Abstract
Arteriovenous malformations in the abdominal region are rare, and they are known to occasionally cause portal hypertension. A 66-year-old man with a chief complaint of fatigue and blood tests showing hepatic dysfunction was seen for a more detailed examination. Abdominal contrast-enhanced computed tomography showed an anastomosis of the ileal artery and ileal vein via a nidus within the mesentery. In addition to alcoholic cirrhosis from a history of high alcohol intake, the patient was diagnosed with portal hypertension from increased portal pressure due to an arteriovenous malformation in the mesentery. Vascular embolization with a percutaneous transhepatic approach was performed for the mesenteric arteriovenous malformation. The ileal vein, which was the dominant outflow vein, was embolized, and the blood flow in the arteriovenous malformation disappeared. A decrease in portal pressure of 29% was confirmed. There were no complications from the embolization. In cases of mesenteric arteriovenous malformations that contribute to portal hypertension, treatment of the malformations can be expected to decrease portal pressure. Compared with surgical intestinal resection, endovascular treatment that can be done with low invasiveness is thought to be a possible option.
Introduction
Arteriovenous malformations (AVMs) occur most frequently in the head and neck region, followed by the limbs, trunk, and viscera [ ]. In the intestinal tract, they are considered to occur most frequently in the cecum and right colon, with development in the ileum accounting for 5.5% of cases [ ]. A mesenteric AVM sometimes produces portal hypertension (PH), and PH is reportedly seen in 50% of congenital inferior mesenteric arteriovenous fistulae [ ].
A case in which portal pressure was decreased by percutaneous transhepatic vascular embolization of an idiopathic mesenteric AVM thought to have contributed to PH is reported.
Case
A 66-year-old man presented with a chief complaint of fatigue. His medical history included fatty liver, hypertension, hyperuricemia, and chronic gastritis. Blood tests showed hepatic dysfunction, and a more detailed workup was performed. He regularly consumed about 100-180 g per day of alcohol.
No abnormalities were seen on physical examination. The results of blood tests are shown in Table 1 . He tested negative for hepatitis B, hepatitis C virus, and antinuclear and antimitochondrial antibodies.
| Test items | Results | Units |
|---|---|---|
| White blood cell | 7030 | /μL |
| Hemoglobin | 16.2 | g/dL |
| Platelets | 141,000 | /μL |
| PT activity | 92.1 | % |
| PT-INR | 1.04 | |
| Aspartate aminotransferase | 55 | U/L |
| Alanine aminotransferase | 58 | U/L |
| γ-glutamyl transpeptidase | 357 | U/L |
| Total bilirubin | 1.6 | mg/dL |
| Albumin | 4.1 | g/dL |
| Triglycerides | 142 | mg/dL |
| Low-density lipoprotein cholesterol | 141 | mg/dL |
| Sodium | 139 | mEq/L |
| Pottassium | 4.4 | mEq/L |
| Chloride | 105 | mEq/L |
| Iron | 156 | μg/dL |
| Copper | 112 | μg/dL |
| Creatinine | 0.78 | mg/dL |
| C-reactive protein | 0.32 | mg/dL |
On abdominal ultrasound, coarsened echotexture, surface nodularity, and hypertrophy of the caudate and lateral segment with volume loss of the right lobe were seen in the liver, suggesting cirrhosis. Splenomegaly was also seen. There was no ascites.
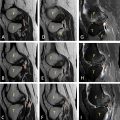
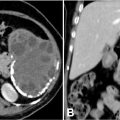
On abdominal contrast-enhanced computed tomography (CT; Incisive CT, Philips Japan, Tokyo, Japan), blunting of the liver edge and splenomegaly were confirmed. An anastomosis of the ileal artery and ileal vein via a nidus within the mesentery was also identified ( Fig. 1 A). In the early phase of contrast-enhanced CT, there was contrast enhancement in the ileal vein at the same level as the artery ( Fig. 1 B). A mesenteric AVM was diagnosed based on these findings.