spine osteoblastomas should be considered when a lucent, sclerotic, or mixed lesion is seen within the spine, the posterior elements in particular.
CT and MRI play complementary roles in its characterization.
Treatment involves curettage or wide surgical excision.
Case 8.2
HISTORY: A 37-year-old man with gradual onset of weakness of the lower extremities and a history of a recent flu-like illness
FINDINGS: Post-contrast, sagittal (Fig. 8.2.1), and axial (Fig. 8.2.2), T1-weighted images of the lumbar spine show contrast enhancement of the ventral roots of the cauda equina.
DIAGNOSIS: Guillain-Barré syndrome (GBS)
DISCUSSION: The diagnosis of GBS is based on clinical features, including weakness, sensory loss, pain, and hypoflexia, or areflexia in the lower extremities. Similar to poliomyelitis, the disease progresses cephalad. After days or weeks, the symptoms plateau and may regress. Some patients show brainstem involvement and may necessitate respiratory support.
Cerebrospinal fluid (CSF) analysis shows only elevated proteins. Current research shows that there are variants of GBS (13). The most common is an acute, inflammatory, demyelinating polyneuropathy (AIDP) for which pathologic examination shows lymphocyte and macrophage infiltration of peripheral nerves with segmental demyelination. Two other subtypes of GBS are acute motor and sensory axonal neuropathy (AMSAN) and acute motor axonal neuropathy (AMAN). These two are known as acute axonal forms, demonstrate marked wallerian degeneration, and have poor prognosis. AIDP is the most common form of GBS in North America and Europe (13). The incidence of AIDP is 1 to 2 cases per 100,000 persons per year, with males affected more often (14). Most cases of AIDP are sporadic, but a preceding infectious episode is common (15). AMAN and AMSAN are more common in the Far East, affect younger patients and occur more frequently during the summer months (14,16). AMAN is, in particular, associated with a recent infection with Campylobacter jejuni (15). The mainstay of treatment is supportive therapy, and other treatments such as plasma exchange, intravenous immunoglobulin, and corticosteroids have shown some efficacy in treating GBS (13). The prognosis is usually good, but 7% to 15% of patients have substantial neurologic deficits. The incidence of death is 5% (16). Overall, 80% of patients recover.
Unenhanced, T1-weighted images may show slightly high signal in the spinal nerve roots (17) but
are nearly always normal (181920). Nerve root enhancement is seen in patients with GBS (17, 20-23). The syndrome has a predilection for the proximal nerve roots (16). Enhancement of the anterior nerve roots without enhancement of the posterior nerve roots suggests GBS, especially in patients without sensory changes (17). Occasionally, the anterior gray-matter horns within the conus medullaris may show enhancement.
are nearly always normal (181920). Nerve root enhancement is seen in patients with GBS (17, 20-23). The syndrome has a predilection for the proximal nerve roots (16). Enhancement of the anterior nerve roots without enhancement of the posterior nerve roots suggests GBS, especially in patients without sensory changes (17). Occasionally, the anterior gray-matter horns within the conus medullaris may show enhancement.
Aunt Minnie’s Pearls
Nerve root enhancement in a patient with an acute onset of rapidly progressive lower-extremity weakness along with appropriate laboratory findings suggest the diagnosis of GBS.
Enhancement of only the anterior rootlets of the proximal cauda equina is generally seen in GBS and in other polio-like variants.
Case 8.3
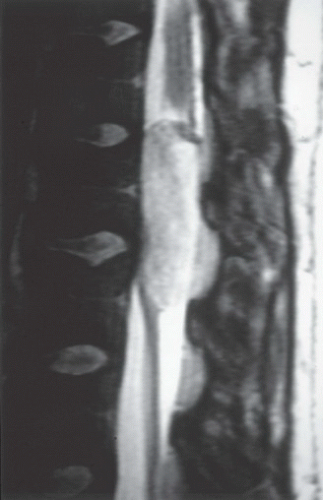
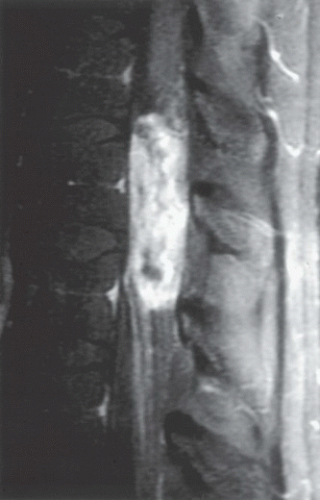
HISTORY: A 47-year-old woman with midthoracic pain, a chronic cough, weight loss, and night sweats
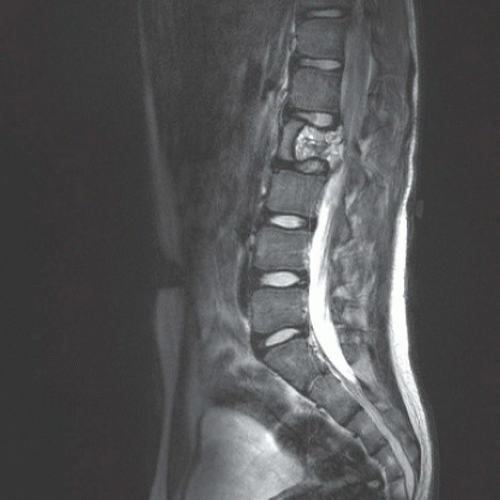
FINDINGS: A sagittal, pre-contrast, T1-weighted MR image (Fig. 8.3.1); corresponding post-contrast image (Fig. 8.3.2); sagittal, T2-weighted image (Fig. 8.3.3); and axial, post-contrast, T1-weighted image (Fig. 8.3.4) show that the disc space at the T9 to T10 level is mostly preserved. There is endplate erosion and erosion of the anterior-inferior corner of T9 and of the anterior-superior corner of T10. An enhancing soft-tissue mass is recognized under the anterior longitudinal ligament. The axial image shows extension into the paravertebral regions and epidural space. There is cord compression.
DIAGNOSIS: Tuberculosis of the spine (i.e., Pott disease)
DISCUSSION: Approximately 3% to 5% of tuberculosis cases involve the skeleton in HIV-negative patients, and 60% of cases are skeletal in HIV-positive patients (24). In cases of skeletal tuberculosis, the spine is most commonly involved. Spinal tuberculosis occurs in 50% of patients with skeletal involvement (25). Untreated spinal tuberculosis can lead to extensive bone destruction and possible compression of the spinal cord. Compared with pyogenic
spondylitis, spinal tuberculosis more commonly leads to paraplegia. The relatively common involvement of the neural arches in tuberculosis contributes to cord compression (24). Spinal tuberculosis usually results from a hematogenous spread to the spine or from direct extension from a paraspinal abscess. Spinal tuberculosis more commonly involves the thoracic and lumbar regions (26,27). Vertebral body destruction begins anteriorly at the superior and inferior end plates, and sclerosis may be seen. Infection spreads under the anterior or posterior longitudinal ligaments.
spondylitis, spinal tuberculosis more commonly leads to paraplegia. The relatively common involvement of the neural arches in tuberculosis contributes to cord compression (24). Spinal tuberculosis usually results from a hematogenous spread to the spine or from direct extension from a paraspinal abscess. Spinal tuberculosis more commonly involves the thoracic and lumbar regions (26,27). Vertebral body destruction begins anteriorly at the superior and inferior end plates, and sclerosis may be seen. Infection spreads under the anterior or posterior longitudinal ligaments.
More than two vertebrae are involved in >50% of patients. Bony erosion anteriorly leads to wedging of the vertebral body, and when multiple segments are involved, kyphosis occurs. Radiographs show indistinctness of the end plates, narrowing of the disc space, and loss of vertebral body height. Erosions and sclerosis of the vertebral body may be seen. Involvement of an entire vertebral body may occur and lead to complete collapse, resulting in a vertebra plana. Large paraspinal abscesses can be seen in the psoas muscles. Occasionally, an abscess may contain a bone sequestrum. Although the focus of infection is usually the anterior portion of the vertebral bodies (27), posterior spinal tuberculosis occurs with an incidence of about 2% to 10% (28). MRI is the preferred modality for evaluating spinal tuberculosis. T1-weighted images show low signal within the vertebral body, and T2-weighted images show high signal owing to bone marrow edema. A thick rim of enhancement around paraspinal and intraosseous abscesses is typical of tuberculosis (26,29). Cold abscesses are usually disproportionately large when compared with the degree of bone involvement. Abscesses tend to be more prominent in children. When tuberculosis involves only a disc, differentiation from a pyogenic infection is not possible. Brucellosis has imaging features similar to those of tuberculosis but more often involves the lumbosacral junction.
Treatment of spinal tuberculosis is predicated on eradication of the infection and correction of any spinal deformity, particularly kyphosis. Spinal tuberculosis can be successfully treated with chemotherapy alone (30). In patients where surgery is indicated, in particular those with kyphotic deformity, anterior or posterior stabilization instrumentation can be placed. Involvement of no more than two vertebral bodies can be stabilized using anterior instrumentation, the first reported method for treating tuberculous involvement of the spine. Multisegment involvement is likely best treated with posterior instrumentation (31).
Aunt Minnie’s Pearls
Large paraspinal abscesses with a thick rim of enhancement accompanied by little bone destruction, particularly in children, suggest tuberculosis.
Isolated destruction of the posterior elements particularly in the cervical region accompanied by adenopathy or abscesses is typical of tuberculosis.
Fluid collections under the anterior or posterior (or both) longitudinal ligaments with involvement of only the anterior aspect of one or more vertebral bodies are suggestive of tuberculosis.
Case 8.4
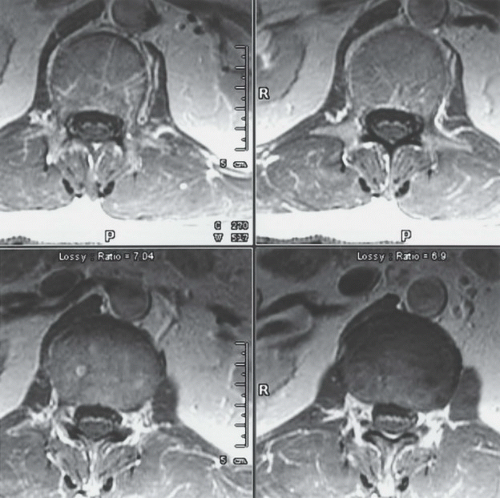
HISTORY: A 34-year-old man with AIDS and back pain (Figs. 8.4.18.4.2 to 8.4.3). Another patient is illustrated in Figures 8.4.4 and 8.4.5
FINDINGS: A sagittal, T1-weighted MR image (Fig. 8.4.1); post-contrast, T1-weighted image (Fig. 8.4.2); and a T2-weighted image (Fig. 8.4.3) show a narrowed L2-L3 disc space with erosion of the end plates. The bone marrow of L2 and L3 has abnormal signal intensity. There is a small, rim-enhancing area of low-signal intensity posterior to the abnormal disc, resulting in narrowing of the spinal canal. On the T2-weighted images, the abnormal disc is bright. Lateral radiograph of the
thoracic spine (Fig. 8.4.4) demonstrates marked end plate destruction centered at a midthoracic disc level. Posterior planar image from a gallium-67 scan (Fig. 8.4.5) demonstrates a corresponding focus of intense radiotracer uptake.
thoracic spine (Fig. 8.4.4) demonstrates marked end plate destruction centered at a midthoracic disc level. Posterior planar image from a gallium-67 scan (Fig. 8.4.5) demonstrates a corresponding focus of intense radiotracer uptake.
DIAGNOSIS: Discitis with epidural abscess (first patient) and discitis alone (second patient)
DISCUSSION: Discitis is an inflammatory process of the intervertebral disc spaces, usually of the lumbar spine. Variable symptoms include fever, abdominal pain, limp, refusal to walk or sit up, and pain in the back, hip, or knee. In adults, infection usually begins at the vertebral body end plates and spreads to the adjacent disc. The opposite occurs in children, whose intervertebral discs are vascularized, with infection spreading to vertebral bodies from an infected disc. An immunocompromised state, advanced age, diabetes mellitus, systemic infection, and genitourinary infection or surgical manipulation predispose to osteomyelitis and discitis (32). Staphylococcus aureus is the most common bacterial cause of spinal osteomyelitis, but other common pathogens include Streptococcus, Enterobacter, Escherichia coli, tuberculosis, Klebsiella, and Salmonella (323334). Radiographs are negative early, but bone scan results are generally positive. MRI is probably the imaging method of choice and allows early identification of the infection and delineation of paraspinal or epidural abscesses in more advanced cases (35). On MRI, the affected disc is always bright on T2-weighted images; degenerated discs are dark on T2-weighted images. The adjacent end plates show low-intensity T1 signal and high-intensity T2 signal. After contrast is given, the disc and adjacent vertebrae enhance. Involvement of other vertebrae begins generally at the level of the canal for the basivertebral vein and is clearly seen on sagittal T2 images. Epidural abscesses usually are found at the level of the infected disc and are seen as masses that enhance peripherally and compress the thecal sac. Occasionally, at the level of an epidural abscess, the spinal cord shows high-intensity T2 signal, probably caused by venous congestion and edema. Diffusion-weighted imaging demonstrates restricted diffusion in pyogenic abscesses of the spine as it does in the brain.
Radionuclide imaging in spinal infections are mostly performed with technetium-99m-labeled diphosphonate bone scans or gallium-67 citrate. Both of these modalities are highly sensitive for infection in the spine but lack specificity. Gallium-67 scans are preferred over indium-111-labeled white blood cells, which have better diagnostic performance outside the spine because the white blood cells have
difficulty reaching the site of infection. Improved specificity can be obtained when gallium-67 scans are interpreted with a three-phase bone scan. Infections are considered to be present when the activity on the gallium-67 scan is greater than that of the bone scan (36). Although MRI has better performance characteristics in the initial diagnostic workup, radionuclide imaging is more specific in the postsurgical and posttreatment setting (37).
difficulty reaching the site of infection. Improved specificity can be obtained when gallium-67 scans are interpreted with a three-phase bone scan. Infections are considered to be present when the activity on the gallium-67 scan is greater than that of the bone scan (36). Although MRI has better performance characteristics in the initial diagnostic workup, radionuclide imaging is more specific in the postsurgical and posttreatment setting (37).
Identification of the causative organism is essential to the proper treatment of discitis osteomyelitis. In the absence of positive blood cultures, percutaneous biopsy of the affected disc and end plates is needed to establish a diagnosis. Unfortunately, approximately only 50% of biopsy specimens yield a positive result. Some have advocated repeat biopsy in these situations (38). Treatment for epidural abscess is surgical evacuation.
Aunt Minnie’s Pearls
MRI allows early identification of infection and delineation of paraspinal or epidural abscesses. The affected disc always has high signal intensity on fluid-sensitive images.
In the postsurgical and posttreatment settings, radionuclide imaging is more specific for infection than MRI.
Percutaneous biopsy is essential to establish the identity of the infecting organism(s) in the absence of positive blood cultures.
In children, discitis is an inflammatory process centered on a lumbar intervertebral disc. Children between the ages of 6 months to 4 years are more frequently affected.
Case 8.5
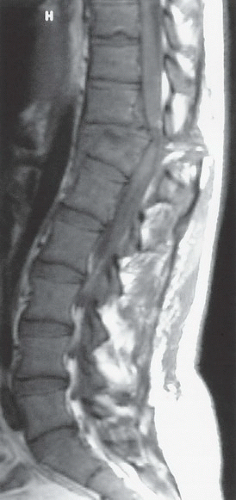
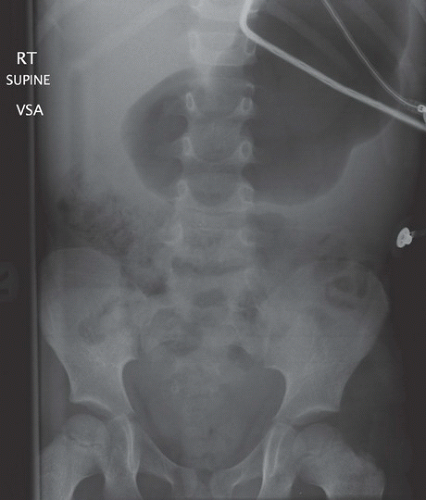
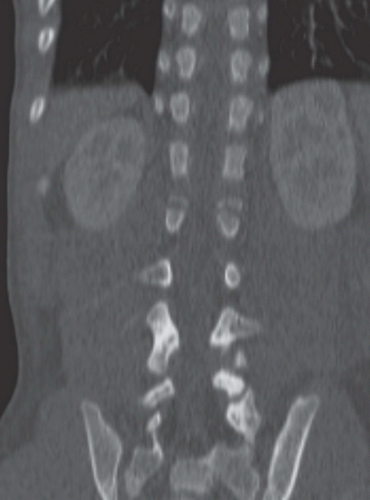
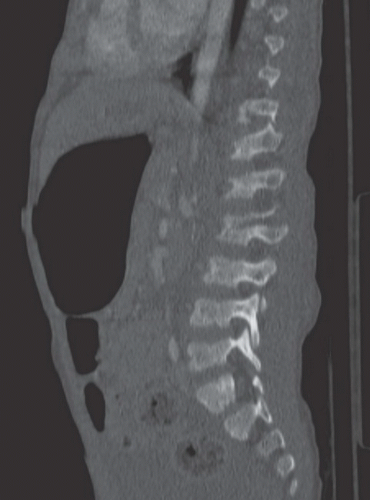
HISTORY: A 10-year-old girl after a motor vehicle crash, during which she was wearing only a lap seat belt (Figs. 8.5.1 and 8.5.2). Figures 8.5.3 to 8.5.5 are from a different patient with the same mechanism of injury
FINDINGS: Sagittal, T1-weighted (Fig. 8.5.1), and T2-weighted (Fig. 8.5.2) images show a fracture dislocation through the T12-L1 level. There is wedge compression deformity of L1 and displacement of bone fragments into the canal, resulting in compression of the spinal cord. The T2-weighted image shows edema of the involved vertebrae and of the cord. Notice the posterior extension (Fig. 8.5.2, arrow) of the fracture. A frontal radiograph of the lumbar spine (Fig. 8.5.3) in a different patient demonstrates a transverse fracture through the vertebral body and pedicles of L2. Coronal CT reformat (Fig. 8.5.4) in this patient demonstrates the same findings. The sagittal CT reformat (Fig. 8.5.5) shows the extension of the fracture line through the posterior elements, including the pedicles.
DIAGNOSIS: Chance-type fracture
DISCUSSION: The Chance fracture, or transverse spinal fracture, is created by forceful hyperflexion of the body against a rigid object some distance anterior to the spine acting as an axis of rotation. Hyperflexion creates a distraction force, resulting in a transverse fracture through the posterior elements and the vertebral body. Chance-type fractures generally occur in the setting of a head-on motor vehicle collision in which the occupant is wearing only a lap-type seat belt or as a consequence of horseback riding accidents. Chance fractures are part of the seat belt syndrome comprising spine injuries in combination with intra-abdominal injuries. In one series of Chance fractures, 44% of patients had substantial intra-abdominal injuries (39). In children presenting with the seat belt sign, 78% had intestinal injuries (40). If an abdominal wall contusion is present in the setting of a Chance fracture, one multicenter study (41) found intra-abdominal injury in 85% of patients. Conversely, they also found that the absence of an abdominal wall contusion was associated with a low chance of intra-abdominal injury (14%). Chance fractures usually involve the thoracolumbar junction, but these fractures can occur anywhere in the thoracic and lumbar spine (39,42). Chance fractures are unstable, but neurological injury occurs infrequently. In a series of 19 patients, 27.7% had neurologic findings (43).
Radiographic findings of Chance fractures can be subtle. Acutely, these fractures may be missed. Pedicles and spinous processes should be examined closely for a break in their cortex indicating fracture. In the lateral view, the fracture may be visualized. Extension of the fracture through the vertebral body may result in irregularity of the superior or inferior end plates. A widened space between the spinous processes with anterior angulation of the vertebral body is suspicious for a Chance fracture. CT findings may also be subtle. In a review of CT scans obtained during a 4-year period, it was found that lap belt-associated injuries of the lumbar spine were missed in five patients (44). Because these fractures occur along the transverse plane, they may be missed on CT scans acquired in the axial projection. Sagittal reconstructions may identify these fractures more clearly. MRI shows the fracture line to have high T2 signal, bone marrow edema, and in many cases, injury to the distal cord and the conus medullaris.
A spectrum of injuries owing to the flexion-distraction mechanism seen in the Chance fracture occurs, ranging from predominantly bony injury to only soft-tissue injury (disc and ligaments). Injuries with an injury pattern different from the classic Chance fracture are known as Chance-type or Chance equivalent fractures (45).
In children, Chance fracture equivalents involving the inferior or superior end plate also occur. The end plates act like physes and may be preferentially injured. In one series, two-thirds of cases involved the end plates, whereas only one-third demonstrated the classic fracture pattern (46).
Aunt Minnie’s Pearl
In any trauma patient with abdominal bruising from a seat belt, search carefully for lumbar spine fractures and intra-abdominal injuries.
Case 8.6
HISTORY: Young patient with left upper-extremity weakness after a motorcycle accident
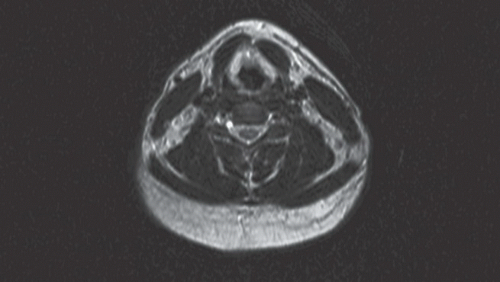
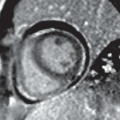
FINDINGS: Frontal view from a cervical myelogram (Fig. 8.6.1) shows a small, contrast-filled, abnormal structure in the lower cervical spine. The postmyelogram axial CT view (Fig. 8.6.2) confirms the presence of the lesion (M). In another patient with right upper-extremity weakness also after a motorcycle accident, an axial T2-weighted MR image (Fig. 8.6.3) shows absence of the right exiting nerve root with a cystic structure in its expected location.
DIAGNOSIS: Cervical pseudo-meningocele owing to traumatic nerve root avulsion
DISCUSSION: Nerve root avulsions result from severe traction on the exiting nerve roots. They are seen most commonly in the cervical spine in association with traction injuries of the arm but can occur in the lumbosacral region with lumbosacral or pelvic fractures. The typical appearance on myelography, CT myelography, or MRI is that of an absent exiting nerve root at the level of the neural foramen (47,48). The avulsed nerve root often retracts laterally, leaving a CSF-filled cavity or pseudo-meningocele in the lateral aspect of the spinal canal extending into the neural foramen and occasionally extraforaminally into the surrounding paraspinous soft tissues. Although pseudo-meningoceles typically fill with contrast introduced into the subarachnoid space, they can occasionally become walled off and manifest as extradural cystic masses. The absence of pseudo-meningoceles on myelography or CT myelography therefore does not exclude an avulsed nerve root. A T2-weighted MR image can demonstrate all pseudo-meningoceles. In rare cases, pseudo-meningocele formation may be associated with spinal cord herniation (495051). Although many nerve root avulsions occur in association with motor vehicle accidents, they also occur during birth from excessive traction on the shoulder (52). With complete nerve root avulsion, nerve regeneration is impossible. However, through recent advancements in surgical techniques, it is possible with microsurgery to reinnervate the brachial plexus by nerve transfer from other peripheral nerves (53).
Aunt Minnie’s Pearls
Severe traction injuries of the arm can lead to nerve root avulsion and pseudo-meningocele formation.
Traumatic avulsions of the cervical nerve roots are more common in newborns and in young men (who are more prone to motor vehicle accidents).
Case 8.7
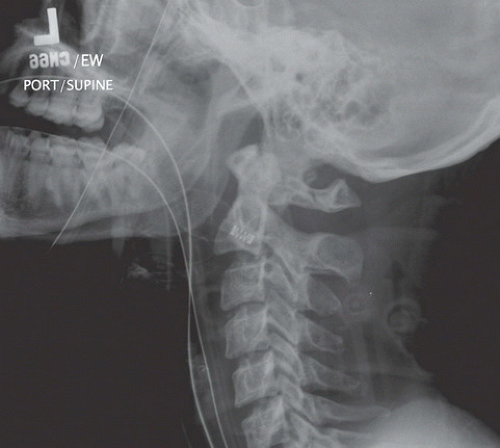
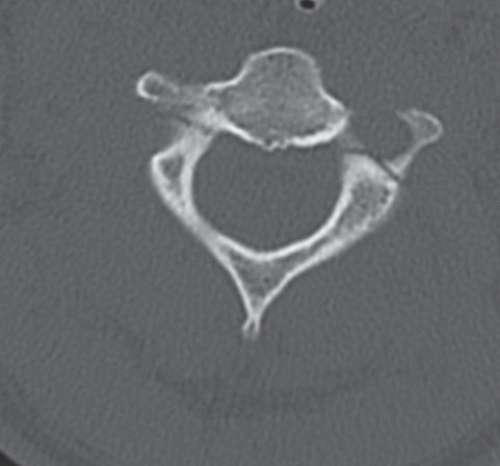
HISTORY: Two patients with cervical spine trauma after motor vehicle collision
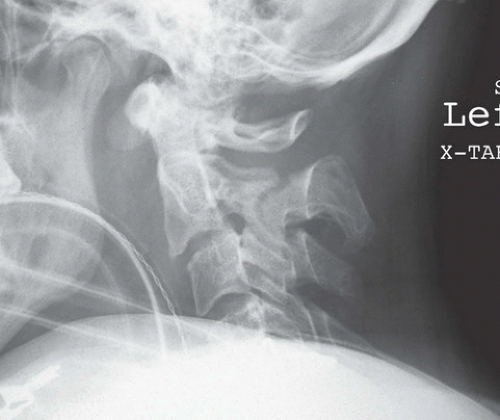
FINDINGS: A lateral radiograph of the cervical spine in one patient (Fig. 8.7.1) demonstrates a bilaminar fracture of the axis with 3-mm anterolisthesis of C2 on C3. In the other patient, lateral radiograph of the cervical spine (Fig. 8.7.2) demonstrates posterior angulation of C2 in relation to C3 with anterolisthesis of 2 mm of C2 on C3. In this same patient, an axial CT image (Fig. 8.7.3) demonstrates bilateral pedicle fractures with involvement of the left transverse foramen. A sagittal T2-weighted MR image (Fig. 8.7.4) demonstrates edema of the spinal cord at the level of the body of C2.
DIAGNOSIS: Traumatic spondylolisthesis of the axis (hangman’s fracture)
DISCUSSION: Traumatic spondylolisthesis of the axis (TSA) is a bilateral fracture of the posterior elements of the C2 vertebra that comprise the neural arch. The degree of instability of the injury is related
to the degree of disruption of the anterior longitudinal ligament and the C2/C3 disc.
to the degree of disruption of the anterior longitudinal ligament and the C2/C3 disc.
Termed a “hangman’s fracture” by Schneider et al. (54), owing to the similarity of the fracture pattern seen in judicial hangings, the mechanism and expected injuries in TSA are quite different from that seen in judicial hangings. Today, motor vehicle accidents, falls, and diving accidents are the most common situations resulting in this type of injury. The most common mechanism is hyperextension with axial compression. Hyperflexion also plays a role, particularly in the more severe injuries. In contrast, the mechanism in judicial hangings using a submental knot is hyperextension with distraction.
A number of radiographic classification systems based on the lateral cervical spine radiograph have been developed to predict degree of instability. The presumption is that a nondisplaced fracture indicates that the anterior longitudinal ligament and disc are intact and that as displacement and angulation increase, the degree of disruption of these structures increases thereby leading to increasing instability. In the two most widely used systems, those of Effendi et al. (55) and Levine and Edwards (56), fractures are graded from 1 to 3 with grade 3 representing the most unstable injury. In both, a type 3 TSA indicates bilateral jumped facets. As positioning after trauma can artifactually reduce the grade of injury, clinical judgment should also be used to determine the degree of instability.
The role of imaging is to determine the type of injury and the presence of complications (57). The lateral cervical spine radiograph is usually sufficient to make the diagnosis of a TSA. The primary role of computed tomography is to evaluate for potential vertebral artery injury and to help identify additional fractures. MRI is used to identify or confirm injury to the spinal cord depending on the clinical situation. Occasionally, lateral flexion and extension radiographs may be of use in determining the stability of the fracture.
Treatment is based on the determination of stability as determined by the classification system in use and the clinical picture (58). Those fractures deemed stable are treated with external fixation: rigid collar or halo vest. Those fractures deemed unstable are treated with anterior cervical fusion.
Aunt Minnie’s Pearls
Traumatic spondylolisthesis of the axis is commonly the result of hyperextension injuries with axial compression. Flexion plays more of a role in severe injuries.
The mechanism in judicial hangings with a submental knot is hyperextension with distraction.
Potential complications include vertebral artery injury and spinal cord injury.
Case 8.8
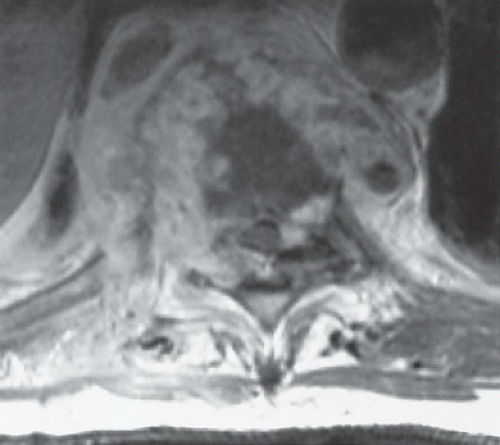
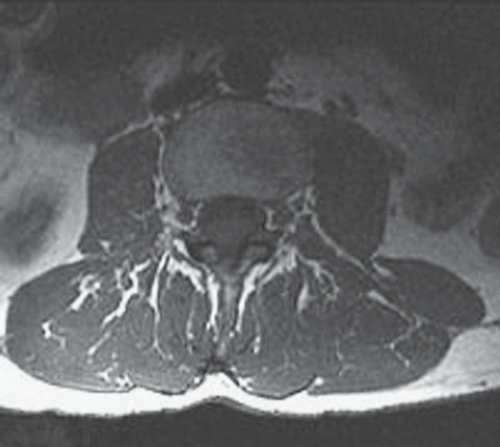
HISTORY: A 35-year-old man with a 3-month history of low back pain and saddle-like distribution anesthesia (Figs. 8.8.1 and 8.8.2). Figures 8.8.3 to 8.8.5 show an example of another subtype of this diagnosis. (Case courtesy of Dr. Aquilla Turk, III)
FINDINGS: Sagittal, T2-weighted (Fig. 8.8.1) and post-contrast, T1-weighted (Fig. 8.8.2) images show an enhancing mass in the region of the conus medullaris with some enhancement of the distal nerve roots. In a different patient, a sagittal T1-weighted post-contrast (Fig. 8.8.3) image shows an enhancing lesion within the distal cord also at the level of the conus medullaris. Axial T1-weighted pre-contrast (Fig. 8.8.4) and post-contrast (Fig. 8.8.5) images demonstrate this lesion to be intramedullary.
DIAGNOSIS: Spinal cord ependymoma, myxopapillary ependymoma
DISCUSSION: Ependymomas are the most common intramedullary tumors in adults, followed by astrocytomas and hemangioblastomas (59). In children, astrocytomas are more common than ependymomas (60). Ependymomas arise from ependymal cells lining the central spinal canal and usually cause symmetric expansion of the cord. Eighty percent of cord ependymomas have associated cysts (61). These are considered to be reactive cysts and are not lined by neoplastic cells but by gliosis. Sixty-seven percent of intramedullary ependymomas occur in the cervical region (62), with extension of the solid portion of the tumor for an average of four vertebral body segments (61,63,64). Unlike astrocytomas that demonstrate infiltrative pathology, ependymomas are generally well-circumscribed lesions, making surgical resection possible (65,66). The myxopapillary variant of ependymoma generally involves the filum terminale (65). Clinically, these patients present with nonspecific back pain or focal neurologic symptoms.
Ependymomas are isointense to hypointense on unenhanced, T1-weighted images and enhance after gadolinium administration (63,64). Sharply marginated enhancement is typical of ependymomas, and this correlates surgically with the margins of the tumor (61). Ependymomas can hemorrhage, and if bleeding occurs along the periphery of the tumor, a hypointense hemosiderin ring will be seen on T2-weighted images. Ependymomas may show blood-fluid levels in their cysts. It has been reported that cervical ependymomas are more likely to hemorrhage (63). Myxopapillary ependymomas have a typical sausage shape, are located in the proximal filum terminale, do not bleed, may extend into the nerve roots of the cauda equina or the conus medullaris, and show enhancement.
Aunt Minnie’s Pearls
A well-enhanced, sharply marginated, centrally located lesion, in the cervical spine in particular, is most likely an ependymoma.
A spinal cord tumor containing a rim of chronic blood products or intratumoral blood is most often an ependymoma.
A sausage-shaped, enhancing tumor in the filum terminale is nearly always an ependymoma. The differential diagnosis includes astrocytoma, paraganglioma, and metastasis.
Case 8.9
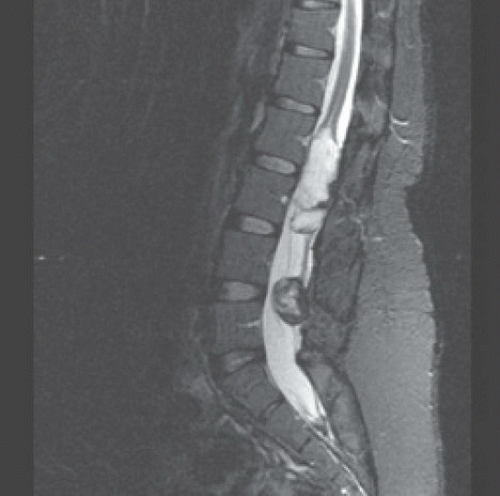
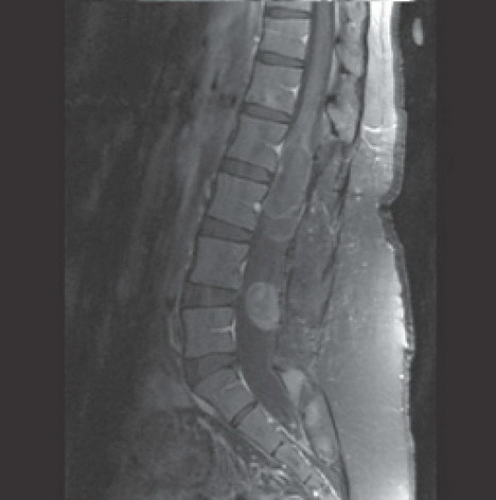
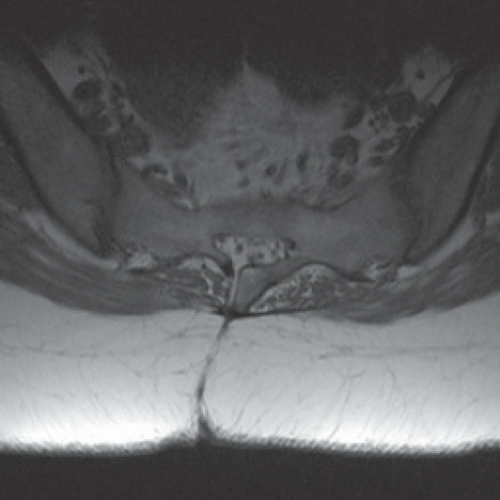
HISTORY: A 26-year-old female presents with recurrent lower back pain, extending into bilateral thighs
FINDINGS: Sagittal T1-weighted, T2-weighted, and contrast-enhanced images show two heterogeneous, low signal on T1-weighted images, predominantly high signal on T2-weighted images, enhancing intradural round lesions at the level of L4-L5 and the conus with a thin filum terminale connecting them (Figs. 8.9.18.9.2 to 8.9.3). Additional axial T2-weighted image of the sacrum (Fig. 8.9.4) demonstrates a subcutaneous dermal sinus tract.
DIAGNOSIS: Spinal dermoid
DISCUSSION: Spinal dermoids are rare, slow-growing dysontogenic tumors that arise from ectopic ectoderm and mesoderm embryonic rests inclusion within the spinal canal at the time of neural tube closure (third-fifth weeks of fetal life) (67). Accounting for approximately 1% to 2% of intraspinal tumors, they occur predominantly in
the lumbosacral region (60%), followed by the thoracic region (10%)—usually residing in an intradural, extramedullary location (68,69). Approximately 20% of spinal dermoids are associated with a dermal sinus tract (67).
the lumbosacral region (60%), followed by the thoracic region (10%)—usually residing in an intradural, extramedullary location (68,69). Approximately 20% of spinal dermoids are associated with a dermal sinus tract (67).
With a slight increased predominance in males, spinal dermoids are usually diagnosed between second and third decades (70). Symptoms result from the lesion’s location, owing to its compressive effect on adjacent structures. The most common presenting symptom is lower back or sciatic pain. Spinal dermoids and tethered cord have been associated with progressive lower neurologic and bladder dysfunction— including postoperative cases of myelomeningocele repair (71). Excluding spina bifida repair, acquired dermoid cysts have also occurred with other procedures (e.g., spinal surgery or lumbar puncture)—likely a result from implantation of epidermal tissue into the subdural space. Rupture of these lesions may cause seizures, chemical (aseptic) meningitis, or arachnoiditis—owing to the spread of lipid droplets throughout the subarachnoid spaces (72).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree