Orbits: Orbital Pathology
PERSISTENT HYPERPLASTIC PRIMARY VITREOUS
KEY FACTS
Refers to a persistent, hyperplastic, embryonic hyaloid vascular system; patients may also have seizures, hearing loss, mental deficiencies, and cataracts.
Persistent hyperplastic primary vitreous (PHPV) is the second most common cause of leukokoria after retinoblastoma.
The affected eye is usually small (microphthalmia).
Computed tomography (CT): hyperdense vitreous, no calcifications; a thin central structure (Cloquet canal) may be seen extending from the posterior retina to the lens; the vitreous may enhance, and retinal detachments may be present.
MRI: T1 and T2 hyperintense (retinoblastoma is usually T2 hypointense); Cloquet canal and fluid levels.
May be indistinguishable from retinal dysplasia occurring with Norrie disease, trisomy 13 syndrome, and Walker Warburg syndrome.
Main differential diagnosis: retinoblastoma, Coats disease, retinopathy of prematurity.
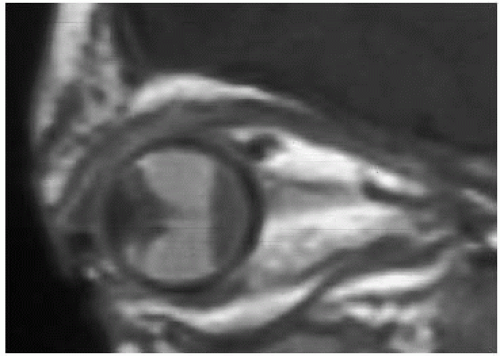
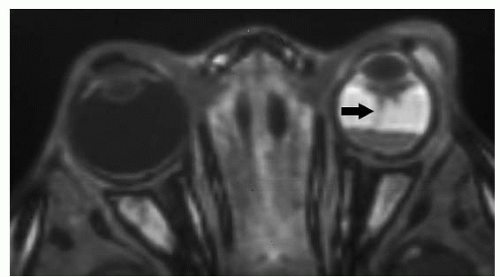 FIGURE 31-1. Axial T1 shows bright left vitreous with a fluid and a central linear canal of Cloquet (arrow). The eye is small. |
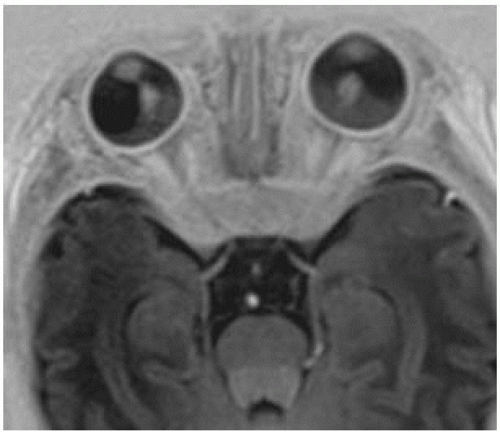 FIGURE 31-3. Axial T1 (inversion recovery) image, in a different patient, shows bilateral detachments that continue anteriorly in the “tentlike” configuration with the canals of Cloquet. |
SUGGESTED READING
de Graaf P, van der Valk P, Moll AC, Imhof SM, Schouten-van Meeteren AYN, Castelijns JA. Retinal dysplasia mimicking intraocular tumor: MR imaging findings with histopathologic correlation. Am J Neuroradiol 2007;28:1731-1733.
GLOBE CALCIFICATIONS
KEY FACTS
Calcifications are related to deposition of calcific hyaline-like material at the surface or deep within the optic disc (drusen bodies are commonly bilateral, while choroidal osteomas tend to be unilateral).
Drusen bodies are located at the level of the optic nerve head.
Drusen bodies are found in < 1% of the population and may be familial.
When the drusen body is deep, it may elevate and blur the margins of the optic disc and clinically mimic papilledema.
Usually drusen bodies are asymptomatic and incidentally found, but occasionally, permanent or episodic visual field defects may be present.
Choroidal osteomas are located distal to the optic disc and are more common in patients with tuberous sclerosis.
Choroidal osteomas cannot be differentiated from the more common idiopathic subchoroidal calcifications.
Disorders of calcium and phosphorus metabolism may also produce ocular calcifications.
Occasionally, choroidal angiomas will calcify.
The end result of any severe infection, inflammation, or traumatic process to the eye is globe shrinking and calcification (phthisis bulbi).
Calcifications at the tendinous insertions of the extraocular muscles (unilateral or bilateral) are normal and seen in older individuals.
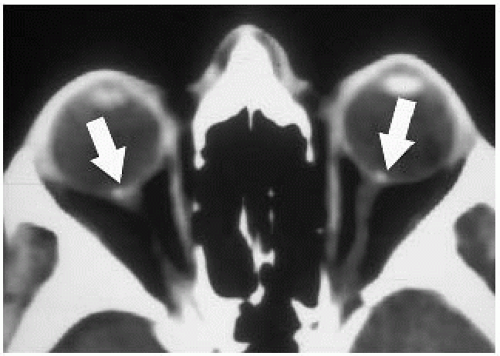
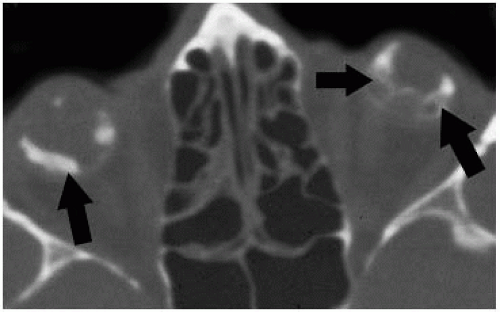 FIGURE 31-6. Axial CT, in a different patient, shows bilaterally calcified (arrows) small globes in phthisis bulbi. |
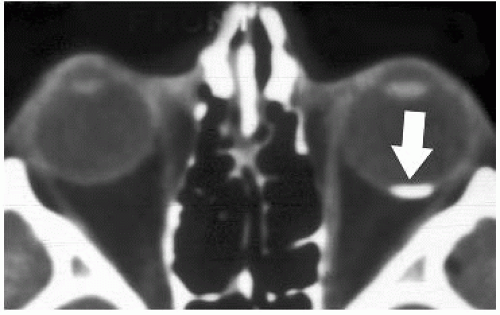
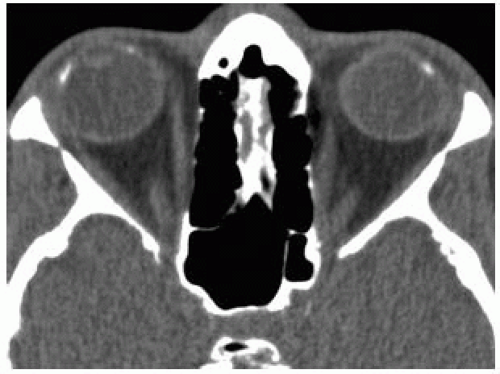 FIGURE 31-7. Axial CT, in a different patient, shows normal calcifications (arrows) at insertions of the left medial and lateral recti muscles (limbus calcifications). |
SUGGESTED READING
Davis PL, Jay WM. Optic nerve head drusen. Semin Ophthalmol 2003;18:222-242.
RETINOBLASTOMA (PNET-RB)
KEY FACTS
Most important cause of leukokoria (white pupillary reflex); other causes for leukokoria include persistent hyperplastic primary vitreous, retinopathy of prematurity, congenital cataract, toxocariasis, and Coats disease.
Average age at diagnosis: 13 months (most are found at <5 years of age); nearly 100% of bilateral cases and 15% of unilateral ones are hereditary (chromosomal defect in 13q).
25% to 30% are bilateral; trilateral retinoblastoma (both eyes and pineal gland or suprasellar region) is very rare (<1%). Patients with 13q abnormalities have increased incidence of cerebral abnormalities.
If the tumor extends beyond the globe, mortality is near 100%; occasionally, it presents as a diffuse infiltrating mass.
Intraocular calcification is a retinoblastoma until proven otherwise. However, CT is no longer needed to make diagnosis as magnetic resonance imaging (MRI) features are typical.
MRI: T1 hyperintense, T2 hypointense, + contrast enhancement (enhancement of the anterior eye segment generally represents reactive angiogenesis and not tumor).
Overall long-term survival is >80% in localized tumors.
Main differential diagnosis: persistent hyperplastic primary vitreous, Coats disease, retinopathy of prematurity.
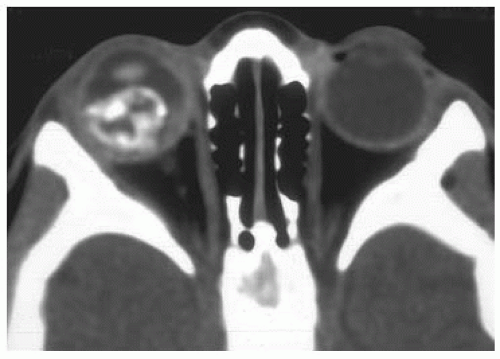
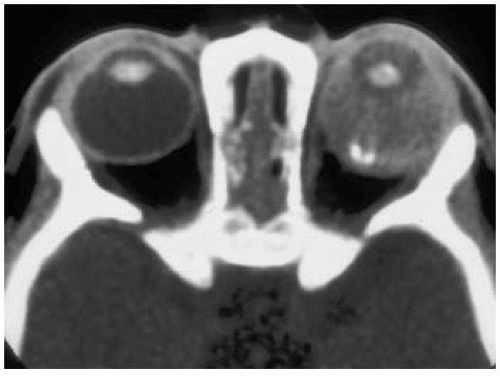 FIGURE 31-9. Axial CT, in a different patient, shows a mostly noncalcified left-sided retinoblastoma with enlargement of the globe. |
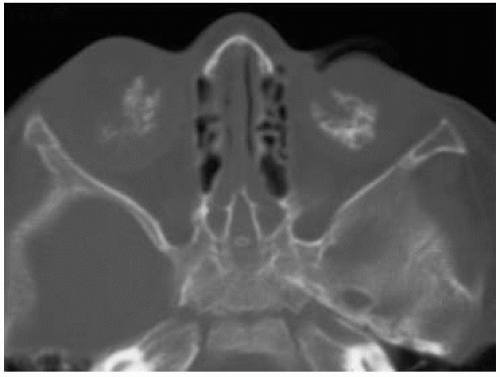 FIGURE 31-10. Axial CT, in a different patient, (bone windows) shows bilateral calcified retinoblastomas. |
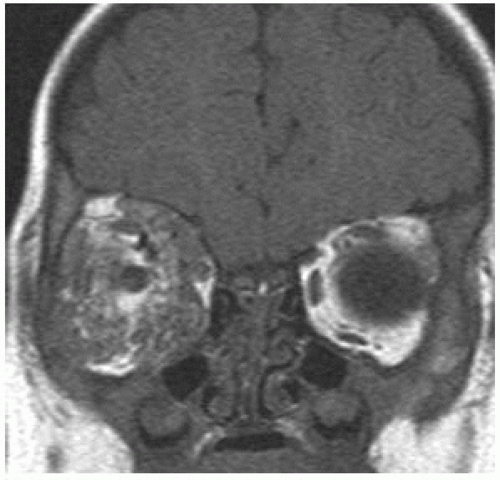
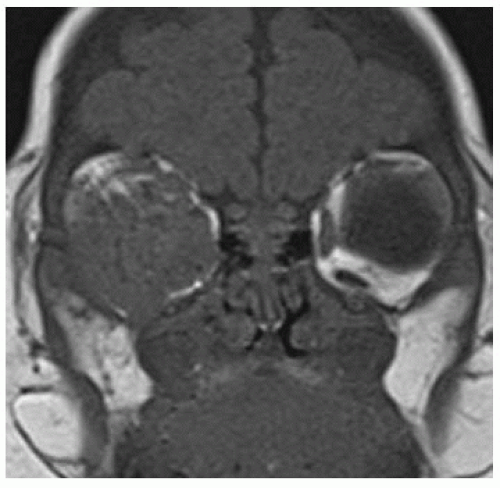
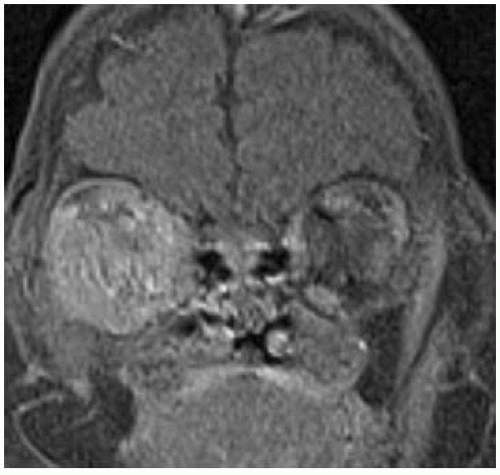
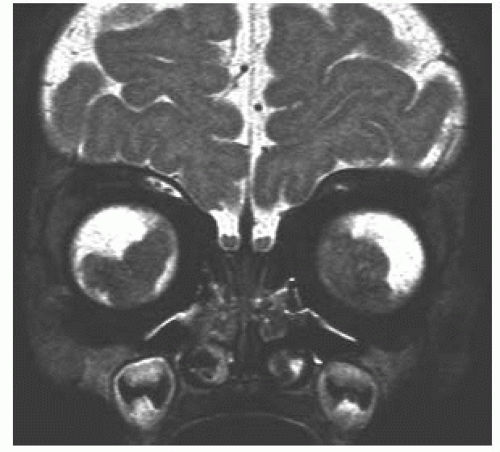 FIGURE 31-11. Coronal T2, in the same patient, shows that the tumors are of very low signal intensity. |
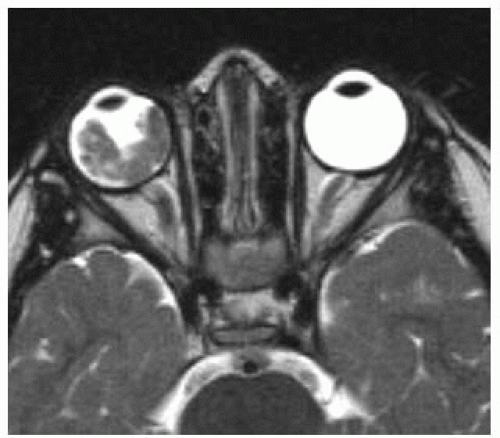 FIGURE 31-12. Axial T2, in a different patient, shows a low signal tumor in the right eye implying a hypercellular tumor. |
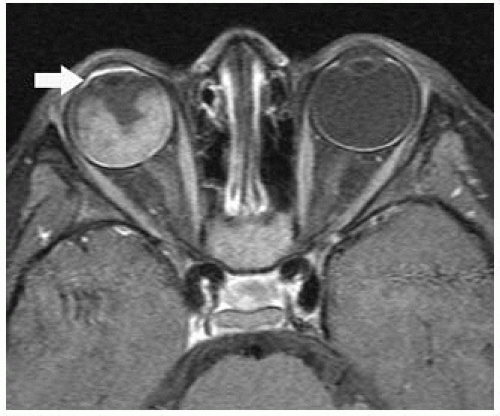 FIGURE 31-13. Corresponding postcontrast T1 shows marked tumor enhancement. Note enhancement of the anterior segment (arrow) due to reactive angiogenesis. |
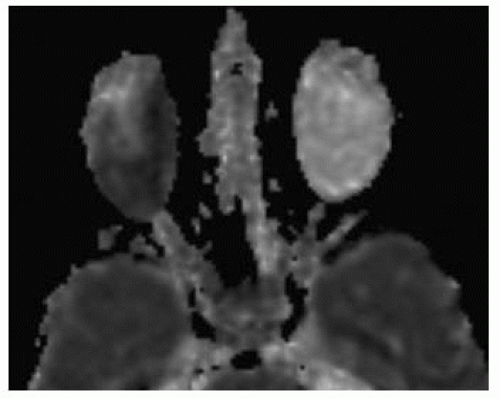 FIGURE 31-14. Corresponding apparent diffusion coefficient (ADC) map shows low signal from the tumor compatible with hypercellularity. |
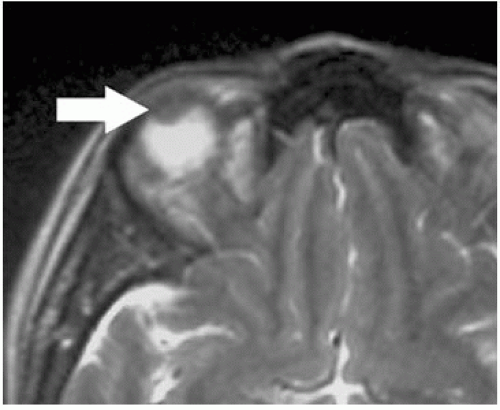
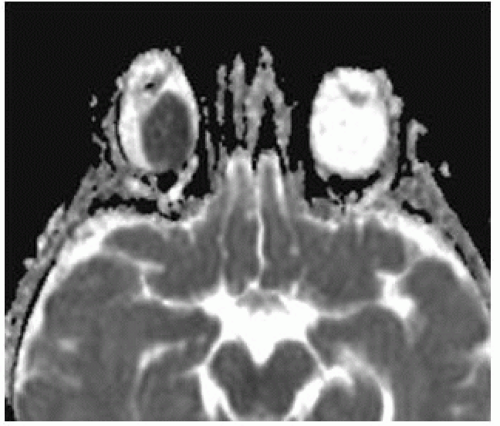 FIGURE 31-15. ADC map, in a different patient, shows a well-defined tumor in the right globe with very restricted diffusioncompatible with hypercellularity. |
SUGGESTED READING
de Graaf P, van der Valk P, Moll AC, Imhof SM, Schouten-van Meeteren AYN, Knol DL, Castelijns JA. Contrast-enhancement of the anterior eye segment in patients with retinoblastoma: correlation between clinical, MR imaging, and histopathologic findings. Am J Neuroradiol 2010;31:237-245.
Galluzzi P, Hadjistilianou T, Cerase A, De Francesco S, Toti P, Venturi C. Is CT still useful in the study protocol of retinoblastoma? Am J Neuroradiol 2009;30:1760-1765.
ORBITAL CAVERNOUS HEMANGIOMA (ADULT TYPE)
KEY FACTS
Cavernous hemangiomas are the most common retro-ocular intraconal tumor in adults (found mainly during the second to fourth decades of life); they have a fibrous pseudocapsule, receive very little blood supply, and may rarely calcify; they can be resected relatively easily.
Many patients have only proptosis without visual defects despite a relatively large mass.
CT: hyperdense well-defined mass before contrast; calcifications may be present, + contrast enhancement.
MRI: T1 isointense to muscles, T2 hyperintense with hypointense capsule; patchy contrast enhancement. On dynamic contrast-enhanced magnetic resonance (MR), they may show filling in with contrast.
Differential diagnosis includes meningioma, schwannoma, and lymphangioma (which are composed of blood vessels and lymphatic channels, occur in young individuals and adults, and tend to bleed spontaneously).
Main differential diagnosis: meningioma, schwannoma/neurofibroma, metastases, venous varix, venolymphatic malformation.
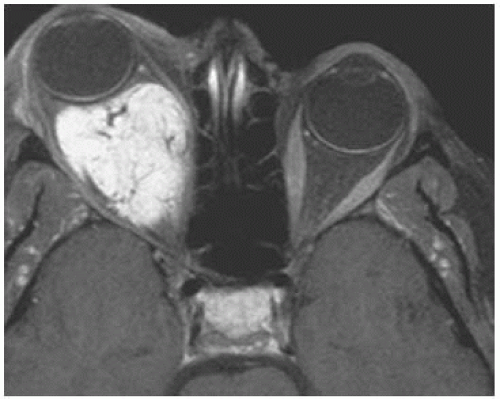 FIGURE 31-16. Axial postcontrast fat-suppressed T1 shows a large right lobulated intraconal deeply enhancing mass. |
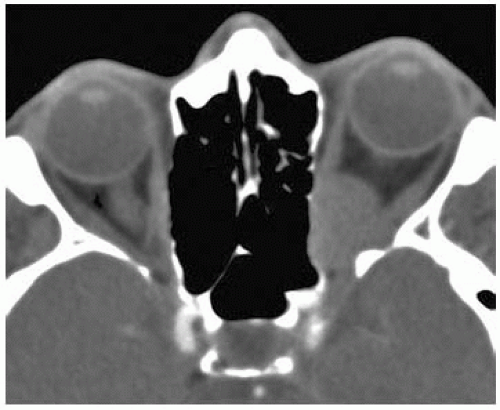 FIGURE 31-17 Axial noncontrast CT, in a different patient, shows a well-defined mass in the left orbital apex with expansion of the superior orbital fissure. |
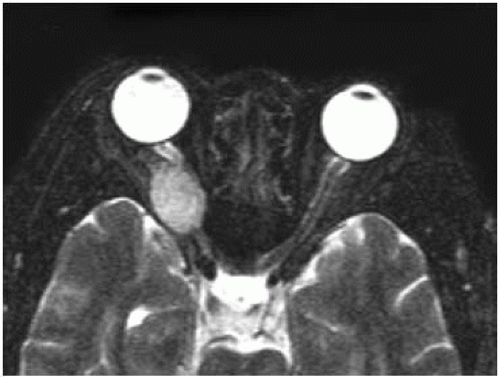 FIGURE 31-18. Axial T2, in a different patient, shows a small right intraconal mass of high signal with dark capsule. |
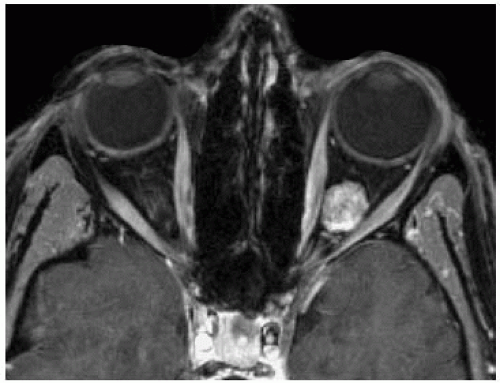 FIGURE 31-19. Axial fat-suppressed T1, in a different patient, shows a hemangioma to enhance homogeneously. |
SUGGESTED READING
Smoker WRK, Gentry LR, Yee NK, Reede DL, Nerad JA. Vascular lesions of the orbit: more than meets the eye.
RadioGraphics 2008;28:185-204. Tanaka A, Mihara F, Yoshiura T, Togao O, Kuwabara Y, Natori Y, Sasaki T, Honda H. Differentiation of cavernous hemangioma from schwannoma of the orbit: a dynamic MRI study. Am J Roentgenol 2004;183:1799-1804.
ORBITAL CAPILLARY HEMANGIOMAS
KEY FACTS
Capillary hemangiomas (infantile type) are of tumors of two classes: RICH (rapidly involuting capillary hemangioma) and NICH (noninvoluting capillary hemangioma); it may be difficult to tell them apart by imaging, but RICH contains larger blood vessels.
RICH type presents at earlier ages and starts involuting at about 1 year of age with near-complete resolution by 5 years of age.
NICH type presents later but does not involute.
Both may decrease in size after administration of propanolol or steroids, irradiation, and embolization.
Only very large ones result in Kasabach-Merritt syndrome.
Main differential diagnosis: venolymphatic malformation, cellulitis, lymphoma/leukemia.
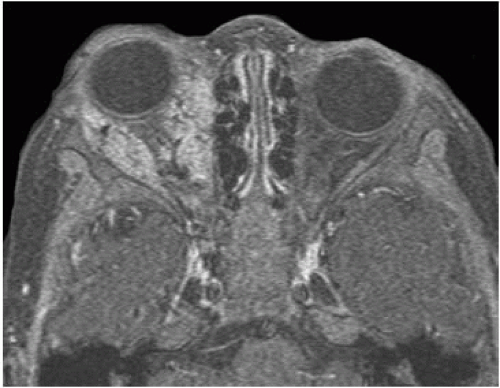 FIGURE 31-21. Axial postcontrast fat-suppressed T1, in the same patient, shows diffuse enhancement throughout the tumor. |
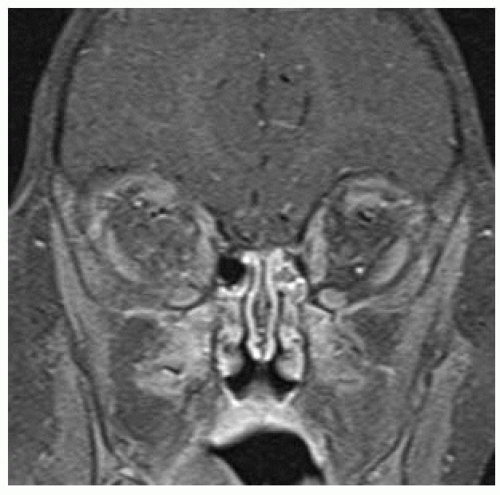 FIGURE 31-24. Corresponding fat-suppressed postcontrast T1 after 6 months of propanolol treatment shows near-complete resolution of the tumor. |
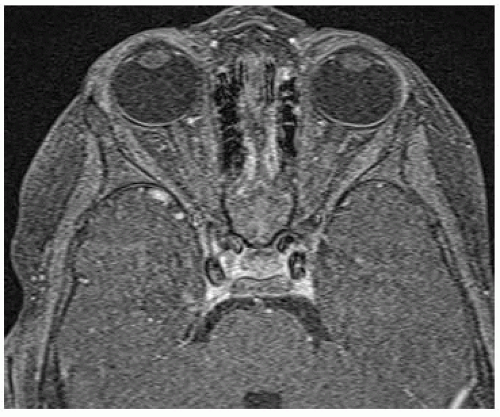 FIGURE 31-25. Axial fat-suppressed post-contrast T1, in the same patient, shows very little enhancing abnormality in the right orbit at 6 months of propanolol treatment. |
SUGGESTED READING
Rosca TI, Pop MI, Curca M, Vladescu TG, Tihoan CS, Serban ATT, et al. Vascular tumors in the orbit-capillary and cavernous hemangiomas. Ann Diagn Pathol 2006;10:13-19.
ORBITAL LYMPHANGIOMA
KEY FACTS
Lymphangoimas are benign “hamartomatous” malformations comprised of veins and lymphatics.
May involve any compartment of the orbit or several compartments simultaneously.
Progressive relentless growth is typical; sudden growth may be due to acute hemorrhage; generally found in first decade of life.
CT: multiloculated mass showing cystic areas with fluid levels (due to spontaneous hemorrhage), calcifications, and enhancement of walls.
MRI: fluid levels may have variable signal intensity on T1 and T2, depending on age of bleeds.
Main differential diagnosis: capillary hemangioma, dermoid, cystic schwannoma, plexiform neurofibromas.
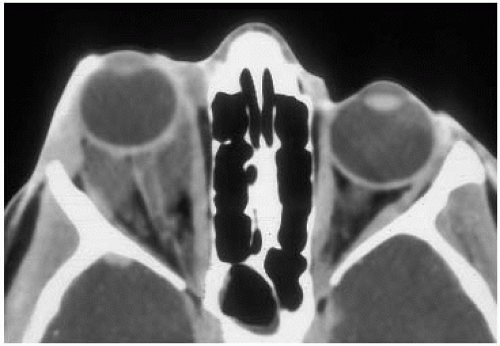 FIGURE 31-26. Axial contrast-enhanced CT shows a lobulated right intraconal mass of low density and cystic appearance. |
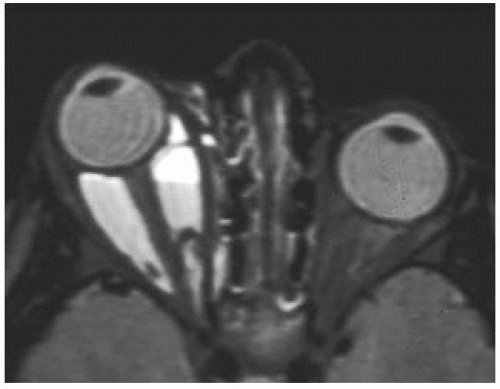 FIGURE 31-27. Corresponding T2, in a different patient, shows fluid levels and high signal intensity from this mostly cystic retroconal lymphangioma. |
SUGGESTED READING
Wright JE, Sullivan TJ, Garner A, Wulc AE, Moseley IF. Orbital venous anomalies. Ophthalmology 1997;104:905-913.
MELANOMA
KEY FACTS
Melanomas arise from the choroid, occur almost exclusively in whites, and are the most primary common ocular tumor in adults.
Most are diagnosed clinically and by sonography.
By funduscopic exam, they may be difficult to visualize if associated with choroid or retinal detachments (especially hemorrhagic ones).
They are most commonly located in the choroid (85%), ciliary body, and iris.
CT: hyperdense mass that shows moderate contrast enhancement.
MRI: T1 bright, T2 dark, + enhancement; effusions are also well visualized and are slightly T1 and T2 bright due to protein and blood.
Mortality reaches 70% when tumor size exceeds 12 mm.
Main differential diagnosis: chorioretinitis, choroidal hemangioma, metastasis, detachment, cysticercosis.
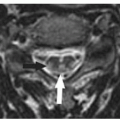
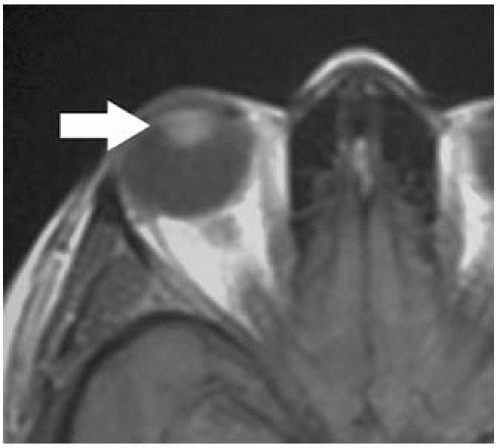 FIGURE 31-28. Axial noncontrast T1 shows a bright mass (arrow) in the superior aspect of the right globe. |
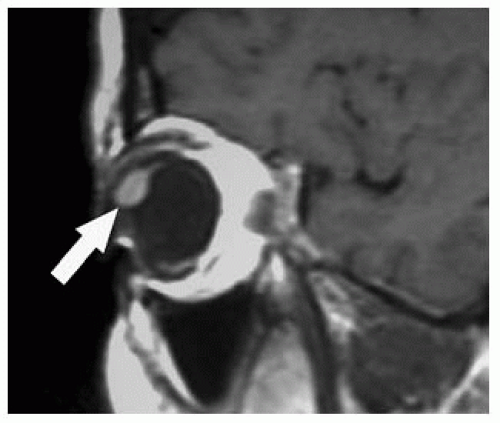 FIGURE 31-30. Sagittal postcontrast T1, in the same patient, shows enhancement of the mass (arrow) that is now of higher signal than before contrast. |
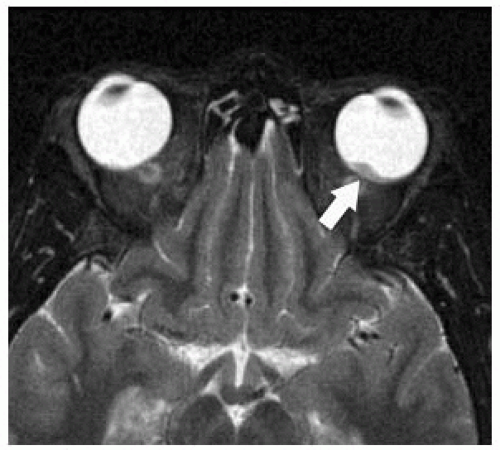 FIGURE 31-31. Axial T2, in a different patient, shows a dark melanoma (arrow) in the left eye.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|