Abstract
Patient-specific vascular models enhance preoperative planning in interventional radiology, particularly in complex and anatomically challenging cases. This report presents two cases of complex aneurysm coil embolization in which three-dimensional, printed, patient-specific vascular hollow models were key to selecting optimal catheters, leading to successful interventions. Preoperative simulations with these models facilitated preselection of the optimal catheter, minimizing the need for intraoperative catheter exchange and reducing the time required for catheter engagement and placement. This approach improves procedural efficiency and outcomes by ensuring a smoother workflow.
Introduction
Coil embolization of peripheral aneurysms in the trunk region has been widely practiced [ ]. Achieving successful outcome requires sufficient catheter stability and the precise placement of an appropriate catheter in the primary branch of the aorta. However, preoperative computed tomography (CT) imaging often fails to provide adequate information to determine whether the chosen catheter shape will be compatible with the primary branch originating from the aorta, such as the celiac artery, superior mesenteric artery (SMA), inferior mesenteric artery, or bronchial artery [ ]. Consequently, multiple catheter exchanges during the procedure may become necessary, leading to prolonged procedure times and increased risk of vascular intimal injury, particularly when using large-diameter guiding catheters [ ].
Preoperative simulation using patient-specific vascular models offer a potential solution by reducing the need for catheter replacement, shortening the time required for catheter engagement and placement, and minimizing intimal damage risk. In Interventional Radiology, several reports have discussed preoperative simulations of aneurysm embolization using individualized vascular models [ ]. However, most existing models either lack hollow structures and only replicate anatomical shapes [ ] or are small-scale hollow models that replicate only aneurysms and adjacent inflow and outflow vessels [ ]. These models fail to reproduce the extended access route from the femoral, radial, or brachial arteries. Furthermore, hollow models often lack flexibility [ , ] and differ in physical properties, such as hardness and slipperiness from biological arteries. Consequently, these models are insufficient for simulating catheter insertion into the primary branches of the aorta.
To address these limitations, we developed a transparent, flexible, and highly slippery vascular model that accurately reproduced a wide range of vascular structures [ ]. Its utility has been demonstrated in procedures involving renal arteriovenous malformations [ ]. Preoperative simulations using this model have been reported to improve the embolization material selection and device access, including identifying the most suitable catheter and guidewire [ ]. Therefore, we planned to use preoperative simulation using this model to treat peripheral aneurysms and aimed to confirm the optimal catheter shape preoperatively.
Herein, we report 2 anatomically complex cases of peripheral aneurysms. In both cases, preoperative simulations using the developed model were performed to select the optimal catheter shape for successful treatment.
Case presentation
Preoperative simulation using patient-specific hollow vascular models
Our institutional review board approved the use of vascular models for this retrospective case report. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. Consent for publication was obtained for every person’s data included in the study. Digital Imaging and Communications in Medicine (DICOM) data from three-dimensional (3D) computed tomographic angiography (CTA) images, with a slice thickness of 0.5 mm, were converted to stereolithography (STL) files. The hollow feature of the model was created using MeshMixer (Autodesk, San Rafael, CA) with a wall thickness of 1.0 mm. The data were processed using PreForm software (Formlabs, Somerville, MA), and the model was printed using a Form 3L 3D printer with flexible, transparent materials (Flexible 80A; Formlabs). The models were subsequently rinsed with isopropyl alcohol, dried, and cured [ , ].The vascular models were coated with silicone and connected to a sheath in a white box to simulate endovascular procedures without fluoroscopy [ ].
Case 1
A female patient in her 40s presented with a 5 × 5 mm saccular aneurysm ( Fig. 1A – C ) at the origin of the dorsal pancreatic artery, branching from the SMA. She was referred to our department for prevention of aneurysm rupture. The proximity of the aneurysm to the SMA trunk made it challenging to perform coil embolization without risking coil deviation into the SMA trunk, particularly during the coil-finishing phase. Given these anatomical complexities, we created a patient-specific vascular model ( Fig. 1D ) to simulate the procedure and test the various catheter options.

Through the simulation, it was determined that using a 4.5-Fr guiding sheath (Parent Plus45 shepherd hook [SH] type, Medikit) and a 4-Fr Rösch hepatic (RH) catheter would provide sufficient backup support to ensure accurate coil placement ( Fig. 2 ).

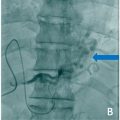
During the actual procedure in the patient, the same catheters (Parent Plus45 SH type and 4-Fr RH catheter) were used via the right femoral approach. Coil embolization for distal embolization and packing was performed with 2.4/2.6-Fr Leonis Mova (125 cm, Sumitomo Bakelite, Tokyo, Japan) inserted into the distal artery to the dorsal pancreatic artery aneurysm using detachable coils (Target XL Detachable Coils, Stryker Corporation, Kalamazoo, Michigan, USA; 3 mm × 9 cm × 1, 4 mm × 12 cm × 1, 5 mm × 20 cm × 1). Embolization was successfully completed with no complications ( Fig. 3 ).