Patient Care Before, During, and After Radiotherapy
Key Points
Dental assessment, supportive care, and rehabilitation are integral in the care of patients with head and neck neoplasms.
Tooth restoration or, when indicated, extraction before commencement of radiotherapy is effective in preventing complications resulting from dental decay and infection.
Stringent oral hygiene and systematic use of fluoride gel are essential to prevent dental hypersensitivity, caries, and osteoradionecrosis of the mandible following radiotherapy.
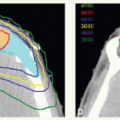
Xerostomia is a common bothersome side effect of comprehensive head and neck irradiation but, fortunately, its incidence and severity have decreased with the use of parotid-sparing intensity-modulated radiation therapy.
Nutritional support and management of pain, nausea, and mucoid secretions are crucial for minimizing distress and facilitating completion of radiotherapy without interruption and recovery after treatment.
Timely assessment and prescription of mouth-opening and swallowing exercises prescribed and supervised by speech pathologists facilitate preservation of functions and quality of life.
Many unpleasant treatment-induced sequelae can be prevented or lessened by timely and proper interventions.
DENTAL CARE
Evaluation, treatment, and prevention of any preexisting oral or dental pathology are an integral part of management of patients with head and neck cancer because complications vary with dental condition, the type of malignancy, and the therapeutic approach. Underlying preexisting silent pathology can become prominent in a patient receiving radiation, and particularly so in combined therapy. Mild problems of the oral cavity can develop into severe complications that can either compromise cancer therapy or cause considerable morbidity. Oral complications can be minimized and, in some cases, eliminated, if identified and addressed early by a dental team. It is, therefore, important to assess the patients’ access to dental care and their commitment to daily oral hygiene procedures.
A comprehensive evaluation of patients presenting with head and neck tumors includes an oral and dental clinical examination supplemented by intraoral radiologic evaluation. Selected dental radiographs are essential in evaluating potential areas of infection that are not obvious on clinical examination (e.g., periodontal-periapical tooth pathology, residual cysts, and impacted or partially erupted exfoliating teeth). From this information, the dentist can plan oral treatment to bring the dental problem under control, thereby meeting immediate needs before radiation therapy. Oral treatment plans should be designed to correct restoration overhangs, rough or sharp edges in teeth, and any other defects that can cause soft tissue irritation. Patients should be instructed to avoid abrasive food that could traumatize soft tissues. Ill-fitting intraoral prostheses should not be worn during radiation therapy. Dental implants should be
carefully assessed, and their removal should be considered if maintenance of peri-implant health cannot be reasonably anticipated or if integration is poor. Any potential source of oral infection should be identified and eliminated.
carefully assessed, and their removal should be considered if maintenance of peri-implant health cannot be reasonably anticipated or if integration is poor. Any potential source of oral infection should be identified and eliminated.
In general, patients with good dental status, including those who need routine restoration of a few cavities, are instructed to maintain oral hygiene and undergo brush training. They also receive custom-made carriers for fluoride prophylaxis to prevent caries and hypersensitivity of teeth and mouth guards, made of flexible plastic material, to prevent biting irradiated tissues that may become edematous. Edentulous patients are instructed to maintain oral hygiene, and to avoid trauma and premature use of prosthesis. In patients undergoing surgical therapy, the oral cavity should also be prepared for appropriate prosthetic rehabilitation to correct surgical deficits.
When there are findings of periapical pathosis, questionable periodontal status, unrestorable teeth with advanced caries, supererupted teeth, and, possibly, unopposed dentition, the teeth involved should be considered for extraction. Endodontic therapy is a viable alternative for pulpal necrosis, provided that the treatment can be expeditiously performed before the initiation of cancer therapy.
To ensure bone coverage and adequate wound healing, extractions should be performed 2 to 3 weeks before initiation of cancer therapy. Extractions and associated alveoloplasty should be performed with minimal trauma and should include smoothing of sharp surrounding hard tissue, appropriate irrigation, and primary closure in order to promote rapid healing. In general, periodontal surgical procedures should be avoided because prolonged healing and meticulous oral hygiene are needed to achieve the desired results.
The decrease in saliva production that often results from radiation to the head and neck region reduces the natural lavage of food and microbial debris from the oral cavity, which can lead to the development of dental caries. The change in the composition of saliva and reduced pH and buffering capacity also create a cariogenic oral environment, particularly in patients ingesting a diet high in carbohydrates or sucrose. Increased gingival recession may occur without signs or symptoms of periodontal inflammation. Therefore, special oral care is needed to prevent complications.
Good oral hygiene during and after therapy is essential for improving oral comfort and for reducing the risk of oral pathology. Bacterial and fungal superinfection can occur, but are less likely to induce septicemia in patients undergoing radiotherapy alone than in those receiving concurrent chemotherapy, which causes bone marrow suppression. Oral rinsing with a solution of 1 teaspoon of sodium bicarbonate dissolved in 32 oz of water many times each day reduces oral microorganisms and aids in maintaining mucosal hydration. This measure, along with the elimination of secondary sources of irritation, such as alcohol, smoking, coarse or hot foods, alcohol- or phenol-containing mouth rinses, and sodium products, can help in minimizing mucositis.
The daily use of a fluoride gel can help minimize dental decay. The common formulations used are either 1.0% sodium fluoride gel or 0.4% stannous fluoride gel. Compared with sodium fluoride, stannous fluoride is slightly more acidic, but its uptake into the enamel matrices is four times greater. In adults with xerostomia, fluoride is released from the enamel within 24 hours; therefore, the fluoride regimen must be performed daily for optimal protection. The most efficient method of fluoride application is to use a custom-made polypropylene fluoride carrier that completely covers and extends slightly beyond the tooth surface. Patients fill the carriers with fluoride gel and place them onto the dentition daily for 10 minutes. Patients who receive low doses of radiation and are expected to have a slight degree of xerostomia can use a toothbrush to apply the fluoride gel. Sensitivity and pain are common side effects of fluoride and may necessitate a change in the fluoride concentration or the method of application. A daily fluoride program can decrease hypersensitivity, help mineralize cavitated enamel matrices, and, more important, inhibit caries-forming organisms.
Conventional oral physiotherapy is recommended during and after radiation, especially if the pterygoid muscles are within the radiation portals. Fibrosis of this musculature leads to trismus, which may be irreversible. Therefore, patients should be encouraged to perform mouth-stretching exercises before, during, and after radiation therapy. When needed, sophisticated means of mouth-opening exercises with opening devices (such as TheraBite, Jaw Dynasplint) may be recommended.
Radiation diminishes cellular elements of bone, thereby reducing its ability to heal after infection, trauma, or surgical procedure (e.g., dental extraction, alveoloplasty), which may result in osteoradionecrosis (ORN). Therefore, periodontal surgical intervention should be planned carefully, and the use of parenteral antibiotics and hyperbaric oxygen should be considered.
NUTRITIONAL SUPPORT
Assessment and Guidance
Nutritional care is crucial in the radiation treatment of patients with head and neck cancer. Patients receive dietary advice to help maintain their weight and nitrogen balance during the course of radiotherapy and the ensuing recovery period. Good nutritional support minimizes the need for therapy modifications (interruptions or dose reduction due to worsening of general condition and/or excessive reactions) that would compromise tumor cure probability.
It is essential that the nutritionist establishes a good rapport with the patient and provides basic instructions before
the onset of acute reactions. It is prudent to counsel the patient’s family members because the patient, who is under stress after learning the diagnosis and experiencing discomfort and pain, may not fully comprehend the instructions. Follow-up meetings are scheduled once a week, or more often when interim problems occur, and data of weekly interviews are recorded along with the patient’s initial and follow-up body weight. The attending physician and nutritionist should review the chart and recommend dietary adjustments when necessary.
the onset of acute reactions. It is prudent to counsel the patient’s family members because the patient, who is under stress after learning the diagnosis and experiencing discomfort and pain, may not fully comprehend the instructions. Follow-up meetings are scheduled once a week, or more often when interim problems occur, and data of weekly interviews are recorded along with the patient’s initial and follow-up body weight. The attending physician and nutritionist should review the chart and recommend dietary adjustments when necessary.
Patients receiving radiation treatment of cancers of the oral cavity, oropharynx, nasopharynx, and hypopharynx are particularly prone to develop difficulties with food intake because of irradiation of a large area of mucous membranes and salivary glands. Therefore, they are encouraged to take supplemental calories at the beginning of treatment before the onset of reactions. The first problem encountered by this group of patients relates to alteration in salivary function, resulting in mucoid thick saliva. Moistened foods and increased fluid intake frequently facilitate mastication and deglutition during the first week.
Taste distortion (metallic flavor), loss of appetite, and burning sensation in the throat when swallowing citrus juices and acidic or spicy food become prominent during the second and third weeks. Helpful measures include the use of bland fruit nectars or fruit-flavored drinks fortified with vitamin C, elimination of highly seasoned foods, addition of food aroma, and serving meals at room temperature.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree