Abstract
This chapter provides an overview of the principles and concepts of patient safety and quality improvement in radiology and includes commonly used methodologies for quality improvement and a discussion of practical examples of patient safety practices in radiology. Many topics introduced in this chapter are discussed more fully in subsequent chapters.
Keywords
Accuracy, benchmarks, error, culture of safety, dashboards, high-reliability organization, KPI, Lean Six Sigma, National Patient Safety Goals (NPSG), precision, quality improvement, quality control, quality science, six aims, value
Safety in radiology is expected by our patients, colleagues, administrators, providers, national organizations, oversight organizations, and the government. It is no longer enough to provide accurate reports of findings on imaging studies. Radiologists and their coworkers in the radiology department are also expected to provide patient-centered care and safe experiences prior to, during, and after imaging and procedures in radiology. To meet this need, considerable educational and other resources have evolved to guide radiologists and their staffs to carry out meaningful improvements in patient safety and have raised the awareness of existing tools to help assess and improve safety in radiology.
Today, radiologists are expected to be fully engaged in all aspects of radiology and to add value to the patient experience by ensuring that safety is at the forefront of care. Performing the right examination at the right time for the right reasons is now a basic assumption. Providing timely results is expected and communicating critical values in short time frames with appropriate follow-up is a widely expected outcome. Consistently delivering actionable recommendations based upon the best evidence available is on the horizon. Within the whirlwind of all these laudable goals is the patient who is likely to be ill and may be overwhelmed and confused by the medical system. As radiologists and staff working in radiology we must now, more than ever, examine our culture, processes, and experiences to do our best to ensure that the patient is kept as safe as possible, while accepting that no system is perfect and that adverse events are not completely preventable. Our goal is to consistently improve our processes and use adverse events and outcomes as opportunities for learning and making patient safety more robust. We do this realizing that it is the right thing to do and the right way to practice medicine. We accept that often there will not be additional reimbursement for better safety measures and that sometimes our leaders and those in positions of greatest power will talk about safety first but actually be less than devoted to the execution of safety measures when they conflict with financial targets. Still, we must keep our eyes on the patient and pursue our patients’ safety as a core duty and basic element of our work in radiology.
Safety and Error
A basic aspect of improving safety is understanding error. The study of human error has been important in industries like manufacturing and aviation for several decades. Medicine has more slowly embraced the study of error. Many cite 1996, with the publication of the monograph To Err Is Human, as the beginning of the serious study of safety and quality in medicine. At that time, the realization began that the current state of affairs in medical care with respect to safety was unacceptable and urgent action was necessary to insure safe treatment of patients.
Quality improvement (QI) is a goal as well as a hot topic for discussion in many healthcare organizations. QI replaces the concept of quality assurance, which was more often than not reactive, punitive, and focused on assigning blame. QI has the goal of actually making things better. It involves retrospective and prospective reviews and data collection, which should be used to create systems that prevent errors from happening, or at least minimize errors and reduce their impact. It should attempt to avoid attributing blame, but people being people, that goal is not always achievable. Ideally, QI is a continuous process, hence the term continuous quality improvement (CQI). In CQI, the challenge is to closely examine a process that is working fairly well and tweak it to make it better still. However, once a process is improved , we tend to move on with other work and it is often a poor outcome or adverse event that forces us to go back to the process and look again to find and correct latent defects. Ideally, such discovery and improvement should be prospective, ongoing, and iterative, not episodic, sporadic, and reactive.
Quality control (QC) is often useful or essential as part of a practice quality improvement (PQI) project. PQI projects are the focus of a later chapter. QC is the process by which we review the quality of all elements and factors in producing an item of outcome. QC often involves evaluation of accuracy , precision , and reliability. Accuracy refers to the closeness of a measurement to the true value. Precision refers to the reproducibility of a measurement. Reliability includes both the accuracy and precision of a measurement. Therefore, QC evaluates a process for accuracy, precision, and reliability and provides data to validate the conclusions of a QI project.
Quality Science and the Six Aims
Quality in healthcare is sometimes referred to as quality science . Perhaps it is less rigorous than physics or mathematics, but it has come a long way in the past 20 or so years. Currently, quality efforts often include measurement, data analysis, and assessment for variation. In the past, variation was accepted or ignored; now variation is viewed as a potential concern and mainly something to be avoided. Leadership that supports QI, and the efforts necessary to obtain and analyze data, is essential to strides that have been made in this field, as well as ongoing progress.
Much of the focus on quality in healthcare and radiology derives from goals and publications originating from an organization known as the Institute of Medicine (IOM). Very recently the name changed to the National Academy of Medicine (NAM), which is a nonprofit, nongovernmental organization that is part of the National Academies of Sciences, Engineering and Medicine. NAM provides advice on issues relating to biomedical science, medicine, and health. The advice should be evidence-based and may be used by policy makers as well as the public at large. The NAM has proposed the Six Aims of High-Quality Care: namely, that healthcare should be (1) safe, (2) timely, (3) effective, (4) efficient, (5) equitable, and (6) patient centered.
An integral part of the quality movement in healthcare is the Maintenance of Certification or MOC. In theory, MOC provides value by promoting lifelong learning that encourages incorporating new information and knowledge into routine clinical practice. The American Board of Radiology looks back at three previous years and determines if each diplomate is meeting MOC requirements. MOC touches on six core competencies: (1) patient care, (2) medical knowledge, (3) interpersonal and communication skills, (4) professionalism, (5) systems-based practice, and (6) practice-based learning and improvement. A central tenet is that patient care should be compassionate, appropriate, and effective and based upon established and evolving knowledge. Communication should be effective with patients, families, and professional associates. Performance of duties should be ethical and sensitive to diverse patient populations. Care givers should be able to work well as part of the team and help to improve the practice of medicine.
Quality Metrics and Dashboards
We all hope to practice quality medicine. However, quality can be an elusive goal, and choosing metrics that truly reflect the quality we seek can be challenging. Dashboards help us to assess quality and avoid unnecessary variation. A dashboard is a visual display of important information, just like in a car. As in driving, the information should be displayed so that it can be monitored at a glance. Benchmarking also helps us make some decisions regarding whether we are practicing quality medicine. It involves comparing a product, policy, program, or outcome with those of a similar organization or a peer. Hopefully we can learn from others how to achieve high performance and they can learn from us.
Quality and Value: Measurement and Graphical Tools
Just as quality can be hard to pin down conceptually, so can value . The term value brings to mind concepts like quality, cost, and efficiency. It may be useful to think of value as efficient use of resources to produce a desired result. Most analyses of value include a comparison of costs to benchmarks.
Thought leaders working in the field of value in healthcare often refer to key performance indicators (KPIs), which are measures used to define and evaluate the success of an organization. KPIs are specific to an organization’s goals and strategies. One can look at progress in KPIs over time to determine whether an organization is making progress toward its goals.
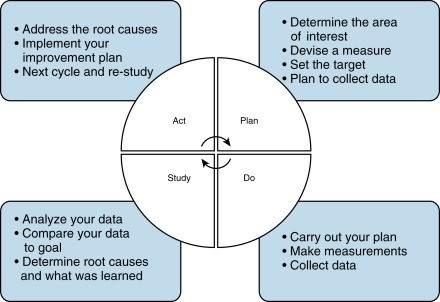
There are a variety of methods that may be useful in the performance of a CQI project. One of the best-known methods is the plan-do-study-act (PDSA) cycle ( Fig. 5.1 ). This series of steps for gaining knowledge about a process was made well known by Dr. W. Edwards Deming and Walter Shewhart at the highly respected Bell Laboratories. It is meant to be an iterative process that identifies a goal, puts a plan into action, monitors outcomes with data collection, and acts on the information acquired to change and hopefully improve the process of a plan. It is important to have an appropriate measure or measures and to set a target level of performance desired. At the end of the first cycle, one can determine how well the data compares with the desired goal and also consider root causes for failure to meet the goal. After the first cycle, an improvement plan should be created and another PDSA cycle begins until the goal is achieved.
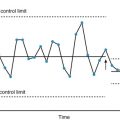
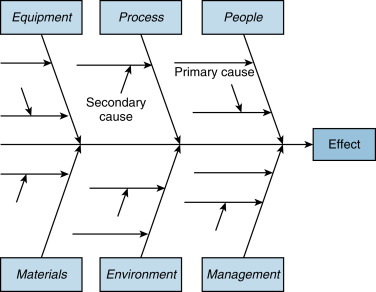
A method commonly used in QI projects involves graphical tools as a picture, which can often be more illuminating than a long discourse. An example of a graphical tool is the flow chart, where the steps in a process are presented as a diagram using commonly accepted symbols to illustrate the process and help clarify stress points as well as opportunities for improvement. A Pareto chart is another graphical tool where risk factors are displayed in order of importance. The fishbone diagram, also known as an Ishikawa diagram, is often used in root cause analysis (RCA) to help identify all causes that contribute to an identified problem in a manner that is visually inclusive and comprehensible ( Fig. 5.2 ). The control chart is another method and is used to determine if a process is stable with variation coming only from sources common to the process. Analysis of a control chart may also help determine the sources of variation. Typically, control charts are used for time series data and therefore variation at a given time of day may be discovered. For further detail on these topics, the reader is directed to the suggested reading list at the end of this chapter.
The Hawthorne Effect
In the performance of a QI project it is important to be aware of sources of bias. In particular, it is important to be aware of the Hawthorne effect , also known as the observer effect. This effect is exhibited in the fact that individuals modify or improve an aspect of their behavior simply in response to their awareness of being observed. As an example, in a study looking at radiation dose measurement during fluoroscopy, there was an initial decrease in fluoroscopic times when radiologists were monitored, which could be attributed to the Hawthorne effect. Interestingly, there is not universal acceptance of this effect by experts in the field, and some feel that it attenuates over time.
Lean/Six Sigma
Yet another methodology used in the QI sphere is Lean Six Sigma . This methodology relies on a collaborative team effort to improve performance by systematically analyzing processes step by step, removing waste from each step, and finding ways to eliminate defects. The interest in this method was inspired by the success of the Toyota Motor Company. It was also central to the strategy of General Electric and Motorola. A core principle of Lean Six Sigma is respect for the relationships among employees, suppliers, and customers based upon mutual trust and dedication to improvement. This speaks to a healthy organizational culture, and although the sentiments are admirable, even Toyota seems to have had difficulty bringing this concept to fruition as it deals with large settlements for concealing safety issues with unintended acceleration and defective air bags. A focus on data collection, elimination of waste, and reduction in unnecessary variation suggests why Lean has become popular in healthcare. However, it is also important to accept that not all companies practicing Lean Six Sigma (including Toyota) have had sustained success. Some business leaders caution that “the process triumphs over judgment” (John Boyle, founder of the Vanguard Group).
In addition to the methods described previously, another technique used since the 1950s is brainstorming. It began in the advertising industry as a method for creative problem solving. It relies on a group process where a list of ideas is spontaneously contributed by the members of the group. Brainstorming seeks quantity of ideas, welcomes out-of-the-box thinking, and prohibits initial criticism. After ideas are accumulated, the group may vote on the value of the ideas, and retained ideas are eventually used as the basis of action plans. Brainstorming, along with all of the methods discussed, has its place and value. However, it is important to realize that the value of any of these techniques is open to skepticism, and, in fact, there is little objective evidence to support the inherent value of any given QI method. Still, experience suggests that each tool may have positive applications when combined with insight and wisdom.
The Joint Commission
The Joint Commission (TJC) is an independent, not-for-profit organization that accredits and certifies healthcare organizations. Thus organizations seriously consider the goals of TJC and usually embrace its goals as part of the organization’s safety priorities. Examples of some of the goals are prevention of falls, patient identification, reducing hospital infections, improving hospital staff communication, and avoiding abbreviations that lead to misinterpretation. These are part of the National Patient Safety Goals (NPSGs). Other goals that often impact radiology departments include reporting of critical results of tests in a timely manner, labeling all medications, maintaining accurate patient medication records, complying with hand hygiene guidelines, preventing central line–associated infections, conducting a preprocedure verification process, marking the proposed procedure site, and performing a time-out before the procedure. Adherence to these priorities and goals is important every day and not just when TJC inspection for accreditation is imminent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree