Abstract
Percutaneous transhepatic embolization (PTE) is a minimally invasive and effective intervention for managing refractory variceal bleeding in patients with portal vein thrombosis (PVT) secondary to hepatocellular carcinoma (HCC). This case report highlights the successful application of PTE in a 69-year-old nonalcoholic male with chronic liver disease and HCC. The patient, previously treated with transarterial chemoembolization (TACE) for segment VIII HCC, presented recurrent hematemesis and significant anemia despite prior endoscopic esophageal variceal band ligation. Diagnostic imaging revealed portal vein thrombosis and extensive gastro-esophageal varices. Given the patient’s unresponsiveness to conventional endoscopic treatments, an emergency PTE was performed. Using a percutaneous transhepatic approach, the left portal vein was accessed under real-time ultrasound guidance. Subsequent venography confirmed extensive varices draining into the splenic artery. Embolization involved deploying a combination of pushable coils and a 20% glue solution, which achieved complete obliteration of the varices, as confirmed by nonprocedure imaging. The track from the liver surface to the left portal vein was sealed using a glue-lipiodol mixture to prevent complications. The patient demonstrated significant clinical improvement postprocedure, with no further episodes of hematemesis. Hemoglobin levels stabilized following transfusion of packed red cells, and the patient was discharged in stable condition. This case underscores the role of PTE as a safe and effective salvage therapy for refractory variceal bleeding in complex cases involving PVT secondary to HCC.
Background
Variceal bleeding is a life-threatening complication of portal hypertension, often associated with advanced liver diseases such as cirrhosis and hepatocellular carcinoma (HCC). Gastro-esophageal varices develop due to increased portal venous pressure, typically resulting from obstruction or reduced flow in the portal venous system. This condition is further exacerbated in patients with portal vein thrombosis (PVT), a frequent finding in individuals with HCC. The presence of PVT not only increases the severity of portal hypertension but also complicates treatment options, making the management of variceal bleeding particularly challenging [ , ]. Current guidelines recommend endoscopic interventions, such as esophageal variceal band ligation, as the first-line therapy for acute variceal bleeding. These procedures are effective in achieving initial hemostasis but may fail in up to 20% of cases, especially in patients with severe portal hypertension or underlying complications like PVT [ , ]. Pharmacological therapies, including vasoactive agents like somatostatin or terlipressin, are often used alongside endoscopic treatments but are insufficient for long-term management in many cases [ ].
In situations where endoscopic and pharmacologic treatments fail, transjugular intrahepatic portosystemic shunt (TIPS) placement is typically considered. However, TIPS may be contraindicated in patients with advanced HCC or extensive PVT, necessitating alternative interventions [ ]. Percutaneous transhepatic embolization (PTE) has emerged as a critical salvage therapy for refractory variceal bleeding in such cases. This minimally invasive technique involves accessing the portal venous system percutaneously and embolising the afferent vessels feeding the varices. PTE is particularly advantageous in patients with complex anatomy or contraindications to TIPS, offering effective hemostasis with a favorable safety profile [ , ]. The efficacy of PTE in achieving hemostasis and reducing variceal recurrence has been demonstrated in multiple studies. Li et al. [ ] conducted a meta-analysis of PTE and reported a high technical success rate, with most patients achieving immediate bleeding control and significant reductions in portal pressure postprocedure. Another study by Chawla et al. [ ] highlighted the role of PTE in managing refractory varices, emphasizing its utility as a bridge therapy in patients awaiting definitive treatment or as a standalone intervention in high-risk cases.
This case report details the successful application of PTE in a patient with HCC, PVT, and recurrent variceal bleeding who was unresponsive to conventional therapies. By illustrating the procedural approach and outcomes, this report underscores the potential of PTE to provide effective, minimally invasive management in complex clinical scenarios.
Case presentation
A 69-year-old nonalcoholic male presented with multiple episodes of vomiting characterized as sudden in onset, nonprojectile, nonbilious, and containing food particles along with traces of blood. The patient reported associated symptoms of weight loss, loss of appetite, and a persistent cough. However, there was no accompanying history of fever, loose stools, or any prior surgical interventions. He had no known medical history of hypertension, diabetes mellitus, tuberculosis, bronchial asthma, or thyroid disorders.
The patient was a known case of chronic liver disease complicated by hepatocellular carcinoma (HCC) located in segment VIII of the liver. Previously, the patient had undergone transarterial chemoembolization (TACE) as a part of his treatment. Approximately 3 months following the TACE procedure, the patient presented again with hematemesis, which was subsequently found to be associated with portal vein thrombosis. At this stage, he underwent endoscopic esophageal variceal band ligation and was discharged after stabilization.
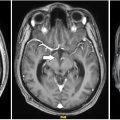
One month later, the patient was admitted to the emergency department with a recurrence of hematemesis and a significant drop in hemoglobin levels to 5.5 gm%. A contrast-enhanced computed tomography (CECT) scan revealed post-TACE changes in segment VIII of the liver with no evidence of arterial enhancement in the arterial phase. The scan also identified extensive portal vein thrombosis along with multiple intramural and extramural gastro-esophageal varices receiving afferent blood supply from the splenic artery. These findings were confirmed through imaging ( Figs. 1 and 2 ).



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree