Outpatient Drainage—Catheter Care
Susan Benveniste
Maye M. Chan
DéAnn O. McNamara
Initial Biliary Catheter Placement
When endoscopic biliary drainage is not possible, decompression or diversion of the biliary tract is achieved by accessing the biliary system percutaneously to drain bile (1). Ideally, side holes of the biliary drain are positioned proximal and distal to the lesion so bile can drain internally utilizing an internal-external drainage catheter. In cases where an obstruction or injury cannot be crossed, the tube is positioned proximal (upstream) to the obstruction which allows for decompression utilizing an external drain.
1. Postprocedure management
a. Patients are typically admitted for observation following placement of a biliary catheter.
b. Pain is typical postprocedure. When severe, it may lead to hypoventilation. Although most patients respond to oral pain medication, some may require intravenous (IV) pain management or a nerve block if the drain is placed intercostal.
c. Although bleeding is usually self-limited, intra- and extrahepatic bleeding is possible due to the vascularity of the liver. Bile drainage should be monitored. Following drain placement, blood stained bile is expected and should clear within 24 to 48 hours. When drainage appears to be bright red blood, a hematocrit is obtained. Careful monitoring of the patient’s hemodynamic status is essential, especially in the first 24-hour period. It is unusual for bleeding to require transfusion, but persistent bleeding may indicate an arterial or portal vein injury. Resuscitation of the patient and arteriography may be required.
d. While the patient is administered appropriate prophylactic antibiotic within 60 minutes of procedure start time, fever or rigors can occur immediately postprocedure as a result of transient bacteremia. The patient should be treated symptomatically and monitored for progression to cholangitis and sepsis, all of which would require immediate treatment with a plan for increased level of care. Rapid resolution of bacteremia through appropriate antibiotics and supportive care for cholangitis permits transition to oral antibiotic administration and decreased hospital stay.
e. Bile peritonitis can occur if even a small amount of bile leaks around the tube into the peritoneal space during tube placement. This can result in severe, acute pain which typically requires IV narcotics. It may last several days.
2. Instructions for biliary tube care
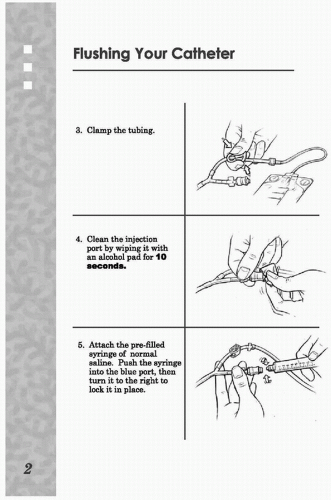
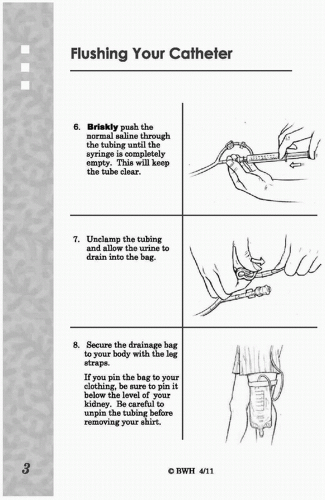
a. External drainage catheters and their attached bag should be considered a closed system and precautions should be taken to prevent bacteria from being introduced retrograde. Unless instructed to cap the tube, by the health care provider, the tubing should not be disconnected from the drainage bag. Always clean hands with soap and water, or an alcohol-based sanitizer before and after tube care. Depending on the physician’s preference and the patient’s clinical status, the tube may be flushed with 10 mL of normal saline to keep the tube patent by removing biliary debris which can build up in the lumen and cause an obstruction. When flushing is planned, a coupling device with a port access, such as a three-way stopcock or Y-connector, is left between the catheter and the drainage bag (Fig. e-103.1).
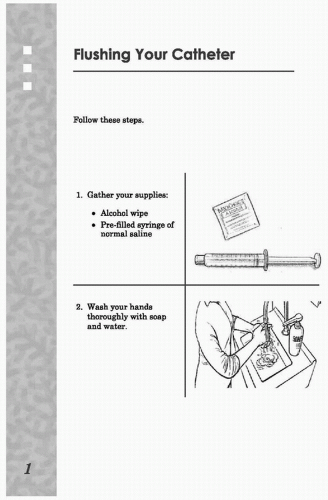 FIGURE e-103.1 • Flushing your catheter. (From Your Nephrostomy Catheter. Patient Education. Brigham and Women’s Hospital; 2011, with permission.) (continued) |
b. Prior to flushing, clean the access port with alcohol. When flushing biliary tubes, do not aspirate. Aspiration introduces bacteria from the intestine, colonizing the bile. Signs of biliary drain obstruction or displacement include resistance, pain, or pericatheter leaking when flushing.
c. The dressing should be changed routinely to keep the skin clean and dry. Dressing changes should use clean technique to prevent introduction of bacteria into the biliary system. When changing the dressing, inspect the tube insertion site as well as the surrounding skin for signs of infection or local irritation. The skin can be washed with a clean gauze and water. The skin should be dry before reapplying clean dressing to cover the site.
d. The tube may be secured at the insertion site with a suture, or it may be stabilized with various drain securing devices. The patient needs to be aware of how the anchor works in order to recognize displacement of the catheter.
e. Biliary tube insertion site and dressing must remain dry and clean to reduce the likelihood of infection.
(1) They should never be submerged in standing water. For this reason, tub baths and swimming are to be avoided.
(2) For the first 48 hours, the patient is instructed to refrain from showering and to maintain integrity of the dressing. Afterward, patients may be instructed to cover the site and dressing with plastic wrap prior to showering. It must be noted that, currently, there is a lack of literature to suggest a difference between the practices of allowing the patient to shower with the tube site exposed versus covered.
3. Follow-up care
a. If attempts to cross the lesion are not successful, the biliary catheter will be placed to external drainage. It may be beneficial for the patient to return in 2 to 7 days for a repeat attempt to cross the lesion. In some situations, depending on the patient’s diagnosis, the biliary tube may need to be left permanently to external drainage. Long-term external drainage may lead to electrolyte disturbances; oral or IV replacement of fluid and electrolytes is required.
b. After initial placement of a biliary catheter across an obstruction, the internal-external drainage catheter is typically attached to a bag to permit external drainage for 24 hours prior. This is thought to help prevent cholangitis. After optimal decompression of the biliary system, the tube can be capped to allow internal biliary drainage.
c. The biliary tube should be checked and changed every 2 to 3 months. Patients should be seen sooner if they develop problems. Changing the tube is usually an outpatient procedure. The procedure is typically not as painful as the initial tube placement, and patients can often be discharged the same day with the tube capped.
d. Prophylactic IV antibiotics are usually administered prior to the tube change, but there remains a risk of developing bacteremia and/or biliary sepsis postprocedure. If this occurs, the patient’s tube should be opened to external drainage and the situation assessed for the severity of symptoms. A fever less than 101°F may typically be treated with antipyretic medication and observed. Fever greater than 101°F suggests cholangitis and requires appropriate antibiotic therapy and supportive care which may include hospitalization (2).
Initial Nephrostomy Tube Placement
Percutaneous nephrostomy tubes may be indicated to provide access for endourologic procedures or for treatment of an obstruction or injury of the renal collecting system (3). Urine may be drained externally to decompress an obstructed system or divert urine away from a ureteral injury or fistula. If the obstruction or injury can




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree